Clinical Features of Bilirubin Encephalopathy
Terminology
Although originally a pathologic diagnosis characterized by bilirubin staining of the brainstem nuclei and cerebellum, the term kernicterus has come to be used interchangeably with both the acute and chronic findings of bilirubin encephalopathy. Bilirubin encephalopathy describes the
clinical central nervous system findings caused by bilirubin toxicity to the basal ganglia and various brainstem nuclei. To avoid confusion and encourage greater consistency in the literature, the AAP recommends (76) that the term acute bilirubin encephalopathy be used to describe the acute manifestations of bilirubin toxicity seen in the first weeks after birth and that the term kernicterus be reserved for the chronic and permanent clinical sequelae of bilirubin toxicity. This is the terminology that is used in this chapter. Recently, Johnson and associates suggested the use of the term bilirubin-induced neurologic dysfunction (BIND) (121) to describe the changes associated with acute bilirubin encephalopathy; they also proposed a scoring system to quantify the severity of the clinical manifestations.
clinical central nervous system findings caused by bilirubin toxicity to the basal ganglia and various brainstem nuclei. To avoid confusion and encourage greater consistency in the literature, the AAP recommends (76) that the term acute bilirubin encephalopathy be used to describe the acute manifestations of bilirubin toxicity seen in the first weeks after birth and that the term kernicterus be reserved for the chronic and permanent clinical sequelae of bilirubin toxicity. This is the terminology that is used in this chapter. Recently, Johnson and associates suggested the use of the term bilirubin-induced neurologic dysfunction (BIND) (121) to describe the changes associated with acute bilirubin encephalopathy; they also proposed a scoring system to quantify the severity of the clinical manifestations.
Acute Bilirubin Encephalopathy
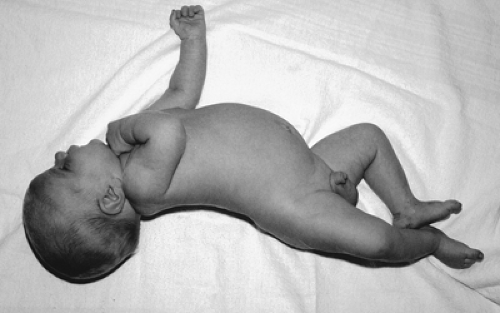
In classic acute bilirubin encephalopathy, markedly jaundiced infants progress through three fairly distinct clinical phases (Table 35-9) (51,122,123,124). In the early phase, the infant becomes lethargic and hypotonic, and sucks poorly. The intermediate phase is characterized by moderate stupor, irritability, and hypertonia. The infant may develop a fever and a high-pitched cry (51), which might alternate with drowsiness and hypertonia. The hypertonia involves the extensor muscle groups, and most infants exhibit backward arching of the neck (retrocollis) and trunk (opisthotonos) (Fig. 35-10). The fever may be caused by diencephalic involvement. The advanced phase is characterized by pronounced retrocollis-opisthotonos, shrill cry, refusal to feed, apnea, fever, deep stupor to coma, and sometimes seizures and death (51,123,124).
TABLE 35-9 MAJOR CLINICAL FEATURES OF ACUTE BILIRUBIN ENCEPHALOPATHY | ||
|---|---|---|
|
Subsequently, usually after 1 week, hypertonia subsides and is replaced by hypotonia. Infants who manifest hypertonia during the second phase almost always develop the clinical features of chronic bilirubin encephalopathy (122,123) although an emergent exchange transfusion might, in some cases, reverse the CNS changes (125). Van Praagh (123) found that those who were consistently neurologically normal during the first week of life never developed the features of chronic encephalopathy, but other investigators found later evidence of brain damage in some infants in whom no, or equivocal, manifestations of kernicterus were apparent in the newborn (Table 35-10) (122,126,127).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree