Fig. 1
(a–c): Examples of the spectrum of clinical presentation of constriction bands. (a) Constriction bands causing hourglass deformity at the base of the fingers. (b) Deeper bands on the central digits with distal deformity; the thumb and small finger are not affected. (c) Acrosyndactyly with phalangeal reduction of the long, ring, and small fingers. The index finger has a prominent band at the base, and the thumb is not involved (Courtesy of Shriners Hospitals for Children, Houston)
Etiology
CBS represents a separate category in the Swanson/International Federation of Societies for Surgery of the Hand (IFSSH) classification for congenital hand differences (Swanson 1976; De Smet 2002). The etiology still remains controversial, a fact reflected in the plethora of terminology for this condition: amniotic band syndrome , constriction ring syndrome, Streeter’s dysplasia, Simonart’s bands, annular groove, amniotic band disruption complex, limb body wall complex, ADAM (amniotic deformity, adhesions, mutilations), and amnion rupture sequence. The difficulty lies in finding a single mechanism that accounts for the disparate anomalies associated with CBS in up to 70 % of cases. These anomalies include clubfoot deformity, leg length discrepancy, cleft lip, cleft palate, and visceral and body wall defects (Moses et al. 1979; Foulkes and Reinker 1994). Aberrant embryonic morphogenesis (intrinsic theory), fetal vascular compromise, and mechanical deformation of normally developed structures (extrinsic theory) have all been proposed.
The intrinsic theory was first suggested by Streeter, who felt that there was a primary mesodermal defect resulting in malformations during embryogenesis (Streeter 1930). Others have supported the concept that the abnormal tissue at the site of constrictions represents abnormal distribution of apoptosis, or programmed cell death, a normal embryological process (McKenzie 1975). Mild constriction bands look like naturally occurring skin creases, but in abnormal locations (Moran et al. 2007). A second theory for the etiology of CBS is that of vascular disruption or hemorrhage within the limb bud mesenchymal tissues after the condensation of the digital rays, from either intrinsic or extrinsic forces (Van Allen 1981; Halder 2010). Kino supported this theory with an experimental animal model (Kino 1975). Lockwood added to the idea of a teratogenic event causing a malformation based on studies of monozygotic twins with CBS (Lockwood et al. 1989).
The currently best-accepted theory, proposed by Torpin in 1965, states that the constrictions are a result of extrinsic forces and events causing deformation of a normally developing fetus (Torpin 1965). Through the first trimester of pregnancy, the fetal membranes have two distinct layers, the chorion and the amnion. The extrinsic theory states that a partial rupture of the inner amnion prior to the fusion of the two layers results in fibrous chorionic bands that can encircle and trap some part of the fetus. The gestational age at which the amniotic rupture occurs is thought to be critical in determining the severity of the resulting deformation. Rupture before 45 days’ gestation can lead to central anomalies, CNS malformations, and truncal defects, because during the 5th week skeletal elements develop from mesodermal condensations appearing along the long axis of the limb bud (Higginbottom et al. 1979). Later rupture is more likely to affect the limbs. Later, as the fetus grows but the bands do not, the bands become constricting, resulting in distal deformation, acrosyndactyly, vascular or neural compromise, or complete limb or digital reduction. If the amniotic bands are swallowed while still partially attached to the chorion, the tether may lead to bizarre facial clefts and palate deficiencies that are not along the embryological planes of facial closure (Bouguila et al. 2007). A possible explanation for the non-band-related effects of a partial amniotic rupture is a transient oligohydramnios from extravasation of amniotic fluid. Until the chorion adjusts its permeability, the developing fetus has restricted space, resulting in compressive deformation forces. This may contribute to the severity of clubfeet deformities seen with CBS (Allington et al. 1995; Gomez 1996) (Fig. 2a, b).


Fig. 2
(a) Clinical photograph of an infant with a deep constriction band with distal edema and clubfoot deformity. The other leg has a milder clubfoot deformity without constriction bands. (b) The affected leg 9 months post band excision. The lymphedema has significantly improved; treatment for the clubfoot deformity is ongoing (Courtesy of Shriners Hospitals for Children, Houston)
Diagnosis
CBS is present at birth and is diagnosed based on clinical features and appearance. There is a predilection for the distal segments of the limbs, with the hand and fingers involved up to 80 % of the time (Tada et al. 1984). In a study of 364 patients with constriction bands, 64 % of the bands were located in the upper limb; of those, 2 % were on the arm, 7 % on the forearm, and 55 % in the hand. The lower limb bands were similarly concentrated in the distal part (Flatt 1977). The central digits are most commonly involved. The thumb is least affected, likely due to its in-palm fetal position, where it is relatively protected by the fingers (Light and Ogden 1993; Foulkes and Reinker 1994). The clinical presentation can have any variation along a spectrum that includes mild hourglass-type circumferential indentation in the skin, deep circumferential cleft, distal deformity such as lymphedema, distal acrosyndactyly, and complete digit or limb reduction (Fig. 1a–c). Moderate to severe constriction bands cause fibrous scar formation that can lead to distal vascular, lymphatic, and neural impairment. Temperature gradients have been measured across constricting bands due to vascular insufficiency across the band (Flatt 1977). Initially mild distal symptoms may progress as the child grows. When the bands are at the level of the digits, nail deformity is often present (Moses et al. 1979). With bands proximal to the wrist crease, neuropraxia or more severe nerve injury can result. A study on 45 patients with CBS found that 23 % had sensory deficits (Moses et al. 1979). Of note, every patient with a sensory deficit in that series also had a notable temperature gradient (average 2.4° Celsius) at the site of the constriction ring . Multiple cases of mild to substantial ulnar, median, and radial nerve compression have been reported (Weeks 1982; Tada et al. 1984; Uchida and Sugioka 1991; Light and Ogden 1993; Weinzweig and Barr 1994; Jones et al. 2001; Beidas et al. 2010). A careful neurological exam is mandatory, albeit it is difficult to perform in young children. Sensory and even mild motor disturbances are challenging to diagnose in infants and are probably underreported. It is helpful to look for subtle signs or abnormal resting posture, such as an intrinsic minus position and inability to extend the finger interphalangeal joints, denoting an ulnar nerve palsy, or wrist drop with inability to extend the metacarpophalangeal joints, denoting a radial nerve lesion. Depending on the timing of the onset of band formation in utero, nerve compression may already have been present for a considerable number of months on a child’s first day of life. Jones reported on a case where a deep constriction band causing ulnar nerve compression was noted on an 18-week ultrasound. That meant that when the infant was born at term, the ulnar nerve palsy had actually been present for 5.5 months (Jones et al. 2001). Early recognition of nerve dysfunction associated with constriction bands is extremely important. Careful preoperative assessment will guide subsequent reconstruction.
CBS should be distinguished from symbrachydactyly and transverse deficiency. Symbrachydactyly is typically unilateral and affects the entire hand. The hand is small, yet the distal phalanges have formed fingernails, as ectodermal development progresses despite mesodermal disruption (Moran et al. 2007). Symbrachydactyly may occur with Poland’s sequence and other conditions of vascular insufficiency (Ogino and Saitou 1987). The presence of bands on multiple other sites in an asymmetric pattern distinguishes CBS. Single digits can be affected in isolation in CBS, and even when the digits appear normal distal to a phalangeal band, the nails are often absent or abnormal. The acrosyndactyly seen in CBS is different from a complex syndactyly resulting from failure of differentiation. In CBS, it is felt that normal digital separation via apoptosis has already occurred when an abnormal force results in distal fusion. This is supported by the findings of epithelialized patent sinus tracts between digits, lack of bony fusion, and the involvement of nonadjacent digits as well as adjacent ones (Fig. 3).
