Fig. 1
Neonatal clavicle fracture on the right side sustained during a difficult vaginal delivery (Courtesy of Joshua M. Abzug, MD)
Children who have clavicle fractures from suspected abuse should undergo a comprehensive head-to-toe survey as if he or she is a trauma patient, so that any concomitant injuries and/or signs of abuse may be detected. Included in this survey are a thorough neurological evaluation, ophthalmologic examination, and a skeletal survey to identify corner fractures or any additional fractures in various phases of healing.
Physical examination of a child with a clavicle fracture involves observing for swelling, deformity, and ecchymosis around the affected clavicle. Open wounds should be noted, as these signs may dictate management. Furthermore, the lateral aspect of the shoulder should be examined for abrasions or erythema, as this is the most common site of impact. Drooping of the involved side may also be seen, as the scapula appears internally rotated and the shoulder appears shortened compared to the contralateral side. However, if significant swelling occurs, this may be difficult to appreciate.
Clavicle fractures typically cause pain about the entire shoulder girdle; however, significant tenderness to palpation is most prominent at the fracture itself. Crepitus may also be present with any attempt of either active or passive range of motion. An associated injury to the brachial plexus may occur, with the lower trunk being especially susceptible due to its location adjacent to the middle third of the clavicle. Therefore, a thorough neurological examination, including assessment of motor and sensory function throughout the entire upper extremity, is mandatory for all patients who sustain clavicular fractures. It may be challenging for a child in pain to perform certain tasks required to complete the neurological evaluation; however, it is crucial to remain patient and repeat the examination as often as necessary to acquire the necessary information.
A comprehensive vascular examination is also necessary due to the location of the subclavian vessels, particularly in patients who have undergone high-energy mechanisms of injury, as the vessels may spasm or undergo thrombosis from blunt trauma. Palpation of both radial arteries should reveal symmetric pulses, and if there is concern for vascular injury, further evaluation with advanced imaging should be performed.
Midshaft Clavicle Fracture Imaging and Other Diagnostic Studies
Initially, imaging of a suspected clavicle fracture should include plain radiographs of the clavicle in two projections, typically a standard anteroposterior (AP) radiograph and an apical lordotic view or 45 ° cephalic tilt view. The apical lordotic view is an AP view with the tube directed 45° cephalad and can be utilized to evaluate the amount of displacement. With these views, one can also visualize the shoulder girdle region as well as the upper lung fields, both of which should be assessed for additional injuries. If clinical suspicion for additional injuries is present, dedicated series of the suspected region(s) should be acquired. Advanced imaging is rarely needed to evaluate clavicle fractures, as the fracture pattern, displacement, and presence of comminution can be easily assessed on plain films. In the setting of high-energy trauma, a chest CT is typically obtained and can be utilized to further evaluate the clavicle fracture.
Injuries Associated with Midshaft Clavicle Fractures
Injuries associated with clavicle fractures vary based on the age of the child. Brachial plexus palsies can be associated with midshaft clavicle fractures in neonates, most commonly affecting the C5 and C6 nerve roots. This can result in limited shoulder movement, elbow flexion, forearm supination, and wrist extension (Gilbert and Whitaker 1991). Differentiation between a pseudopalsy, the child not moving his or her arm secondary to the clavicle fracture itself, and an associated neonatal brachial plexus palsy can be made by 3–4 weeks of age, when the pain from the fracture will be markedly decreased due to early callus formation. Children who sustain clavicle fractures resulting from nonaccidental trauma are likely to sustain additional injuries such as fractures of the rib, tibia/fibula, humerus, or femur, intracranial bleeding, eye contusions, retinal hemorrhage, and/or burns (Chang et al. 2004; Pandya et al. 2009). Adolescents with clavicle fractures due to high-energy mechanisms of injury may have associated polytrauma, including injury to vital organs or adjacent structures. Concomitant rib fractures, scapula fractures, pneumothorax, brachial plexus injury, or subclavian vessel injury can also occur (Jeray 2007). Abdominal, head, spine, and/or lower extremity trauma may also be present.
Midshaft Clavicle Fracture Classification
Clavicle fractures are typically classified based on fracture location, pattern, and the presence or absence of displacement. Thus, clavicle fractures are described as medial, midshaft, or lateral; non-displaced or displaced; open or closed; and comminuted or simple. Additional classification schemes to assess adult clavicle fractures have been proposed, but none are extensively utilized, as their nomenclature is either purely descriptive of fracture location or cumbersome with several types and subtypes (Allman 1967; Orthopedic Trauma Association 1996; Robinson 1998).
Midshaft Clavicle Fracture Outcome Tools
There are currently no outcome scores specifically utilized to evaluate results following pediatric clavicle fractures. Outcome measures such as patient satisfaction, range of motion, pain, fracture union, and complications are commonly employed. Additional measures including the Disability of the Arm, Shoulder, and Hand (DASH) score, QuickDASH, Simple Shoulder Test, and Constant Shoulder Score have been used to assess outcomes. Radiographic criteria evaluating shortening and/or vertical displacement of the clavicle have also been utilized to evaluate outcomes.
Midshaft Clavicle Fracture Treatment Options
Nonoperative Treatment of Midshaft Clavicle Fractures
Indications/Contraindications
The established treatment of pediatric and adolescent clavicle fractures is nonoperative, allowing the fracture to form callous and heal in situ, regardless of whether there is significant displacement (Fig. 2) (Bae et al. 2013). Well-established indications for nonoperative management include non-displaced or minimally displaced fractures, defined as displacement less than 1.5–2 cm. Conversely, open fractures and fractures with associated neurovascular injury or limb at risk should all proceed directly to operative intervention (Table 1).


Fig. 2
Healed neonatal clavicle fracture demonstrating the abundance of callus formation that occurs (Courtesy of Joshua M. Abzug, MD)
Table 1
Midshaft clavicle fractures: Nonoperative management
Indications | Contraindications |
|---|---|
Non-displaced fractures | Open fractures |
Minimally displaced fractures (<1.5–2 cm) | Fractures associated with neurovascular injury |
Techniques
Nonoperative treatment of clavicle fractures is achieved by immobilizing the child’s shoulder girdle, classically with a sling. A figure of eight dressing or shoulder immobilizer can alternatively be used. Immobilization in neonates who have sustained a clavicle fracture during the birthing process can be achieved by performing a swathe technique, such as placing cast padding followed by an ACE bandage around the torso and arm.
Follow-up radiographs are obtained at 4-week intervals until fracture union is achieved. The child is allowed to resume normal activities as tolerated once union is accomplished. Calder et al. have proposed that follow-up radiographs are unnecessary in the pediatric population due to the near universal fracture-healing rate of children (Calder et al. 2002). However, in children wishing to return to sports, radiographs should be obtained until union is established in order to decrease the refracture risk.
Outcomes
Even though pediatric clavicle fractures have a relatively high incidence and the majority of pediatric clavicle fractures are treated nonoperatively, there is little data regarding the outcomes of these injuries. Union rates from 95 % to 100 % have been reported with nonoperative treatment (Grassi et al. 2001; Khan et al. 2009; Vander Have et al. 2010). Most non-displaced fractures unite by 4–8 weeks post-injury, while displaced fractures achieve union in approximately 10 weeks (Vander Have et al. 2010).
The majority of patients obtain excellent outcomes and are capable of returning to their activities without restrictions. A small percentage of patients with significant fracture displacement who are treated nonoperatively may have subjective complaints of pain with prolonged activity, easy fatigability, axillary pain, or drooping shoulders with bony prominence (Vander Have et al. 2010). Bae et al. evaluated 16 patients with displaced (>2 cm) mid-diaphyseal clavicle fractures treated nonoperatively. All fractures achieved union with no meaningful loss of shoulder motion or abduction-adduction strength by isokinetic testing. The majority of patients had low DASH and pain Visual Analog Scores (VAS) that were very low, with means of 4.9 and 1.6, respectively. Only one patient required a corrective osteotomy (Bae et al. 2013). The authors concluded that routine surgical fixation for displaced, nonsegmental clavicle fractures may not be justified based on concerns regarding shoulder motion and strength alone. Further investigations are needed to determine the risk factors and causes of pain and functional compromise in the minority of pediatric patients with symptomatic malunions. In contrast, adult studies have shown that patients with significantly displaced midshaft fractures that are treated nonoperatively have significantly worse Constant Shoulder Scores and DASH scores, higher rates of nonunion, longer times to union, and more symptomatic malunions than those who have undergone plate fixation (Canadian Orthopedic Trauma Society 2007).
Operative Treatment of Midshaft Clavicle Fractures
Indications/Contraindications
Absolute indications for operative management of pediatric and adolescent clavicle fractures include open fractures, comminuted fractures in which the central fragment is markedly displaced (Fig. 3), and fractures associated with neurovascular injury. Floating shoulder injuries and fractures associated with polytrauma are considered relative indications for surgical treatment by some authors. A floating shoulder injury created by a midshaft clavicle fracture and glenoid neck fracture may be managed by open reduction and internal fixation (ORIF) of the clavicle exclusively, as ligamentotaxis via the coracoclavicular ligament will reduce the accompanying glenoid fracture (Bahk et al. 2009).
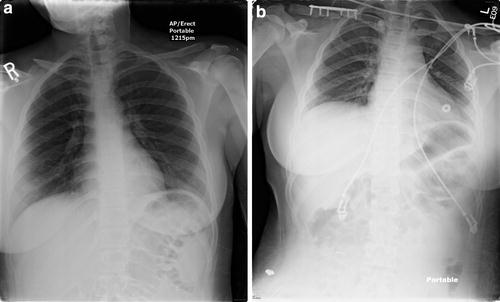
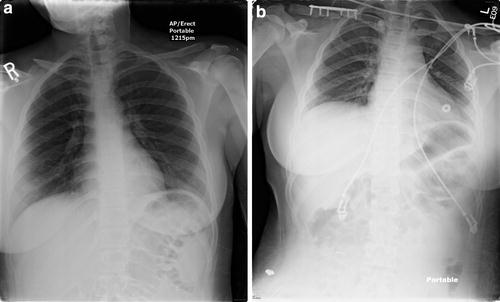
Fig. 3
Displaced right clavicle fracture with a central “zed”-type fragment. (a). Preoperative. (b). Postoperative (Courtesy of Joshua M. Abzug, MD)
Significantly displaced fractures in adults that are managed nonoperatively have demonstrated healing with a malunion that can trigger changes in shoulder mechanics, including pain with overhead activities, decreased strength, and decreased endurance (Hill et al. 1997; McKee et al. 2003). The benefit of operative fixation versus nonoperative treatment of displaced midshaft clavicle fractures has been the subject of several studies. One recent meta-analysis of randomized clinical trials comparing operative and nonoperative treatment in adults revealed a significantly higher nonunion and symptomatic malunion rate in the nonoperative group. Furthermore, patients managed with operative interventions demonstrated earlier functional return, but it is unclear whether this data is applicable to adolescents (McKee et al. 2012). It is clear, however, that young children, especially younger than age 8, have the potential to remodel foreshortened, displaced fractures.
Surgical Procedure
Preoperative Planning
Similar to any procedure that utilizes medical implants, it is essential to have the necessary hardware available prior to proceeding to the operating room (Table 2). Several options exist for treating pediatric and adolescent clavicle fractures, including anatomically designed clavicle plates, standard non-locking and locking plates, and intramedullary devices such as pins, wires, screws, and elastic nails.
Table 2
ORIF of midshaft clavicle fractures: Preoperative planning
OR table: standard OR table capable of beach chair positioning or utilization of a Mayfield head positioner |
Position/positioning aids: supine beach chair or Mayfield headrest position with the head/neck tilted away |
Bump placed behind the scapula |
Fluoroscopy location: contralateral to fracture |
Equipment: surgeon’s choice of implant |
Tourniquet (sterile/nonsterile): none |
Draping: shoulder girdle, entire clavicle, and ipsilateral limb and prepped and draped into the field to allow for visualization, traction, and manipulation |
Medially, the contralateral sternoclavicular joint should be included in the operative field |
Plate fixation requires one to determine if the location of the plate will be anteroinferior or superior. The benefit of using anteroinferior plates is the ability to drill in a posterosuperior direction so that the drill is not directed toward the surrounding neurovascular structures. Moreover, the plate is less prominent in this location. Superior placement of the plate is technically easier and provides strong resistance of the biomechanical forces acting to displace the fracture.
Compared to plate fixation, intramedullary fixation provides the potential benefits of requiring less soft tissue stripping at the fracture site, smaller skin incisions leading to better cosmesis, decreased risk of hardware irritation, easier hardware removal, and less bony weakness after plate removal (Fig. 4). However, intramedullary fixation provides inferior resistance to torsional forces when compared to plating, which can result in fracture of the intramedullary implant. Additionally, the intramedullary device has the potential to migrate, which raises major concerns and has thus limited usage of these devices.


Fig. 4
Midshaft clavicle fracture treated with an intramedullary device (Courtesy of Dan A. Zlotolow, MD)
Positioning
Positioning options during ORIF or intramedullary fixation of clavicle fractures include the beach chair position with or without a Mayfield head positioner or having the patient supine. With either position, a bump is placed behind the scapula to assist in reducing the fracture.
Surgical Approaches
ORIF is performed via a direct approach to the clavicle by creating a skin incision that follows Langer’s lines (Table 3). Skin incisions placed in locations not directly overlying the planned plate location on the clavicle can be done in order to avoid wound complications and to improve cosmesis (Coupe et al. 2005). Following the incision, electrocautery is utilized to divide the platysma, fascia, and periosteum in line with the initial skin incision. Throughout this process, it is imperative to identify and protect the cutaneous supraclavicular nerves which may number as many as 3–4. Subperiosteal dissection is then performed to expose the fracture site while ensuring that soft tissue attachments to any malrotated or segmental fracture fragments are preserved.
Table 3
ORIF of midshaft clavicle fractures: Surgical steps
Skin incision approximately 1 cm inferior to the clavicle in line with Langer’s lines |
Electrocautery through the platysma, fascia, and periosteum directly onto the clavicle while avoiding injury to the supraclavicular cutaneous nerves |
Expose fracture site in a subperiosteal manner while preserving soft tissue attachments to malrotated and comminuted fragments |
Reduce fracture fragments utilizing bone-holding forceps |
Apply plate in desired location |
Assess reduction and screw lengths with direct visualization and fluoroscopic imaging in multiple planes |
Close periosteum |
Meticulous skin closure with absorbable suture |
Apply sling or shoulder immobilizer |
Intramedullary fixation is accomplished via an approach that utilizes a small incision over the fracture site to expose only the ends of fracture fragments (Table 4). In order to place the intramedullary device in an antegrade manner, an additional percutaneous incision is positioned over the superolateral region of the clavicle.
Table 4
Intramedullary fixation of midshaft clavicle fractures: Surgical steps
Skin incision overlying the fracture site in line with Langer’s lines |
Electrocautery through the fascia and periosteum directly onto the clavicle while avoiding injury to the supraclavicular cutaneous nerves |
Expose fracture site in a subperiosteal manner while preserving soft tissue attachments to malrotated and comminuted fragments |
Drill the medial segment of the fracture in preparation for device placement while ensuring no violation of the anterior medial cortex occurs |
Drill distal fragment medullary canal and exit out posterior lateral cortex so that the drill can be visualized just beneath the skin |
Make a percutaneous skin incision where the drill is tenting the skin |
Place intramedullary device in a retrograde manner through fracture site to exit through posterior lateral skin incision |
Reduce fracture fragments |
Advance device antegrade across the fracture |
Utilize device-specific mechanisms, if available, to prevent migration or permit compression |
Close periosteum |
Meticulous skin closure with absorbable suture |
Apply sling or shoulder immobilizer |
Technique
Once the fracture site and fragments are exposed, the fracture is reduced using bone-holding forceps. A separate interfragmentary screw or mini-fragment plate fixation can be used in segmental fractures to reduce the fracture from three parts to two. The fracture is then anatomically reduced and clamped, ensuring that areas of comminution are accounted for. Either an anatomic clavicular plate or a small pelvic reconstruction plate is then contoured to permit rigid internal fixation. The plate is subsequently applied in the preferred position, and the reduction, screw placement, and length are assessed with a combination of direct visualization and fluoroscopic imaging in multiple planes. Subsequently, the supraclavicular nerves are protected and the periosteum is closed. Layered closure with absorbable suture, including meticulous skin closure, is then performed to decrease the risk of wound complications and allow for the best possible cosmesis. Lastly, the patient is placed in a sling or shoulder immobilizer.
Intramedullary fixation is performed by exposing the fracture ends and then drilling the distal fragment in a retrograde direction through the intramedullary canal to exit the posterior-lateral cortex. The medial segment is then drilled while ensuring that there is no violation of the anterior medial cortex. The device is then placed retrograde through the canal to exit the posterior-lateral hole followed by the skin. Subsequently, the fracture is reduced and the intramedullary device is advanced antegrade across the fracture site. Several devices have mechanisms that may now be employed in order to prevent migration of the device and to permit fracture compression.
