Typically, surgery completed with the patient under general anesthesia. Preoperative antibiotics are given as indicated
In the setting of an isolated upper extremity compartment syndrome, the patient is placed in a supine position. A tourniquet is used rarely
Skin incision(s) should consider existing wounds or compromised skin to maximize soft-tissue flap viability
An initial skin-only incision permits meticulous hemostasis using electrocautery within the subcutaneous tissues and identification of the fascial plane for dissection
Following fasciotomy of the primary osteofascial envelope, each of the contained soft-tissue structures is evaluated for need of associated decompression, such as the epimysium or fascial septa of anatomic sub-compartments, such as the deep flexor digitorum profundus muscles or pronator quadratus muscle of the volar forearm
Sites of potential neurovascular constriction are inspected and released, such as the lacertus fibrosus at the proximal forearm
The skin is not closed at the initial decompression as a significant re-elevation of interstitial tissue pressures may occur
A sterile wound VAC or damp to dry dressing may be used for wound coverage following surgery
Postoperative care includes strict anti-edema/anti-swelling measures and upper limb range of motion exercises, as indicated
Compartmental Decompression
Arm/Brachium
Typically, access to the anterior and posterior compartments is completed via a lateral incision, although the need to extend the exposure distally into the forearm or more proximally to decompress the deltoid should be considered. Anteriorly, the fascia investing the brachialis muscle should be decompressed. At the elbow, the neurovascular structures should be traced across into the forearm, distal to the lacertus fibrosus to ensure that all sites of potential compression have been released (Fig. 1; Table 2).
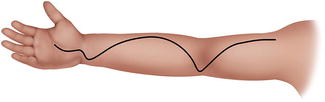
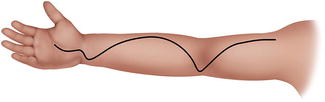
Fig. 1
Classic incision for forearm and then at fasciotomy with carpal tunnel release
Table 2
Decompression fasciotomies for compartment syndrome of the upper arm – surgical steps (Fig. 1)
Access to the anterior and posterior compartments may be made from a medial or lateral incision, along the midsagittal aspect of the arm |
A proximal extension of the exposure for access to the deltoid muscle or a distal exposure to include forearm decompression should be considered; a Bruner or curvilinear incision may provide a transition across the elbow region to the anterior/volar forearm |
Posterior compartment: decompression fasciotomy of the triceps fascia |
Anterior compartment: decompression fasciotomy of the biceps fascia and the brachialis fascia. The neurovascular structures in the distal arm/antecubital fossa should be decompressed with division of the lacertus fibrosus |
Dorsal Forearm
The dorsal forearm is exposed via a single, dorsal incision from 3 to 4 cm distal to the lateral epicondyle towards Lister’s tubercle. The superficial and deep muscular layers of the dorsal forearm, sub-compartmentalized by fascial septa, are inspected and decompressed (Fig. 2; Table 3).
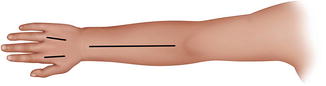
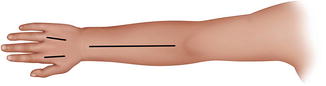
Fig. 2
Dora’s incisions for forearm and hand fasciotomy
Table 3
Decompression fasciotomies for compartment syndrome of the forearm: Surgical steps
Volar fasciotomies typically done first as decompression may reduce intra-compartmental pressures within the mobile wad and dorsal compartments to acceptable, physiologic levels |
Dorsal or posterior compartment: a dorsal, longitudinal incision is made to access the dorsal structures from the lateral elbow to the musculocutaneous junction at the mid- to distal 1/3 forearm (Fig. 2) |
Volar or anterior compartment: decompression fasciotomy should include the lacertus fibrosus proximally and the transverse carpal ligament/carpal tunnel, distally |
Careful decompression of the volar compartment and its sub-compartments is imperative. Individual muscles should be evaluated for epimysiotomy, particularly the deeper FDP and pronator quadratus |
Volar Forearm
Volar forearm fasciotomy may be accomplished via several surgical exposures. The approach of Henry is completed via an incision from the radial styloid to the antecubital fossa, in line with the medial epicondyle. Often, the incision is slightly curvilinear and incorporates a Bruner or oblique transition across the elbow flexion crease and the volar wrist crease to decompress the lacertus fibrosus/antecubital fossa contents and the carpal canal, respectively (Fig. 1). The modified McConnell approach uses a longitudinal volar-ulnar incision, thereby requiring an ulnar to radial dissection (Fig. 3). It begins 1 cm proximal and 2 cm lateral to the medial epicondyle and is carried out obliquely across the antecubital fossa towards the volar-ulnar aspect of the mobile wad. The incision is curved distally and ulnarly and reaches the midline of the forearm at the junction of the mid- and distal 1/3 forearm, before continuing distally, ulnar to the palmaris tendon. Similarly, an ulnar approach may minimize injury to the dominant blood supply to each forearm compartment (Ronel et al. 2004; Matsen et al. 1980). It is important to recognize the relative isolation of the pronator quadratus and the deep flexor compartment and the need for concomitant decompression of these potential sub-compartments of the volar forearm (Table 3).


Fig. 3
Ulnar-based incisions for forearm and thenar fasciotomies with carpal tunnel release
Mobile Wad
During decompression of the volar and/or dorsal compartments, direct or indirect decompression of the mobile wad may have occurred, and therefore, reevaluation is warranted prior to surgical incision. If necessary, a longitudinal incision is made overlying the mobile wad, carefully protecting the superficial branch of the radial nerve and the lateral antebrachial cutaneous nerve, or decompressive fasciotomy may be accomplished through the volar and/or dorsal fasciotomy sites (Table 3).
