Types of COC
Containing Ethinyloestradiol:
Most are monophasic pills, delivering the same dose of oestrogen and progestogen every day. The content of the synthetic oestrogen ethinyloestradiol ranges from 20 to 40 µg, with ‘standard-dose’ pills containing 30–40 µg and ‘low dose’ pills 20 µg. The usual preparations of choice are the 30 or 35 µg pills (e.g. Microgynon 30). Oral contraceptives are also grouped in four ‘generations’, depending on the dose of ethinyloestradiol used and type of progestogen. Bleeding patterns are determined more by the type of progestogen used rather than the oestrogen dose or the type of phasic regimen.
Containing Oestradiol Valerate:
This natural oestrogen is now combined with a synthetic progestogen, dienogest, as Qlaira. There are four phases of oestrogen and progestogen dose over 26 days followed by 2 pill-free days. Qlaira has advantages, with reduced changes in lipid profiles and haemostatic variables, and with only 2 pill-free days, may minimize menstrual migraines and mood swings associated with oestrogen withdrawal. Long-term data are limited: risks are assumed to be similar to the other COCs.
Contraceptive Efficacy
Taken properly, combined hormonal contraception is highly effective, with a failure rate of 0.2 per 100 woman years. If less care is taken, failure rates are much higher. The low-dose COC preparations containing 20 µg ethinyloestradiol have similar contraceptive efficacy to ‘standard’ 30–35 µg pills (Cochrane 2011 CD003989).
Common Side Effects of Sex Hormones
| Progestogenic | Oestrogenic |
| Depression | Nausea |
| Postmenstrual tension-like symptoms | Headaches |
| Increased mucus | |
| Bleeding; amenorrhoea | Fluid retention and weight gain |
| Acne | Occasionally hypertension |
| Breast discomfort | Breast tenderness and fullness |
| Weight gain | Bleeding |
| Reduced libido |
Indications
All women without major contraindications may use combined hormonal contraception (‘from menarche to menopause’). It is suitable for the teenager (in conjunction with condoms) and the older woman with no cardiovascular risk factors until the age of 50. It is also useful for menstrual cycle control, menorrhagia, premenstrual symptoms, dysmenorrhoea, acne/ hirsutism and prevention of recurrent simple ovarian cysts.
The COC Pill in Practice
Reduced absorption of the pill can occur if suffering from diarrhoea, vomiting or if taking some oral antibiotics. If the woman has diarrhoea she should continue taking the pills but follow the missed-pill instructions (below) for each day of the illness. If she vomits within 2 h of taking the pill she should take another or follow the rules for missed pills. If she is taking broad-spectrum antibiotics, she should continue the pills but use condoms during and for 7 days after the antibiotic course. With liver enzyme inducing drugs (e.g. anticonvulsants), the oestrogen dose may need to be increased.
The Missed Pill:
For standard-strength preparations (30–35 µg ethinyloestradiol) one or two missed pills anywhere in the pack are not a problem. For low-dose preparations (20 µg) only one pill can be missed. The forgotten pill should be taken as soon as possible and then the packet continued as normal. If more pills have been missed then continue the packet as normal but condoms should be used for 7 days. If there are less than seven pills remaining in the packet avoid a pill-free break by running straight into the next packet. Note that advice for missed pills is different and more complex for Qlaira (see product information).
The Pill and Surgery:
The pill is normally stopped 4 weeks before major surgery because of its prothrombotic risks, but the risks of pregnancy should also be considered. The pill is not discontinued prior to minor surgery.
Counselling the Woman Starting on the ‘Pill’
Advise of major complications and benefits
Advise to stop smoking
Advise to see doctor if symptoms suggestive of major complications
Advise about poor absorption with antibiotics and sickness and what to do about missed pill(s) (give leaflet)
Stress the importance of follow-up and blood pressure measurement
Disadvantages
Major: Complications
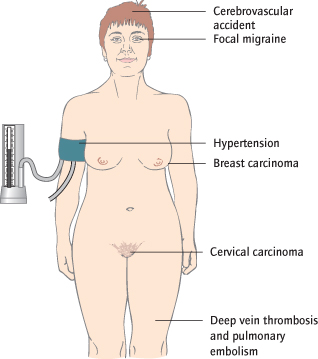
These are very rare. In general, the risks of pregnancy (including termination of an unwanted pregnancy) outweigh the risks of CHC. The estimated excess annual risk of death for women taking the pill is 2–5 per million users for women <35 years of age. This can be minimized by careful selection and follow-up of women. Venous thrombosis and myocardial infarction are the most important complications (http://www.fsrh.org.uk/). The risk is further multiplied by smoking, increased age and obesity (absolute contraindication if body mass index [BMI] >40, or age >35 years and smokes >15 cigarettes per day; relative contraindication if BMI 35–39). Venous thromboembolism is more common with ‘third-generation’ pills containing the progestogens gestodene or desogestrel than with the more widely prescribed second-generation preparations containing norithisterone or levonorgestrel, although the absolute risk remains low. Other problems include a slightly increased risk of cerebrovascular accidents, focal migraine, hypertension, jaundice, and liver, cervical and breast carcinoma (Fig. 12.2).
