Child Maltreatment
Robert M. Reece
EPIDEMIOLOGY OF CHILD MALTREATMENT
In the United States in 2003, approximately 2.9 million children were reported to Children’s Protective Service (CPS) agencies for abuse and/or neglect. Approximately one-third of the reported cases (906,000) were substantiated as abuse or neglect after investigation, representing a rate of 12.4 per 1,000 U.S. children. Approximately 60% suffered neglect, 19% were physically abused, 10% were sexually abused, and 5% were emotionally maltreated. In addition, 17% were associated with other types of abuse. (These numbers add up to over 100% because many children are victims of more than one type of maltreatment.) The highest victimization rates were for the 0- to 3-year age group, and girls were slightly more likely to be victims than were boys. Pacific Islander children, American Indian or Alaska Native children, and African-American children had the highest rates of victimization. The rate of white victims of child abuse or neglect was 11.0 per 1,000 children of the same race or ethnicity; the rate for Pacific Islanders was 21.4 per 1,000 children; for American Indian or Alaska Natives, 21.3 per 1,000 children; and for African-American children, 20.4 per 1,000 children.
Approximately 1,500 children died from child abuse and neglect in 2003, a rate of 2 deaths per 100,000. More than 75% of these deaths occurred in children under 4 years of age; 10% were 4 to 7 years old; 5% were 8 to 11 years old, and 6% were 12 to 17 years old.
Almost 60% of all perpetrators were female because the most common pattern of maltreatment was a child neglected by a female parent. Victims of physical or sexual abuse were more likely to be maltreated by a male parent, a male relative, or other males. Parents were the perpetrators of maltreatment in 80% of cases.
DEFINITIONS OF CHILD MALTREATMENT
The definition of physical abuse in Public Law 93–247 is “the physical or mental injury, sexual abuse, negligent treatment, or maltreatment of a child under the age of eighteen by a person who is responsible for the child’s welfare under circumstances which indicate the child’s health or welfare is harmed or threatened thereby.” Neglect occurs when a caretaker responsible for a child either deliberately or by extraordinary inattentiveness permits a child to suffer or fails to provide one or more of the conditions generally deemed essential for developing a person’s physical, intellectual, or emotional capacities.
PHYSICAL ABUSE
Bruises
Several studies of bruises in random populations of children have shown that the locations of nonintentional bruises are related to the developmental stage of the child. Bruises anywhere on the body are extremely uncommon in infants less than 6 months old but are more commonly seen as the child becomes increasingly mobile. Infants who do not yet “cruise” bruise only rarely. In Sugar’s study bruising was rare in normal children on the hands, buttocks, cheeks, nose, forearms, or chest. Bruises on the lower legs were found to be uncommon in children less than 18 months of age in Roberton’s study, but in Sugar’s series nearly one in five of the “cruisers” (10 to 18 months of age) and half of the “walkers” had bruises, most frequently on the shins and knees. In Roberton’s study, head and facial injuries were common in the 10- to 18-month-old age group and uncommon over the age of 4 years. Less than 1% of children below 3 years of age had lumbar bruises, but lumbar bruises occurred in 14% of the children of school age.
“Aging” of Bruises
The color changes that occur in bruises are quite variable in relationship to the age of the bruise. The difficulties inherent in assessing the age of bruises include variability in the depth, the location, the vascularity of the underlying tissue, and the age and skin complexion of the child. Superficial bruises occur almost immediately, while deep bruises may take days to appear. The color of the bruise also depends on the depth of the bruise, with yellowish tinges appearing in 3 days in superficial bruises, while in deeper bruises the yellow color may not be appreciated until 7 to 10 days. Blood is seen sooner in loose tissues (such as around the eyes). In one study of 369 photographs of bruises, the authors concluded that (a) a bruise with any yellow must be older than 18 hours; (b) red, blue, and purple or black may occur anytime from 1 hour to resolution; (c) red color has no bearing on the age of the bruise because red color can be present in bruises no matter what the age is; and (d) bruises of identical ages and cause on the same person may not appear as the same color and may not change at the same rate. Visual aging of bruises is an inexact science and should not be relied upon to ascertain that a particular bruise is consistent with a specific age. As in all injuries, the history of the injury is important, along with an appraisal of the biomechanics required to produce the tissue damage in question.
Distinguishing between Inflicted and Nonintentional Bruises
Inflicted bruises often have characteristic locations, patterns, or shapes that can help differentiate them from nonintentional
injuries (Table 17.1). Bruises located over bony prominences are more likely to be nonintentional, whereas bruises on the dorsal surface of the body are more likely to be inflicted. Certain patterns of bruising help identify the inflicting agent (Box 17.1).
injuries (Table 17.1). Bruises located over bony prominences are more likely to be nonintentional, whereas bruises on the dorsal surface of the body are more likely to be inflicted. Certain patterns of bruising help identify the inflicting agent (Box 17.1).
TABLE 17.1. RELATIONSHIP OF LOCATION AND CAUSE OF BRUISES | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Differential Diagnosis
Both common and rare skin conditions need to be considered when diagnosing skin bruises (Box 17.2). Other more rare causes of bruising, petechiae, or purpura, but less likely to be confused with child abuse, include Rocky Mountain spotted fever, disseminated intravascular coagulopathy, meningococcemia, vitamin K deficiency secondary to cystic fibrosis, head lice with maculae caeruleae (linear bruises), capillary hemangiomas, eczema, purpura fulminans, spider bites, and calcium chloride cutaneous necrosis.
BOX 17.1 Shape/Size/Patterns of Inflicted Bruises
Pinch marks appear as small double bruises.
Open-handed slap produces clear skin mark where fingers hit (negative image), with fingers outlined by linear stress petechiae. This happens with high-velocity injuries; with high velocity and large forces, bruising is seen as a positive image outlined by petechiae.
Belts, ropes, strings, cords, shoes, hairbrushes, coat hangers, extension cords, kitchen utensils, and many other instruments can leave identifiable imprints.
Vertical bruises on the buttocks at the margin of the gluteal cleft can be due to whipping, paddling, or spanking. The mechanics of this injury involve a crimping of the skin at the gluteal cleft margins.
Bruises under the fingernails (subungual hematomas)
Bilateral black eyes in a child are almost always of inflicted origin. Attribution of this injury to another child by the caretakers is common, but children under 10 years of age have neither the motivation nor the power to inflict this degree of injury.
Petechiae on the face and neck, and subconjunctival hemorrhages from strangulation injuries.
Bruises on the pinna of the ear from “boxing” the ears with both open hands, or by pinch injuries while pulling the child by the ear.
Tattooing
Factitious dermatitis (Munchausen by proxy)
BOX 17.2 Differential Diagnosis of Cutaneous Lesions in Child Abuse
“Mongolian spots”: More accurately termed slate blue nevi, these bluish-gray discolorations of the skin occur in many children of African, Asian, or Mediterranean origin. They are present at birth, may be extensive, involve multiple areas, and may be seen on any part of the body. They are most commonly seen on the buttocks or lower back.
Ehlers-Danlos syndrome: This inherited connective tissue disorder is characterized by skin fragility (easy bruisability), joint hypermobility, and skin hyperelasticity.
Erythema multiforme: Intradermal hemorrhage and petechiae, with purpura usually starting at the palms, soles, hands, feet, and leg extensor surfaces, and extending to the trunk and face is typical. Target lesions are flat macules with small papular centers.
Coagulopathies: Idiopathic thrombocytopenic purpura, leukemia, hemophilia, von Willebrand’s disease.
Henoch–Schönlein purpura: This is thought to be an IgA-mediated vasculitis in small vessels of involved organs. Seventy-five percent of all cases occur in children 2–11 years of age, with younger children rarely affected.