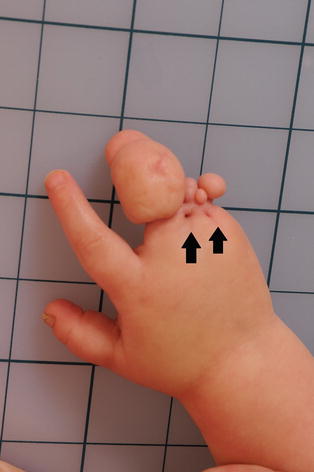
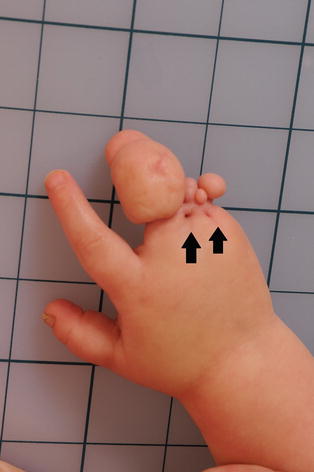
Fig. 3
Clinical photograph of a constriction band causing acrosyndactyly. Black arrows show epithelialized sinus tracts between the syndactylized fingers (Courtesy of Shriners Hospitals for Children, Houston)
Transverse limb deficiency, a failure of formation, is also typically unilateral, with the proximal forearm being the most commonly affected site, as opposed to the fingers in CBS. The proximal limb is abnormal. Transverse deficiencies in the digits often take the form of disarticulations with distal soft tissue pockets, while constriction band reductions occur at the level of the phalangeal midshaft with tapering bone stumps (Ogino and Saitou 1987; Kallemeier et al. 2007) (Fig. 4a, b). Both symbrachydactyly and transverse deficiencies can have terminal structures such as nubbins, rudimentary finger nails, clefts, and pits (which represent anomalous muscle attachments to the skin) (Kallemeier et al. 2007) (Fig. 5a, b). In CBS severe enough to result in an intrauterine amputation , no such distal structures are present at all. While symbrachydactyly and transverse limb deficiency are currently classified as different entities, it is likely they represent different points along a single continuum (Kallemeier et al. 2007), distinct from CBS.
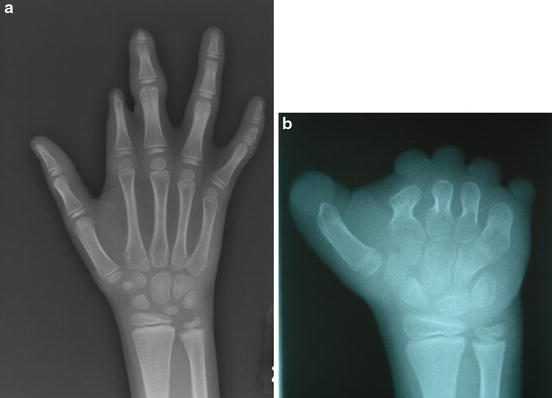
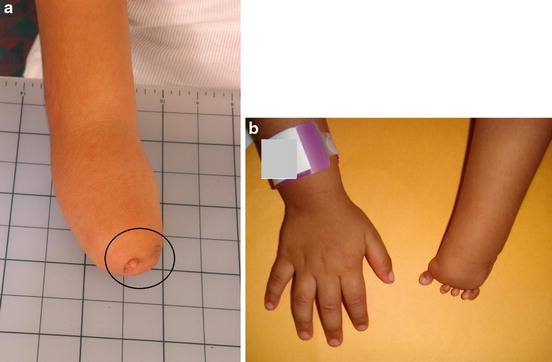
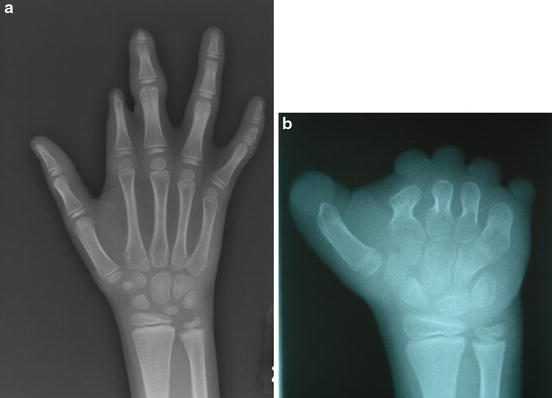
Fig. 4
(a, b): Radiographic comparison between adactyly due to constriction band syndrome and failure of formation. (a) CBS. The digital reduction occurs at the mid-phalanx level, with tapered distal bone segment and no nubbins or excess soft tissue distally. Note also that only the index and long fingers are affected. (b) Failure of formation. The digital reduction occurs at the MP joint level, with metacarpal dysplasia and distal soft fleshy skin nubbins. Note that the entire hand is uniformly affected (Courtesy of Shriners Hospitals for Children, Houston)
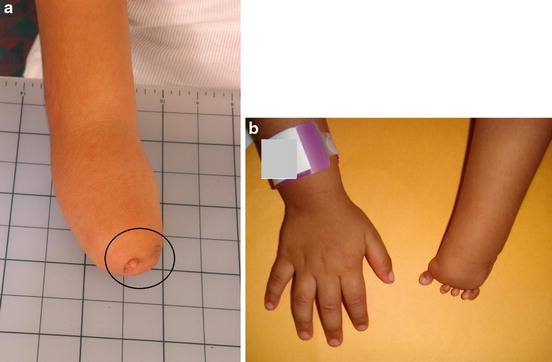
Fig. 5
(a, b): Examples of transverse limb deficiencies with rudimentary nubbins and clefts (Courtesy of Shriners Hospitals for Children, Houston)
Relevant Anatomy
The anatomy relevant to surgery depends on the area of the body affected by the constriction bands. Most bands are superficial, and only the skin and subcutaneous tissue are involved. It is important to note that the neurovascular bundle may be displaced superiorly near areas of banding. Severe constriction bands can cause neurovascular and lymphatic compromise that distorts the anatomy distal to the constriction point.
