Long Agonist protocol
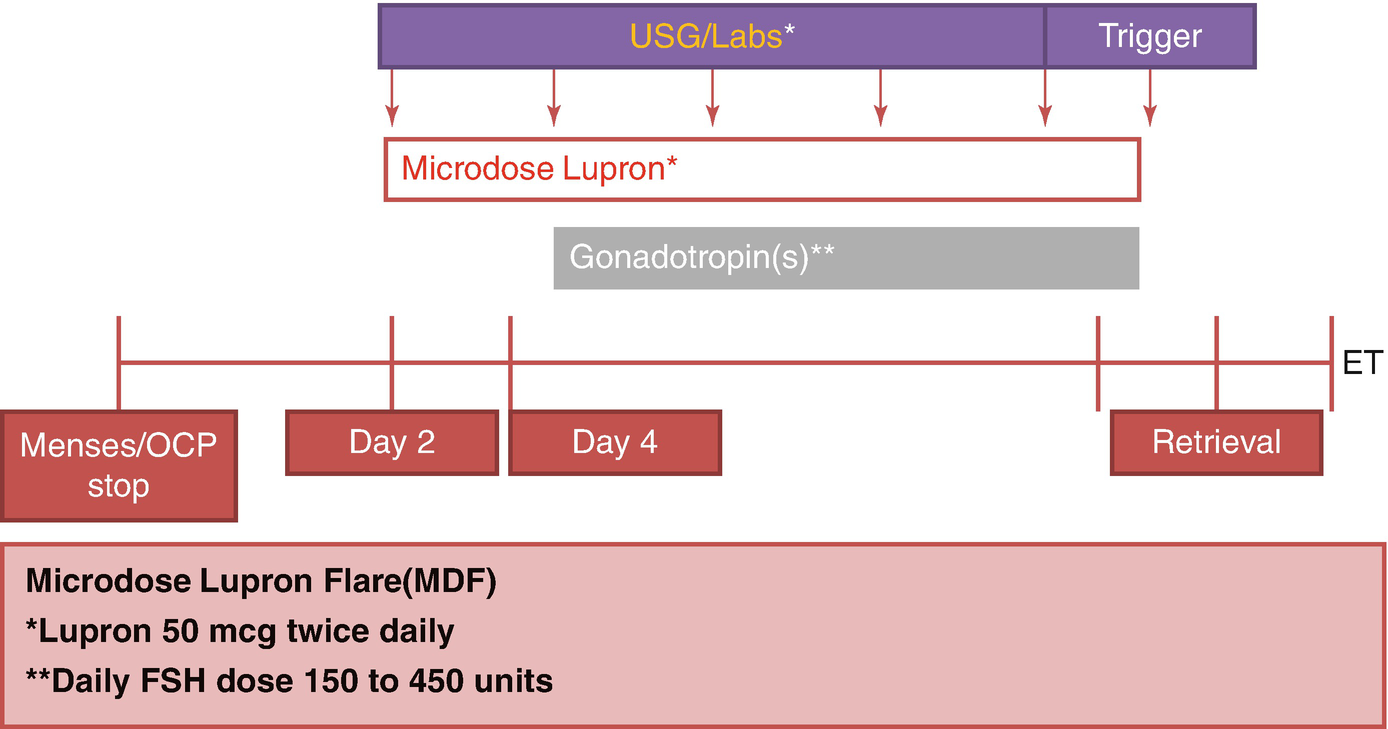
Microdose lupron flare protocol (MDF)
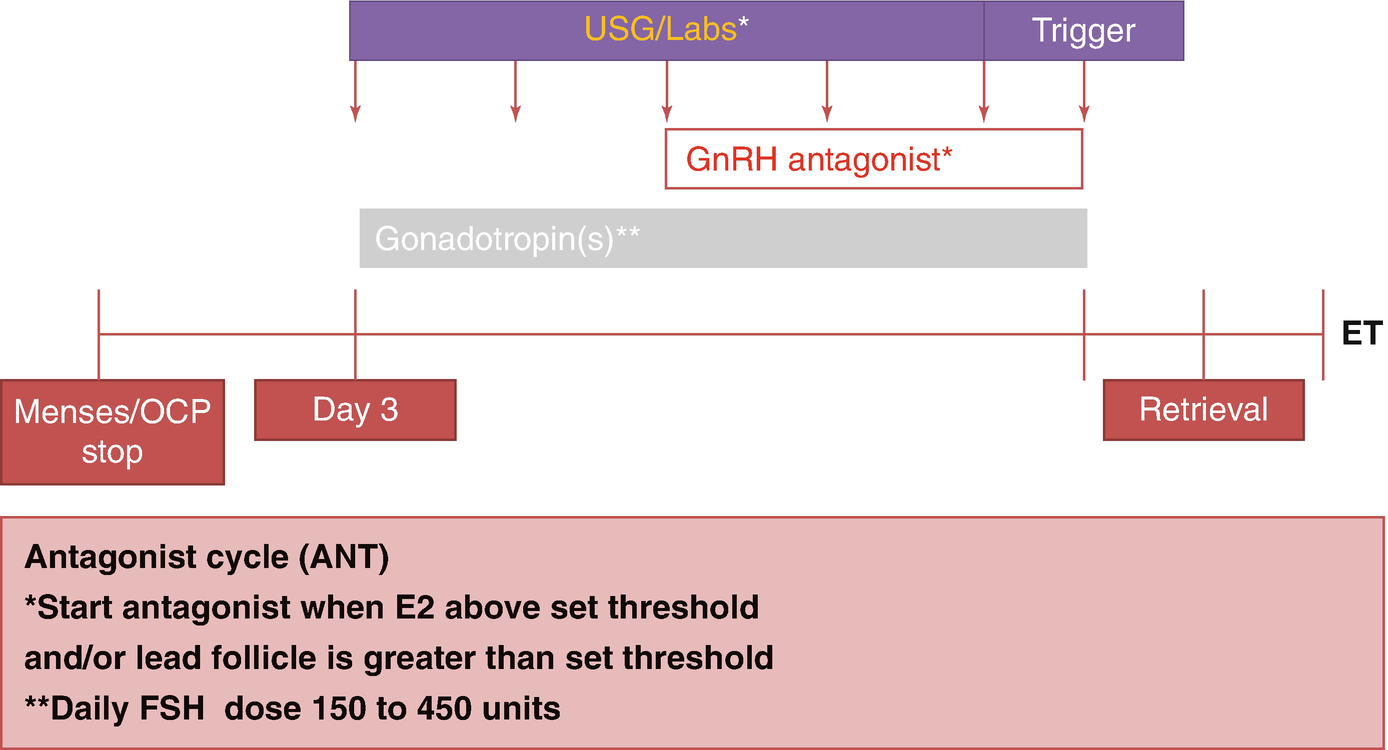
Antagonist Cycle (ANT)
In the following text, the various factors within an individual protocol that can affect cycle response in patients with POR will be reviewed such as FSH dose, use of augmentation agents growth hormone (GH), dehydroepiandrosterone (DHEA) and testosterone, dual trigger, follicular flushing, freezing all the embryos for later transfer, progesterone supplementation, conversion to IUI as a strategy, comparison of the conventional protocols against each other, followed finally by comparison of the conventional protocols with newer protocols.
8.2.1 Dose of Gonadotropins
A randomized controlled trial (RCT) of 308 patients used AMH levels to individualize the FSH dosing for patients using the LA protocol. In fact, the study showed that cycles using AMH to dose were more likely to yield <5 oocytes compared to the other arm (25.7% vs 11%) [17].
A systematic review including seven RCTs concluded that more trials are needed to prove or disprove a benefit for individualized dosing of FSH in women with POR [18].
A recent Cochrane Review included 20 trials and concluded that lack of blinding, severe heterogeneity of the trials, and poor-to-moderate quality of the studies hampered firm conclusions, but dosing differences were unlikely to be of clinical benefit in increasing the live birth in women with POR [19].
On the contrary, a retrospective review of 1394 treatment cycles concluded that increasing the daily dose of FSH to >450 units is unlikely to be of benefit and is more likely to do harm [20]. A similar conclusion was arrived at by two other sets of investigators using MDF protocol and comparing 450 units with 600 units of FSH daily [21, 22].