Secondary syphilis: Purpuric lesions sometimes on the palms and soles.
Allergic shiners: Dark areas under eyes often seen in children with hayfever or other allergic rhinitis.
Cultural rituals: Cao gio (coining), cupping, quat shat (spooning).
Phytophotodermatitis: Lime, lemon, or other citrus fruit juice on skin followed by exposure to sunlight produces hand print patterns.
The approach to the evaluation of suspected abusive cutaneous injuries is shown in Box 17.3.
Burns
Burns are defined as a chemical and physical insult to tissue resulting from thermal, electrical, chemical, or radiation mechanisms.
Epidemiology
Approximately 40,000 children under the age of 15 years are hospitalized each year because of burns and more than 2,000 children die from burn injury each year. Most studies show that 20% of burns in young children are abusive. Burns represent 10% of all physical abuse cases. Scald burns comprise 85% of all burns in childhood, with the greatest prevalence in children less than 4 years of age. Flame burns account for 13% of the total, with chemical and electrical burns representing the remainder. Boys are burned more often than girls. As in most maltreatment, burns of inflicted origin are seen more often in younger children than accidental burns.
Types of Burns
Thermal Burns
Scald Burns
Forced immersion scalds are usually uniform in depth, with sharply demarcated borders, and flexion creases are relatively spared. When a child’s hands or feet are held
forcibly in hot water, the burns take on a stocking or glove appearance, and the burns are often bilateral. Buttocks, lower back, and perineum burns occur when a child’s middle body is forcibly held under hot water. In some cases, areas are spared from scalding if these areas of skin are in contact with a relatively cooler surface such as the bottom of a tub (donut burns). In other cases, body creases are spared because apposing surfaces of skin are not exposed to the scalding agent. All these signs suggest restricted motion and significant exposure time. Essential in the evaluation of scalding burns is an understanding of the time and temperature relationships of water. It is self-evident that longer durations of exposure and higher water temperatures exert the most effect on the extent of damage to tissues. This relationship is shown in Table 17.2.
forcibly in hot water, the burns take on a stocking or glove appearance, and the burns are often bilateral. Buttocks, lower back, and perineum burns occur when a child’s middle body is forcibly held under hot water. In some cases, areas are spared from scalding if these areas of skin are in contact with a relatively cooler surface such as the bottom of a tub (donut burns). In other cases, body creases are spared because apposing surfaces of skin are not exposed to the scalding agent. All these signs suggest restricted motion and significant exposure time. Essential in the evaluation of scalding burns is an understanding of the time and temperature relationships of water. It is self-evident that longer durations of exposure and higher water temperatures exert the most effect on the extent of damage to tissues. This relationship is shown in Table 17.2.
BOX 17.3 Approach to Evaluation of Cutaneous Injuries
Detailed history including mechanism of injury, identification of discrepancies between history and injuries, prior accidents, past medical history, developmental history, and family history
Complete skin examination noting location, size, shape, pattern, and color of bruises; photodocumentation
Complete physical examination including measurements for height, weight, and head circumference
Developmental history
Observation of the parent–child interaction
Appropriate laboratory examinations: May include hematocrit, hemoglobin, blood smear, and bleeding and clotting studies (platelet count, prothrombin time, partial thromboplastin time, factor V analysis)
Skeletal survey in any child under the age of 3 years in which the possibility of child abuse is being considered
Dry Contact Burns
Objects of all kinds, especially household appliances, are responsible for the lesions seen with this type of burn. The most frequent appliances are irons, hair dryers, hair curlers, cigarette lighters, light bulbs, grills from stoves or heaters, and cigarettes. Often the burn can be identified by the unique imprint of the burning agent. Cigarette burns are circular and blister early; when healed, they appear craterlike, with hyperpigmented edges. They are most frequently seen on the hands or feet, but are reported in all areas of the body. Accidental cigarette burns do occur but appear to be “brushed lesions” that are ovoid, and the resultant burns are more superficial. Nonintentional burns from the metal frames of car seats, seatbelt buckles, baby carriers, strollers, playpens, and other baby equipment, as well as burns from ashes and embers of wood and coal fires, have been implicated in dry contact burns.
TABLE 17.2. TIME-TEMPERATURE SCALE (AFTER MORITZ): EXPOSURE TIME (IN SECONDS) TO CAUSE SECOND-DEGREE BURN | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Chemical Burns
Strong acids and alkalis (lye, calcium chloride) can cause cutaneous burns or the burns can be internal if the chemical agent is ingested or placed into a body cavity.
Electrical Burns
The combination of heat and direct action of electrical forces on polarized molecules in tissue causes electrical burns. The evolution of electrical burns occurs over a longer period of time than scalding or dry contact burns. Microwave burns cause a preferential burning of tissues with high water content, such as skin and muscle. Cutaneous burns from “stun guns” have been reported, consisting of a pair of small (0.5 cm) superficial circular burns.
Bites
Human bites may be seen as a manifestation of abuse. This form of abuse, when perpetrated by an adult, is a primitive behavior and is a critical red flag when deciding about the future safety of the child in an environment where this has happened. Certain characteristics of human bites help to determine whether they are from a child or an adult. Adult bite marks usually only reach from one canine tooth to the other and only one dental arch is represented. A child’s bite usually involves both arches and the distance between the canines is usually less than 2.5 cm using dental rulers. Photographs of bite marks with a dental ruler in the picture can be extremely helpful. Dental impressions can be taken from the victim and perpetrator to match the bite marks on the skin. Saline swabs can be used to pick up saliva for ABO grouping or DNA.
Head Injuries
More fatalities and long-term morbidity are due to abusive head injury than from any other form of physical abuse. The types of abusive head injuries range from asymptomatic scalp swelling, mild to moderate bruising, and skull fracture, to intracranial bleeding, axonal injury, and brain swelling resulting in stupor, coma, and death. When a child under 3 years of age comes for medical care with a serious head injury without a readily apparent major trauma history (motor vehicle accident, falls from heights over 10 feet), the chances are high that this is an inflicted injury.
When a seriously head-injured child is being evaluated and treated medically, it is crucial that a detailed, analytical—but not challenging or accusatory—history be obtained from the caretakers. Parents who have inflicted an injury will often invent an explanation as to how the injury occurred. Thus, the skill of interviewing becomes an important foundation on which to build the diagnostic formulation. The person collecting the history should ideally be someone with experience in child abuse cases and one who does not have immediate responsibility for the medical treatment required by the child. Gentle probing, with inquiries and request for clarification on questionable portions of the history, often will reveal discrepancies between the history of the injury and the actual findings on examination. The failure to suspect inflicted neurotrauma as the cause of nonspecific signs such as irritability, lethargy, poor feeding, or vomiting may result in a missed diagnosis and risk of further trauma to the child. In one recent study, the diagnosis of abusive head trauma had been missed in nearly one-third of cases, as evidenced by the presence of old subdural collections in cases in which there was acute bleeding due to subsequent episodes of abuse.
The history of the pregnancy, labor and delivery, and neonatal course and a history of family diseases are important, with
particular attention to bleeding and clotting disorders, neurologic diseases, metabolic and bone disease, or other genetic conditions of the family. The past medical history of the child, including previous injuries and serious illnesses or hospitalizations, and a review of systems should be obtained. The social milieu with attention to the living arrangements and the relationships of household members should be explored.
particular attention to bleeding and clotting disorders, neurologic diseases, metabolic and bone disease, or other genetic conditions of the family. The past medical history of the child, including previous injuries and serious illnesses or hospitalizations, and a review of systems should be obtained. The social milieu with attention to the living arrangements and the relationships of household members should be explored.