Minor: Side Effects
Both oestrogenic and progestogenic side effects may occur. The most common are nausea, headaches and breast tenderness. Breakthrough bleeding is common in the first few months, but has usually settled after 3 months. If not then consider changing the pill to one containing a more potent progestogen or if using a 20 µg ethinyloestradiol pill increase it to a 30 µg preparation. Lactation is partly suppressed so the pill is contraindicated during the first 6 weeks of breastfeeding.
Advantages
Contraceptive:
Despite the rare complications, CHC is a very effective and acceptable method of contraception: it has been the subject of considerable research and in appropriate women it is very safe.
Non-Contraceptive Benefits:
Useful effects include more regular, less painful and lighter menstruation. There is protection against simple ovarian cysts, benign breast cysts, fibroids and endometriosis. Hirsutism and acne may improve: CHC need not be prescribed merely for contraception. The risk of pelvic inflammatory disease (PID), but not HIV, is reduced possibly because of thicker cervical mucus. Longer term, there is reduction in the incidence of ovarian, endometrial and bowel cancer.
Contraindications to Combined Hormonal Contraception
| Absolute: | History of venous thrombosis |
| History of cerebrovascular accident, ischaemic heart disease, severe hypertension | |
| Migraine with aura | |
| Active breast/ endometrial cancer | |
| Inherited thrombophilia | |
| Pregnancy | |
| Smokers >35 years and smoking >15 cigarettes/day | |
| Body mass index (BMI) >40 | |
| Diabetes with vascular complications | |
| Active/ chronic liver disease | |
| Relative: | Smokers |
| Chronic inflammatory disease | |
| Renal impairment, diabetes | |
| Age >40 years | |
| BMI 35–40 | |
| Breastfeeding up to 6 months postpartum |
Risk of Non-Fatal Venous Thromboembolism for Users of Combined Oral Contraceptives (COCs)
| User category | Incidence per 100 000 women per year |
| All women not using ‘pill’ | 5 |
| Pregnant women | 60 |
| Women using older 30 µg ‘pill’ | 15 |
| Women using new 30 µg ‘pill’ | 25 |
| Women smoking and using ‘pill’ | 60 |
Other Combined Hormonal Contraception
These are non-oral combined preparations of oestrogen and progestogens. Safety, side effects and efficacy are similar to combined oral preparations.
Combined Transdermal Patch (Evra)
Evra is a transdermal adhesive patch that releases ethinyloestradiol (34 µg) plus the progestogen norelgestromin. A new patch is applied weekly for 3 consecutive weeks and then replaced; this is followed by a patch-free week. Efficacy, side effects and contraindications to use are similar to the COC.
Combined Vaginal Ring (Nuvaring)
The latex-free Nuvaring releases a daily dose of 15 µg of ethinyloestradiol and 120 µg of the progestogen etonogestrel to inhibit ovulation. The ring is easily inserted into the vagina by the patient and worn for 3 weeks. It is then removed to allow for a 7-day ring-free break and a withdrawal bleed. A new ring is then inserted. This may be better tolerated than the COC due to lower systemic oestrogenic side effects. It is recommended that the ring not be removed during intercourse but, if necessary, may be removed for a maximum of 3 h. When used properly, the efficacy of the ring is equivalent to the COC. It has the same metabolic and coagulation effects as other combined hormonal methods (Contraception 2011; 83: 107–15).
Counselling Before Using the ‘Mini Pill’
Advise woman about bleeding patterns
Emphasize the importance of meticulous timekeeping
Progestogen-Only Pill (POP)
The standard progestogen-only pill
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree