Consolidation
Daniel J. Podberesky, MD
DIFFERENTIAL DIAGNOSIS
Common
Infectious Pneumonia
Aspiration Pneumonia
Pulmonary Edema
Atelectasis
Less Common
Pulmonary Contusion
Pulmonary Hemorrhage
Pulmonary Infarct
Lymphoma
Rare but Important
Radiation Pneumonitis
Hydrocarbon Aspiration
Hypersensitivity Pneumonitis
Pulmonary Alveolar Proteinosis
Bronchiolitis Obliterans with Organizing Pneumonia
Lymphoid Hyperplasia
Near-Drowning
Pulmonary Inflammatory Pseudotumor
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Blood, pus, protein, water, cells
History extremely helpful
Helpful Clues for Common Diagnoses
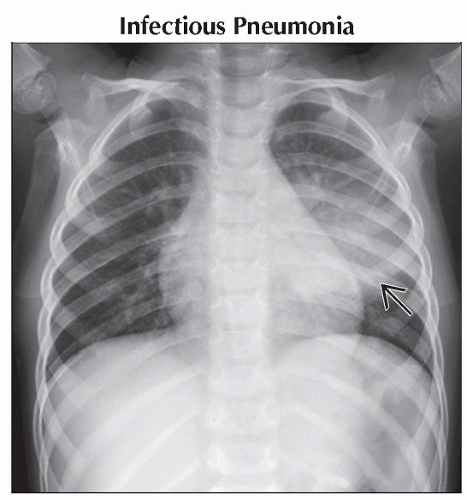
Infectious Pneumonia
Lung consolidation ± air bronchograms
Not associated with volume loss
± associated parapneumonic effusion
Round pneumonia
Young children
Poorly developed collateral airway pathways
Aspiration Pneumonia
Typically oral or gastric contents
Chemical pneumonitis, which can be superinfected
When upright, right lower lobe most frequent
When supine, posterior segments of upper lobes and superior segments of lower lobes most frequent
Pulmonary Edema
Transudative fluid collecting in lung tissue
May result from
Increased hydrostatic gradient
Low oncotic pressure
Increased capillary permeability
Interstitial edema may progress to alveolar edema and consolidation
Pleural effusions
Cardiogenic vs. noncardiogenic (e.g., neurogenic, renal or hepatic disorders, toxins)
Atelectasis
Airspace collapse resulting in increased lung density
Volume loss
Elevation of diaphragm
Cardiomediastinal shift
Shift of fissures
Crowding of vessels
Can be lobar, segmental, subsegmental, or plate-like
Frequently seen in inpatient settings, viral respiratory infections, and asthmatic patients
Helpful Clues for Less Common Diagnoses
Pulmonary Contusion
Edema and hemorrhage collecting in area of lung trauma
Typically evolve on radiography over 24-48 hours
Typically resolve in 3-5 days
Look for other signs of trauma
Pneumothorax, mediastinal injury, fractures, pleural fluid
Pulmonary Hemorrhage
Can be indistinguishable from other sources of consolidation on radiograph
May resolve fairly rapidly
Common causes in children include
Infection
Cystic fibrosis
Immunologic disorders (e.g., Goodpasture syndrome)
Wegener granulomatosis
Trauma
Pulmonary Infarct
Usually result of pulmonary embolus
Peripheral, wedge-shaped consolidation
Hampton hump: Pleural-based, peripheral, wedge-shaped consolidation secondary to pulmonary embolus
Lymphoma
Helpful Clues for Rare Diagnoses
Radiation Pneumonitis
Typically requires at least 4500 rads
Acute
1-8 weeks after radiation
Patchy consolidation confined to radiation portal
Chronic
9-12 months after radiation and beyond
Consolidation and fibrosis/scarring
Bronchiectasis
Hydrocarbon Aspiration
Gasoline, kerosene, lighter fluid
Severe chemical pneumonitis
Patchy consolidation develops over several hours
Edema
Hypersensitivity Pneumonitis
a.k.a. extrinsic allergic alveolitis
Type 3 immune response to environmental antigen
Moldy hay, dust, pigeon droppings
Reticulonodular opacities typically seen on x-ray
Consolidation may occur during acute/subacute phase
HRCT may demonstrate ground-glass opacities, centrilobular nodules, and consolidation
Pulmonary Alveolar Proteinosis
Accumulation of PAS-positive phospholipids in alveoli
Perihilar consolidation
“Crazy-paving” on CT
Ground-glass opacities and septal thickening
Diagnosis via bronchoalveolar lavage
Bronchiolitis Obliterans with Organizing Pneumonia
a.k.a. cryptogenic organizing pneumonia
Granulation tissue in bronchioles and alveolar inflammation
Patchy alveolar consolidation, ground-glass opacification, centrilobular nodules
Diagnosis via tissue biopsy
Lymphoid Hyperplasia
Nonneoplastic nodular proliferation
Nonspecific nodular areas of consolidation
Adenopathy
Near-Drowning
Drowning 2nd most common cause of accidental death in children
Hypoxemia secondary to aspiration or laryngospasm
Pulmonary edema pattern on x-ray that may have delayed appearance
Edema typically resolves fairly rapidly
Pulmonary Inflammatory Pseudotumor
a.k.a. plasma cell granuloma
Most common benign lung neoplasm in children
May involve mediastinum and pleura
Occasional calcifications
Image Gallery
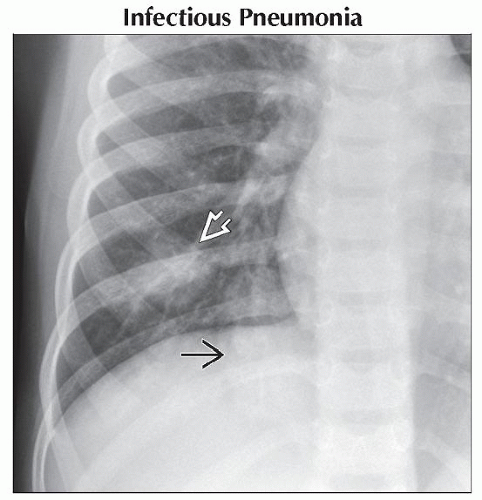 Frontal radiograph shows 2 areas of consolidation in the right lower lobe
 . The more lateral density . The more lateral density  is consistent with a round pneumonia in this 6 year old with a cough and fever. is consistent with a round pneumonia in this 6 year old with a cough and fever.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|