Treatment-Specific Outcomes
The majority of studies regarding the management of pediatric and adolescent midshaft clavicle fractures are retrospective and involve preadolescents and adolescents. Mehlman et al. retrospectively reviewed 24 children, with a mean age of 12 years, who underwent operative treatment of completely displaced clavicle shaft fractures. This series reported zero nonunions or infections, and 21 of the 24 patients were able to return to unrestricted sports activity. Three complications were reported, including two patients with scar sensitivity and one patient who developed a transient ulnar nerve neurapraxia. Hardware removal was performed on an elective basis for all patients (Mehlman et al. 2009).
Namdari et al. also performed a retrospective review of 14 skeletally immature patients who underwent ORIF for displaced midshaft clavicle fractures. There were no nonunions reported, but eight patients had numbness about the surgical site. Four patients required hardware removal (Namdari et al. 2011).
The only comparative study to date evaluating nonoperative versus operative management of midshaft clavicle fractures in adolescents was performed by Vander Have et al. In this retrospective review of 43 fractures, 25 were treated nonoperatively and 17 were treated operatively. Neither group reported a nonunion although 5 symptomatic malunions occurred in the nonoperative group, 4 of which were managed with corrective osteotomy. All complications within the operative group were associated with hardware prominence. Return to full activities occurred faster in the operative group, by approximately 4 weeks, when compared to the nonoperative group (Vander Have et al. 2010).
Although the Vander Have study reported a high rate (20 %) of symptomatic malunion in the nonoperative group, with many patients requiring corrective osteotomy, Bae et al. have recently reported that the majority of significantly displaced (>2 cm) diaphyseal clavicle fractures treated nonoperatively result in an asymptomatic malunion that does not require corrective osteotomy. Of the 16 fractures included, all progressed to malunion with only 1 patient requiring a corrective osteotomy. The mean DASH score was low at 4.9 and the mean pain VAS was 1.6. There was no significant loss of strength or motion reported (Bae et al. 2013; Vander Have et al. 2010).
Preferred Treatment
The vast majority of pediatric and adolescent clavicle fractures are managed nonoperatively with 3–4 weeks of immobilization. Schulz et al. determined that nonoperative treatment of adolescents with displaced and shortened midshaft clavicle fractures is effective, with good functional outcomes (Schulz et al. 2013). Additionally, a long-term study by Randsborg and colleagues demonstrated good to excellent patient-reported outcomes in the majority of adolescents following nonoperative treatment of clavicle fractures (Randsborg et al. 2013). The authors of these studies concluded that nonoperative management of clavicle fractures in adolescents should remain the mainstay of treatment. Home or formal rehabilitation is then performed to restore range of motion and strength prior to resuming full activities. Operative treatment is performed for open fractures, fractures associated with neurological or vascular injury, and significantly displaced fractures in athletes.
The beach chair position is utilized along with a Mayfield head positioner with a skin incision placed approximately 1 cm inferior to the clavicle. Once the fracture fragments are exposed, the fracture is reduced utilizing bone-holding forceps. In comminuted fractures, mini-fragment plates are placed to convert multiple small pieces into large fragments. During the reduction process, it is critical to restore the length and contour of the clavicle, which is achieved by utilizing smooth wires, suture, mini-fragment plates, or interfragmentary screws. When the reduction is anatomic, the plate is applied to the superior aspect of the clavicle. A malleable retractor is placed inferior to the clavicle in order to protect the surrounding neurovascular structures. Following plate placement, fluoroscopic imaging and direct visualization are utilized to assess the fracture reduction and screw lengths. Thorough irrigation of the wound is then performed and the periosteum is closed. The wound is then closed with a meticulous subcuticular closure in order to obtain the best cosmesis and decrease the chance of wound complications. Sterile dressings including a Tegaderm are applied, and the patient is placed into either a sling or shoulder immobilizer.
Surgical Pitfalls and Prevention
The most dreaded complication during operative treatment of clavicle fractures is damage to a neurovascular structure and/or creation of a pneumothorax. Utilizing meticulous technique during fracture fragment exposure and while drilling/placing screws during plate application can prevent these extremely rare iatrogenic complications. It is critical to stay subperiosteal while exposing fracture fragments in order to create a layer between the bone and surrounding structures. Retractors can then be positioned in this layer, and direct visualization can be employed during drilling and screw placement to limit any chance of damage to the nearby neurovascular structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