It is a hallmark of CBS that the anatomical structures proximal to the constriction band are completely normal. This is true of limb reductions resulting from CBS as well, highlighting the importance of differentiating an intrauterine amputation from CBS from congenital limb deficiency. The reliable presence of normal proximal anatomy is an extremely important point for surgical planning. But is the proximal anatomy truly completely normal? Recent studies have scrutinized this anatomy more closely. Satake et al. noted metacarpal hypoplasia in 30 % of hands with constriction band amputations at the mid proximal phalanx level (Satake et al. 2012). A small study of upper and lower limb vascular anatomy in CBS found an incidence of proximal vascular abnormality ranging from 100 % in deep bands and limb reductions to 11 % in superficial bands (Daya and Makakole 2011).
Imaging
With advancements of ultrasound technology, constriction bands, limb deformations, and many skeletal anomalies can be visualized as early as the start of the second trimester. Prenatal diagnosis of atypical facial clefting should alert clinicians to the possibility of CBS, which can help in prenatal counseling and family preparation. Limb-threatening constriction bands can be diagnosed and theoretically treated, prior to progression to intrauterine amputation (Soldado et al. 2009). Doppler ultrasound has demonstrated restoration of blood flow to a threatened limb after fetal intervention (Moran et al. 2007). However, intrauterine surgery is not without risks to fetus and mom. Postnatally, plain radiographs of the affected hand are helpful in preoperative planning when acrosyndactyly is present; otherwise, imaging is not routinely utilized.
Classification
Given the wide variation of clinical presentation where no two patients will have the exact same pattern, number, or severity of constriction bands, CBS is difficult to classify. While multiple classification systems have been proposed, none have been universally adopted. The two most helpful classifications are descriptive – one is based on the depth of band involvement, and the other is based on the severity of the deformity distal to the band.
Isacsohn divided constriction bands into five groups depending upon the depth of band involvement (Isacsohn et al. 1976). In group 1, the band is a shallow groove in the skin; in group 2 the band involves the subcutaneous tissue and muscle; in group 3 the band extends to bone; in group 4 there is bony pseudarthrosis; and in group 5 an intrauterine amputation occurred. This classification highlights the fact that increasing depth of band involvement results in increasing severity of distal lymphatic, vascular, and neural compromise.
The most widely quoted classification system is the Patterson classification, which is based on the pattern of deformity distal to the constriction band (Patterson 1961) (Table 1).
Table 1
Patterson classification for constriction bands
Group 1 | Simple constriction rings | |
Group 2 | Constriction rings with distal deformity and/or lymphedema | |
Group 3 | Constriction ring with acrosyndactyly | |
I | Distal fusion with well-formed web spaces | |
II | Distal fusion with incomplete web space formation | |
III | Distal fusion with sinus tract between digits; no web space | |
Group 4 | Intrauterine amputation | |
Treatment Options
Nonoperative Management
Nonoperative management is appropriate for the two ends of the constriction band spectrum – the very mildly affected and the limb or digital amputations. Superficial bands without lymphedema or neurological compromise require no operative treatment. The prognosis for isolated superficial extremity bands is excellent with no functional deficits, although there can be aesthetic concerns. For patients with digital amputations, careful assessment of their hand function is required. If the function of the hand is acceptable, no treatment is needed (Wiedrich 1998; Kawamura and Chung 2009). It is better to adapt tools and equipment to fit the child’s needs than to undertake complex reconstruction that cannot result in a normal hand and will still require adaptive equipment (Fig. 6a, b).


Fig. 6
(a, b): Example of modification of sports equipment. (a) The patient’s fingers are too short to keep a standard baseball glove from falling off his non-dominant left hand when he catches a ball. (b) The volar wrist component, stitched into the glove, provides an alternative mechanism of support to keep the glove on his hand while catching a ball (Courtesy of Shriners Hospitals for Children, Houston)
Operative Treatment
Indications
Acute vascular compromise, severe lymphedema, and distal nerve compression are definite indications for surgical intervention. The presence of an acrosyndactyly prompts reconstruction for functional improvement as well as for the prevention of deformity with subsequent digital growth. Mild to moderate bands that were initially asymptomatic should be reevaluated for surgical intervention if there is a change, such as onset of cold intolerance or deformity with growth. The desire for a more aesthetic contour to the limb or digit is a valid indication to excise a constricting band (Fig. 7a, b); however, purely aesthetic excision should be avoided if there is a tendency for hypertrophic scar formation. Complex reconstruction should be avoided if no clear functional benefit can be expected.
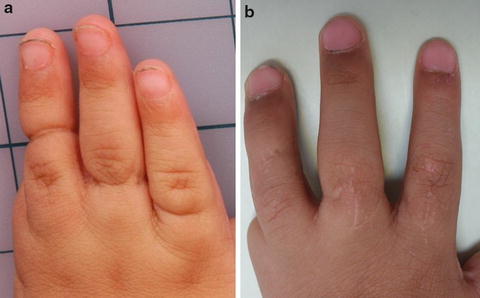
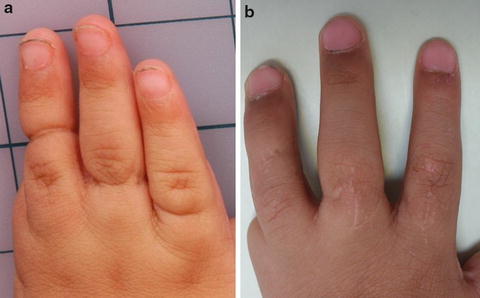
Fig. 7
(a, b): Preoperative (a) and postoperative (b) views of asymptomatic constriction bands treated electively to improve the contour of the fingers (Courtesy of Shriners Hospitals for Children, Houston)
Timing of Surgical Intervention
In the rare cases where an infant is born with constriction bands causing acute vascular compromise or severe distal edema, the bands should be released within the first hours or days of life as a limb-sparing procedure (Fig. 8). Nerve and distal soft tissue reconstruction is performed in a subsequent second stage. In the majority of cases, the limb is adequately perfused and the timing of constriction band excision is determined by the depth of the band and the severity of distal deformity. The presence of distal lymphedema signals venous or lymphatic obstruction, or both. These bands should be excised within the first 3 months of life to allow for resolution of the edema and prevent secondary fibrosis. Clinical evidence of nerve dysfunction should also prompt intervention as early as possible, preferably within the first 3 months of life. Depending on the onset of the limb constriction in utero, nerve compression could already be of several weeks’ or months’ duration on the day of birth, which increases the urgency of band excision to release nerve compression. If acrosyndactyly is present, reconstructive surgery is recommended between 6 months and 1 year of age to allow for untethered normal longitudinal bone growth. When the constriction is minor and the surgical goals purely aesthetic, the procedure may be performed at any age. In these elective cases, many surgeons choose to wait until the child is several years of age and their baby fat has dispersed. If a child has other conditions that also require treatment within a certain time frame, such as cleft lip or palate or clubfeet, it is imperative to communicate with the other surgeons regarding the timing of surgeries. If possible, procedures should be scheduled so as to maximize treatment during each anesthetic exposure.


Fig. 8




Infant with a deep constriction band around the proximal left arm. The band was urgently incised shortly after birth as a successful limb-sparing procedure. In subsequent staged procedures, the band was fully excised and nerve grafting performed. The lymphedema resolved and protective sensation to the hand was achieved, but there remains minimal motor function of the wrist and hand. Note the presence of bilateral clubfeet (undergoing casting) (Courtesy of Shriners Hospitals for Children, Houston)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


