Chapter 392 Community-Acquired Pneumonia
Epidemiology
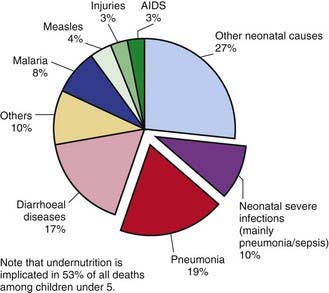
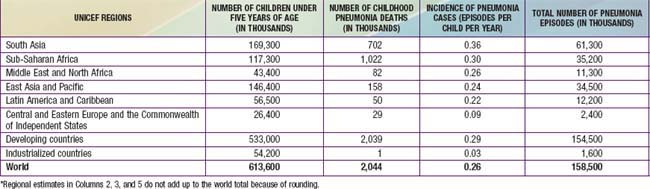
Pneumonia—inflammation of the parenchyma of the lungs—is a substantial cause of morbidity and mortality in childhood throughout the world, rivaling diarrhea as a cause of death in developing countries (Fig. 392-1). With ≈158 million episodes of pneumonia per year, of which ≈154 million are occurring in developing countries, pneumonia is estimated to cause ≈3 million deaths, or an estimated 29% of all deaths, among children younger than 5 yr worldwide. The incidence of pneumonia is more than 10-fold higher (0.29 episodes versus 0.03 episodes), and the number of childhood-related deaths due to pneumonia ≈2000-fold higher, in developing than in developed countries (Table 392-1).
Table 392-1 INCIDENCE OF PNEUMONIA CASES AND PNEUMONIA DEATHS AMONG CHILDREN UNDER FIVE, BY UNICEF REGION*
In the USA from 1939 to 1996, pneumonia mortality in children declined by 97%. It is hypothesized that this decline is attributable to the introduction of antibiotics, vaccines, and the expansion of medical insurance coverage for children. Haemophilus influenzae type b (Hib) (Chapter 186) was an important cause of bacterial pneumonia in young children but has become uncommon with the routine use of effective vaccines. The introduction of heptavalent pneumococcal conjugate vaccine and its impact on pneumococcal disease (Chapter 175) has reduced the overall incidence of pneumonia in infants and children in the USA by ≈30% in the 1st yr of life, ≈20% in the 2nd yr of life, and ≈10% in children >2 yr of age. In developing countries, the introduction of measles vaccine has greatly reduced the incidence of measles-related pneumonia deaths.
Etiology
Although most cases of pneumonia are caused by microorganisms, noninfectious causes include aspiration of food or gastric acid, foreign bodies, hydrocarbons, and lipoid substances, hypersensitivity reactions, and drug- or radiation-induced pneumonitis. The cause of pneumonia in an individual patient is often difficult to determine because direct culture of lung tissue is invasive and rarely performed. Cultures performed on specimens obtained from the upper respiratory tract or “sputum” often do not accurately reflect the cause of lower respiratory tract infection. With the use of state-of-the-art diagnostic testing, a bacterial or viral cause of pneumonia can be identified in 40-80% of children with community-acquired pneumonia. Streptococcus pneumoniae (pneumococcus) is the most common bacterial pathogen in children 3 wk to 4 yr of age, whereas Mycoplasma pneumoniae and Chlamydophila pneumoniae are the most frequent pathogens in children 5 yr and older. In addition to pneumococcus, other bacterial causes of pneumonia in previously healthy children in the USA include group A streptococcus (Streptococcus pyogenes) and Staphylococcus aureus (Chapter 174.1) (Table 392-2).
Table 392-2 CAUSES OF INFECTIOUS PNEUMONIA
| BACTERIAL | |
| Common | |
| Streptococcus pneumoniae | Consolidation, empyema |
| Group B streptococci | Neonates |
| Group A streptococci | Empyema |
| Mycoplasma pneumoniae* | Adolescents; summer-fall epidemics |
| Chlamydophila pneumoniae* | Adolescents |
| Chlamydia trachomatis | Infants |
| Mixed anaerobes | Aspiration pneumonia |
| Gram-negative enterics | Nosocomial pneumonia |
| Uncommon | |
| Haemophilus influenzae type b | Unimmunized |
| Staphylococcus aureus | Pneumatoceles, empyema; infants |
| Moraxella catarrhalis | |
| Neisseria meningitidis | |
| Francisella tularensis | Animal, tick, fly contact; bioterrorism |
| Nocardia species | Immunosuppressed persons |
| Chlamydophila psittaci* | Bird contact (especially parakeets) |
| Yersinia pestis | Plague; rat contact; bioterrorism |
| Legionella species* | Exposure to contaminated water; nosocomial |
| Coxiella burnetii* | Q fever; animal (goat, sheep, cattle) exposure |
| VIRAL | |
| Common | |
| Respiratory synctial virus | Bronchiolitis |
| Parainfluenza types 1-3 | Croup |
| Influenza A, B | High fever; winter months |
| Adenovirus | Can be severe; often occurs between January and April |
| Human metapneumovirus | Similar to respiratory syncytial virus |
| Uncommon | |
| Rhinovirus | Rhinorrhea |
| Enterovirus | Neonates |
| Herpes simplex | Neonates |
| Cytomegalovirus | Infants, immunosuppressed persons |
| Measles | Rash, coryza, conjunctivitis |
| Varicella | Adolescents or unimmunized |
| Hantavirus | Southwestern USA, rodents |
| Coronavirus (severe acute respiratory syndrome) | Asia |
| FUNGAL | |
| Histoplasma capsulatum | Ohio/Mississippi River valley; bird, bat contact |
| Blastomyces dermatitidis | Ohio/Mississippi River valley |
| Coccidioides immitis | Southwest USA |
| Cryptococcus neoformans | Bird contact |
| Aspergillus species | Immunosuppressed persons; nodular lung infection |
| Mucormycosis | Immunosuppressed persons |
| Pneumocystis jiroveci | Immunosuppressed, steroids |
| RICKETTSIAL | |
| Rickettsia rickettsiae | Tick bite |
| MYCOBACTERIAL | |
| Mycobacterium tuberculosis | Travel to endemic region; exposure to high-risk persons |
| Mycobacterium avium complex | Immunosuppressed persons |
| PARASITIC | |
| Various parasites (e.g., Ascaris, Strongyloides species) | Eosinophilic pneumonia |
* Atypical pneumonia syndrome; may have extrapulmonary manifestations, low-grade fever, patchy diffuse infiltrates, poor response to beta-lactam antibiotics, and negative sputum Gram stain.
From Kliegman RM, Greenbaum LA, Lye PS: Practical strategies in pediatric diagnosis & therapy, ed 2, 2004, Philadelphia, Elsevier, p 29.
S. pneumoniae, H. influenzae, and S. aureus are the major causes of hospitalization and death from bacterial pneumonia among children in developing countries, although in children with HIV infection, Mycobacterium tuberculosis (Chapter 207), atypical mycobacteria, Salmonella (Chapter 190), Escherichia coli (Chapter 192), and Pneumocystis jiroveci (Chapter 236) must be considered. The incidence of H. influenzae has been significantly reduced in areas where routine Hib immunization has been implemented.
Viral pathogens are a prominent cause of lower respiratory tract infections in infants and children <5 yr of age. Viruses are responsible for 45% of the episodes of pneumonia identified in hospitalized children in Dallas. Unlike bronchiolitis, for which the peak incidence is in the 1st yr of life, the highest frequency of viral pneumonia occurs between the ages of 2 and 3 yr, decreasing slowly thereafter. Of the respiratory viruses, influenza virus (Chapter 250), and respiratory syncytial virus (RSV) (Chapter 252) are the major pathogens, especially in children <3 yr of age. Other common viruses causing pneumonia include parainfluenza viruses, adenoviruses, rhinoviruses, and human metapneumovirus. The age of the patient may help identify possible pathogens (Table 392-3).
Table 392-3 ETIOLOGIC AGENTS GROUPED BY AGE OF THE PATIENT
| AGE GROUP | FREQUENT PATHOGENS (IN ORDER OF FREQUENCY) |
|---|---|
| Neonates (<3 wk) | Group B streptococcus, Escherichia coli, other gram-negative bacilli, Streptococcus pneumoniae, Haemophilus influenzae (type b,* nontypable) |
| 3 wk-3 mo | Respiratory syncytial virus, other respiratory viruses (parainfluenza viruses, influenza viruses, adenovirus), S. pneumoniae, H. influenzae (type b,* nontypable); if patient is afebrile, consider Chlamydia trachomatis |
| 4 mo-4 yr | Respiratory syncytial virus, other respiratory viruses (parainfluenza viruses, influenza viruses, adenovirus), S. pneumoniae, H. influenzae (type b,* nontypable), Mycoplasma pneumoniae, group A streptococcus |
| ≥5 yr | M. pneumoniae, S. pneumoniae, Chlamydophila pneumoniae, H. influenzae (type b,* nontypable), influenza viruses, adenovirus, other respiratory viruses, Legionella pneumophila |
From Kliegman RM, Marcdante KJ, Jenson HJ, et al: Nelson essentials of pediatrics, ed 5, Philadelphia, 2006, Elsevier, p 504.
* H. influenzae type b is uncommon with routine H. influenzae type b immunization.