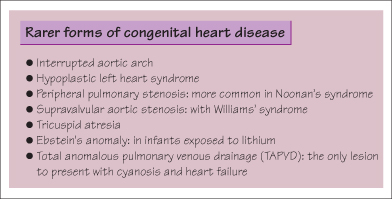
Congenital heart disease (CHD) is the commonest congenital malformation (7–8 per 1000 livebirths). About 8% are associated with chromosomal abnormality (e.g. AVSD in Down’s syndrome) or genetic abnormalities, such as a deletion at chromosome 22q11 which is associated with aortic arch defects and hypocalcaemia (diGeorge syndrome). The risk of CHD is higher if there is a family history. Teratogens may cause CHD (e.g. VSD and tetralogy of Fallot in fetal alcohol syndrome and Ebstein’s anomaly after fetal lithium exposure).
Many severe forms of CHD are diagnosed antenatally. Others present at birth, with cyanosis (e.g. transposition of the great arteries or pulmonary atresia) or shock (hypoplastic left heart syndrome). Some duct-dependent lesions present when the arterial duct closes within the first few days (e.g. coarctation of the aorta, severe pulmonary stenosis). Defects with a left to right shunt (e.g. VSD) present with heart failure and difficulty feeding some weeks after birth. Finally, some lesions may be asymptomatic and are first detected as a heart murmur (e.g. ASD, aortic stenosis) (see Chapter 20).
Medical management involves the control of heart failure, pending definitive repair. Many defects can just be monitored for years, and may not need surgical correction.
Congenital Heart Disease that Typically Presents in the Newborn Period
 Coarctation of the Aorta
Coarctation of the Aorta
This is a narrowing of the aortic arch. Severe coarctation presents in the first few days of life when the duct closes and insufficient blood is able to reach the lower limbs and perfuse vital organs, causing circulatory collapse and acidosis. The key feature is weak or impalpable femoral pulses. Blood pressure may be higher in the arms than the legs and oxygen saturation will be lower in the feet than the (preductal) right hand. Milder forms of coarctation present with heart failure and a murmur or with hypertension in a young adult. The immediate management is IV prostaglandin E2 to keep the arterial duct patent. Once the diagnosis is confirmed by echocardiography, the narrowed segment is repaired surgically or dilated using a balloon. In girls with Turner’s syndrome, 5–10% have coarctation and a proportion may also have a bicuspid aortic valve and aortic dissection in adulthood.
 Transposition of the Great Arteries
Transposition of the Great Arteries
In transposition of the great arteries (TGA), the aorta and main pulmonary artery are transposed, so that the aorta comes off the right ventricle and the pulmonary artery off the left ventricle. TGA always presents soon after birth with profound cyanosis and acidosis. The only way oxygenated blood from the lungs can reach the systemic circulation is across the arterial duct, or a VSD, if present. The emergency management is to commence a prostaglandin infusion, provide ventilatory and circulatory support and perform an atrial septostomy which allows mixing of oxygenated and deoxygenated blood. The definitive treatment is the ‘switch’ operation, where the two great vessels are switched over and the coronary arteries are reconnected to the new aorta. TGA can be missed on antenatal ultrasound scan since the basic ‘four-chamber’ view is normal.
Investigations and their signficance
| Pulse oximetry | To determine degree of cyanosis or check for postductal drop (screening for CHD) |
| Chest radiograph | Cardiomegaly in heart failure |
| Boot-shaped heart (Fallot’s tetralogy) | |
| Increased vascular markings with left to right shunts (VSD, ASD, PDA) | |
| ECG | Right ventricular hypertrophy |
| Superior QRS axis (AVSD, primum ASD) | |
| Echo | Ultrasound examination of the heart, usually performed by a paediatric cardiologist, can diagnose the vast majority of congenital heart defects |
| Fetal echo | Many defects can be detected antenatally |
| Cardiac catheter | To define complex anatomy or perform non-invasive treatment (e.g. balloon dilatation of stenosed valve) |
Tetralogy of Fallot
Tetralogy of Fallot is the commonest cyanotic defect, representing 6–10% of all CHD. ‘Tetralogy’ refers to a large VSD, an aorta that sits over the ventricular septum, pulmonary infundibular stenosis and right ventricular hypertrophy. The pulmonary narrowing causes a right-to-left shunt across the VSD. Some present with cyanosis at birth but others are diagnosed by an ejection systolic murmur. Classically these children develop hypercyanotic ‘spells’ which are relieved by squatting down (to reverse the right-to-left shunt by increasing left ventricular pressure). CXR may show a ‘boot-shaped’ heart. Surgical correction is usually performed at 2–3 months of age. Tetralogy of Fallot can have a genetic cause and is seen in fetal alcohol syndrome.
 Patent Ductus Arteriosus
Patent Ductus Arteriosus
During fetal life the arterial duct shunts blood from the pulmonary artery to the aorta, bypassing the unexpanded lungs. Normally the duct closes within a few days of birth, first by constriction and then by fibrosis. In sick preterm or hypoxic babies it remains open. As the right-sided pressures are now less than the aortic pressure, blood shunts from the systemic to the pulmonary circulation causing cardiac failure and pulmonary oedema. The clinical signs of a patent ductus arteriosus (PDA) are a continuous ‘machinery’ murmur below the left clavicle and collapsing pulses. A PDA is particularly common in premature infants receiving mechanical ventilation (up to 20%). Management involves diuretics and fluid restriction, and sometimes administration of prostaglandin synthetase inhibitors (e.g. indomethacin or ibuprofen). Rarely the duct needs to be closed by surgical ligation or by a trans-catheter occlusion device.
< div class='tao-gold-member'>