8.2.2 Augmentation Agents
8.2.2.1 Growth Hormone
Many studies have been published regarding the use of GH to improve pregnancy rate in POR as also discussed extensively in Chap. 5. Almost all of them have study design problems including insufficient numbers and inconsistent definition of POR. A few studies are worth reviewing; however, and not surprisingly, they provide conflicting results. An open randomized trial using LA protocol included 240 women who fit the Bologna criteria. There was no difference in the live birth rate between the two groups [23]. In contrast, a meta-analysis of 16 eligible studies, including 663 patients, showed a significant difference in live birth rate (RR 1.73) with use of GH [24]. In direct contrast, a meta-analysis of 6 RCTs and 5 controlled clinical trials including 3788 patients concluded that there was no difference in pregnancy rates [25].
Another open-label, randomized trial included 287 patients and randomized them to 3 arms comparing the 3 conventional stimulation protocols with augmentation using GH. There was no statistically significant difference in pregnancy rates between the three groups [26].
8.2.2.2 Testosterone
Studies using testosterone as an adjuvant in POR patients are beset with the same problems as other studies in POR also echoed in Chap. 5. There are many studies proving a lack of efficacy as there are showing benefit [27–29]. A meta-analysis of 3 RCTs with 221 subjects showed a twofold increase in LBR (RR 2.01). The duration of treatment with testosterone may hold the key to success according to one study that compared different duration of exposure to testosterone ranging from 2 weeks to 4 weeks. The maximum benefit was seen in women who had used testosterone for at least 4 weeks [28].
8.2.2.3 DHEA
DHEA has probably been studied the most as an adjuvant agent for patients with POR and almost all studies are small with heterogeneity in the study population. As is the case with other adjuvants, many studies seem to show a benefit, and a similar number of studies don’t show any benefit. Nevertheless, a 2015 Cochrane Review included 17 RCT with 1496 subjects and concluded that pretreatment with DHEA or testosterone may improve the live birth rates in poor responder patients [30].
8.2.2.4 Double Trigger
The idea behind the double trigger is to ensure ovulation by giving the injection at staggered times before the retrieval (GnRHa at 40 hours and hCG at 34 hours prior to retrieval) [31]. In a small pilot study, double trigger was compared with GnRHa alone or hCG alone. A higher number of top-quality embryos were noticed in the double-trigger arm compared with the other two arms. More studies are needed to confirm if this translated into more live births [32].
8.2.3 Follicular Flushing with Conventional Stimulation
Follicular flushing has been advocated as a strategy in normal responders and proven to be ineffective [33]. Each follicle is flushed three times with 2 mL of culture medium using a double lumen needle [34]. In the first RCT in POR patients, 50 women were randomized to have direct aspiration or follicular flushing. The average number of oocytes retrieved was four in the direct aspiration group and three in the follicular flushing group. Significantly, a lower pregnancy rate of 4 vs 36% was observed [33]. In another RCT, 80 patients were randomized, and similar live birth rates (25 vs 22.5%) were observed [34]. Similarly, another RCT recruited 80 patients and did not show any difference between the 2 groups for birth rate. Both the above trials showed a significant doubling of procedure time, however [35].
8.2.4 Freezing All Embryos After Conventional Stimulation
The optimal embryo transfer (ET) strategy was studied retrospectively in 2263 women undergoing IVF; 879 women fit the criteria for POR, and 645 had day 2 or cleavage stage transfer while remaining 234 had blastocyst transfer. Of the latter group, 59 had fresh transfer, and 87 had frozen embryo transfer. The cycle cancellation was lowest in the women who had day 2 or cleavage stage transfers, but the live birth rate per ET (LBR/ET) was also the lowest. Whereas the former group had an LBR/ET of 21.5%, the blastocyst transfer group had an LBR/ET of 41.1%. Among those, the LBR/ET was 30.5% and 40.2% for fresh transfer and frozen transfers (FET), respectively [36].
Another retrospective study reviewed 433 women with POR. Two hundred and seventy-seven women underwent fresh transfer, and 156 had FET. The clinical pregnancy rate was not different between the two groups (14.1 vs 13.7%) [37]. Another retrospective study included 559 patients with POR and failed to show a significant difference between the fresh transfer and FET groups [38].
8.2.5 Conversion to Intrauterine Insemination
A multicenter retrospective study looked into the strategy of cycle cancellation vs intrauterine insemination (IUI vs IVF) when two or less follicles were recruited during COS. Of the 461 cycles that met the criteria, 136 were cancelled, 141 were converted to IUI, and 184 completed IVF. LBR was significantly higher (11.6 vs 1.6%) in the IVF group regardless of the age of the patient and was even more significant in women aged <40 (13.1 vs 2%) [39]. More studies are needed to confirm that even in women with only one or two follicles, it is worthwhile to continue with IVF rather than cycle cancellation or converting to IUI.
8.3 Comparison of the Three Conventional Stimulation Protocols
The three conventional stimulation protocols were compared in an RCT involving 111 women with POR. The duration of stimulation and the total dose of gonadotropins used were significantly greater with the LA protocol compared to the other two protocols. The ongoing pregnancy rate was highest (16.2%) with the ANT protocol, and the other two protocols had an ongoing pregnancy rate of 8.1% [40].
In contrast, another RCT showed an entirely different outcome. The researchers allocated 330 women between ANT protocol (168 women) and LA protocol (162 women). The cycle cancellation rate was higher in the ANT group compared to the LA group but was not statistically significant (22.15 vs 15.2%). The clinical pregnancy rate per transfer was also not significant (42.3 vs 33.1%). However, when the cycle cancellation rates were considered, the clinical pregnancy rate per cycle initiated was significantly lower in the ANT group compared to the LA group (25.6 vs 35.8%) [41].
Interestingly, 2 years before the publication of the above trials, a meta-analysis of 14 studies involving 566 patients in ANT protocol and 561 patients in LA protocol was performed. This showed a shorter duration of stimulation in the ANT group as the only significant difference between the two groups. There was no difference in cycle cancellation rate or the clinical pregnancy rates [42]. Taken together, it is likely that there is no significant difference in pregnancy rates between the three protocols.
8.4 Comparison of the Conventional Protocols with Newer Protocols
8.4.1 Mild Stimulation
Multiple studies have been published on using mild stimulation of ovaries for IVF in POR patients compared to conventional protocols that traditionally use high or very high doses of gonadotropins. The common features of many of the protocols described under this category are use of clomiphene citrate, aromatase inhibitors, and low-dose gonadotropins, as discussed in the chapter in Part II. ASRM Practice Committee recently reviewed the available studies and recommended that mild-stimulation IVF protocols be considered as primary stimulation protocols in POR patients as the pregnancy rates are similar and the cost of stimulation is lower [4].
8.4.2 Luteal Phase Estrogen Priming with Flexible Antagonist Start
This protocol was first described by Dragisic in 2005 using luteal phase estrogen followed by GnRH antagonist and gonadotropin started at the same time. The underlying principle is suppression of luteal follicle recruitment and decreasing follicular heterogeneity. In a retrospective study, 117 patients underwent estrogen priming protocol, and 69 underwent MDF protocol. Although similar number of oocytes were retrieved in both groups, the ongoing pregnancy rate was 37% in the estrogen priming group vs 25% in the MDF group which was not statistically significant [43].
In another retrospective study, 86 patients had luteal estrogen with antagonist start midway through stimulation compared with 69 patients who had ANT protocol for COS. The ongoing pregnancy rates were 27.1 vs 20% which did not reach statistical significance [44].
8.4.3 Delayed Start
Delayed start with GnRH antagonist protocol for young POR patients was first described in 2014 [45]. The modification in delayed-start protocol compared to estrogen priming with flexible antagonist start protocol is that estrogen priming is followed by 7 days of GnRH antagonist treatment before starting ovarian stimulation with gonadotropins.
One hundred women were randomly assigned to receive the delayed-start protocol or the MDF protocol. There was no significant difference between clinical or ongoing pregnancy rate between the two groups [46]. Similarly, another smaller RCT with 54 patients did not show any difference in any of the measured outcomes including pregnancy rate [47].
8.5 Conclusion
Conventional IVF stimulation protocols are likely equally effective and better than IUI for patients with POR. There is no consensus on one specific conventional IVF stimulation protocol for patients with POR. However, mild-stimulation IVF may be more cost-effective and may at least result in similar outcome as using conventional IVF protocols with fresh embryo transfers. More detailed discussions on mild approaches for COS are extensively discussed in the upcoming chapters.

Full access? Get Clinical Tree