Hand
Carefully planned incisions are required to maximize soft-tissue viability as well as to ensure adequate exposure and decompression of each compartment in the hand. Two longitudinal dorsal incisions between the index-long and ring-small intervals permit meticulous release of the palmar and dorsal interosseous compartments along the length of the metacarpals, essential to ensure decompression of all osteofascial envelopes (Fig. 2). A longitudinal incision along the radial margin of the thenar eminence permits access to the thenar muscles, and the adductor pollicis (a separate compartment) is decompressed through an incision centered dorsally over the first web space. The hypothenar muscles are exposed via a longitudinal incision along the ulnar border of the hand with care as to preserve the neurovascular supply to the abductor digiti quinti in the region of the pisiform. The carpal tunnel is decompressed via a palmar incision made beginning at the level of Kaplan’s cardinal line, slightly ulnar to the thenar crease, and extending proximally to a point just distal to the volar wrist crease, 2–3 mm ulnar to the thenar crease unless extension proximally into the forearm is indicated via a Bruner transition across the volar wrist crease, protecting the palmar cutaneous branch of the median nerve (Fig. 4; Table 4).


Fig. 4
Incisions for thenar, adductor, and hypothenar fasciotomies with carpal tunnel release
Table 4
Decompression fasciotomies for compartment syndrome of the hand – surgical steps
Typically, complete fasciotomies of the hand include: (1) carpal tunnel; (2) thenar compartment; (3) hypothenar compartment; (4) intrinsics (multiple) |
Carpal tunnel: an incision from the level of Kaplan’s cardinal line distally to the volar wrist crease with a Bruner transition across the wrist crease is made with careful protection of the palmar cutaneous branch of the median nerve, the thenar motor branch, and the median nerve proper |
Intrinsics: two longitudinal, dorsal hand incisions are made to expose the palmar and dorsal interosseous musculature. The incisions are made in the approximate intervals of the index-long and ring-small interspaces. A third longitudinal incision may be made over the dorsal aspect of the first web space in order to evaluate and to decompress the adductor and first dorsal interosseous compartments |
Thenar: a longitudinal incision along the radial border of the thenar eminence, at the junction of the glabrous and non-glabrous skin, permits access to the thenar muscles (APB, FPB, OPP) and to the adductor muscle also |
Hypothenar: a longitudinal incision along the ulnar margin of the hand in order to expose the ADQ |
Digital fasciotomies are completed by integrating any existing wounds or areas of skin compromise and by using a mid-axial incision to maximize full-thickness flap coverage of the volar digit. Where feasible, for the index, long, and ring fingers, an ulnar incision is used, and a radial incision is made for the thumb and small finger in order to minimize potentially adverse effects to the sensibility of the digit. The incision is continued through Cleland’s ligaments, retracting the neurovascular bundles in a volar direction and remaining volar to the flexor tendon sheath. Selective incision of the flexor sheath may be necessary in the presence of a suppurative flexor tenosynovitis.
Aftercare
Medical resuscitation is important for global patient care, and the clinical team should remain alert for signs of renal dysfunction in particular, evidenced by myoglobinuria. Intravenous antibiotics are continued in the immediate postoperative period until a stable wound is appreciated or may be individualized based on the patient’s condition. Pediatric pain management may be indicated in certain cases, notably helpful to facilitate early joint and musculotendinous motion to prevent stiffness.
After adequate surgical decompression and debridement of the involved compartments, patients require continued observation for wound care and the initiation of hand/upper extremity range of motion where appropriate. Following initial fasciotomies, the limb should be splinted in a position of function. Careful monitoring of adjacent compartments for emerging pathology may be required in certain conditions such as infection. Reevaluation of the wound guides further management; debridement of all nonviable tissue in the operating room or a sterile environment approximately every 48–72 h may be required. The decision to continue with delayed wound closure or reconstruction is individualized to the patient’s condition. The use of a sterile vacuum-assisted closure (VAC) device may permit slightly longer intervals between subsequent wound evaluations once the absence of nonviable tissue is confirmed (Zannis et al. 2009). Prioritization of wound closure should consider neurovascular structures, exposed joints, and gliding tendons.
Anti-edema measures should be emphasized, including extremity elevation and avoidance of constrictive dressings or splints proximal to the surgical site. Splinting may help to minimize progressive contracture of the injured extremity and, at an appropriate time, may be removed to initiate range of motion exercises.
Summary
Pediatric upper extremity compartment syndrome is a complex injury involving an elevation of interstitial tissue pressures within an osteofascial envelope to non-physiologic levels, leading to alterations in tissue metabolism and, ultimately, to cellular death. The diagnosis of compartment syndrome can be challenging but the likelihood of an accurate diagnosis and effective treatment is enhanced by a high index of suspicion, careful clinical examination, and the use of adjuvant diagnostic methods such as the measurement of interstitial tissue pressure. While certain injuries such as a both-bone forearm fracture or supracondylar humerus fracture may be more commonly associated with the risk for compartment syndrome, there are many conditions for which increased tissue pressures may be subtle, including iatrogenic injury. The challenges of establishing a diagnosis of compartment syndrome in children add to the complexity of the condition. Despite prompt intervention, however, many variables impact treatment outcomes such as the amount of muscle damage from a direct trauma, the medical condition of the patient, and associated injuries such as fracture or soft-tissue deficit. Treatment occurs in stages, including medical resuscitation, emergent compartment fasciotomy with careful exploration and decompression of all tissues, wound care and delayed reconstruction, and subsequent rehabilitation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