BOX 17.4 Injuries to the Scalp
Bruises (visible externally)
Bruises (intra- and subcutaneous; not visible externally)
Lacerations
Abrasions
Subgaleal hematomas
Alopecia (hair loss secondary to hair-pulling)
Because head injuries are of such serious consequence, the general physical examination of the child with a head injury may overlook less urgently compromised organ systems. Bleeding visceral organs are the most glaring and potentially disastrous omissions, but overlooking cutaneous injuries can deprive the diagnostician of important clinical data because of the fleeting nature of these injuries. Likewise, inspection of the oral cavity for intraoral lesions and a search for hidden surface head lesions under the hair are important. The neck should be carefully inspected for signs of injury (strangulation, hand or finger bruising). The presence of bruises on the back, on the thighs, or in the perineum should also be noted. Photo documentation of such injuries is highly desirable.
The examination of the retina is of utmost importance. This should be carried out ideally by pupillary dilation and indirect ophthalmoscopy, but in lieu of that, by direct ophthalmoscopy. When possible, this should be done by a pediatric ophthalmologist and pictures should be taken of the retina.
The types of injuries in serious abusive head injury include trauma to the scalp (Box 17.4), skull fractures (Table 17.3), subdural or subarachnoid bleeding, cerebral edema, axonal injuries, parenchymal tears and contusions, and injuries to the cervical spinal cord.
Bleeding in the epidural space is usually arterial and occurs because of trauma to the overlying skull, resulting often in a skull fracture of the temporoparietal bone that tears a branch of the middle meningeal artery. The bleeding in the epidural space appears as an elliptical density on computerized tomography (CT) scan. It can accumulate rapidly and can, if not diagnosed and treated promptly, lead to coma and death. An epidural hematoma is more often nonintentional than abusive in origin, but can be seen as a consequence of abuse. Prompt medical attention and, in some cases, evacuation of the hematoma, usually results in the rapid resolution of symptoms and signs.
TABLE 17.3. FRACTURES OF THE SKULL | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Bleeding in the subdural and/or the subarachnoid spaces is due to the stretching and breaking of the veins bridging from the surface of the brain to the dural sinuses. These veins are fixed to the brain and to the dural membrane. With motion of the brain, these veins break and bleed.
Bleeding within the brain substance (parenchyma) is primarily due to trauma, a vascular or hypoxic insult to the brain itself.
Shaken Baby/Shaken Impact Syndrome
The term shaken baby syndrome has been criticized because it ascribes a clinical condition to an unwitnessed act that may or may not include impact. The arguments for and against this term are beyond the scope of this chapter, but the term is so widely used that it will be used here.
There are no reliable statistics regarding the incidence of shaken baby/shaken impact syndrome (SBS/SIS) since there are no central reporting registries to collect these data. Estimates range from 600 to 1,400 cases per year. SBS/SIS occurs in babies, usually under 1 year of age, but is also described in children considerably older. There is considerable support—clinical, confessional, and experimental—for the concept that shaking and, in many cases, impact by throwing the child against a surface and resultant deceleration are the responsible mechanical forces producing the subdural hematoma, brain injury, and consequent cerebral edema leading to raised intracranial pressure. There has been much discussion about shaking versus shaking plus impact as the mechanism for the production of the lesions seen in SBS/SIS. This began with Duhaime’s 1987 article in which she described a retrospective study of 48 cases of shaken baby syndrome seen at her institution. Of these, 62% had clinical evidence of blunt trauma to the head (bruising, skull fracture), and postmortem evidence of blunt trauma was present in all of the fatal cases. In this report, she also studied the forces generated when three types of dolls were shaken. Using a strain gauge measuring forces during shaking, she was unable to demonstrate enough force from shaking to account for the extent of damage seen in clinical cases. She concluded that impact with rapid deceleration of the intracranial contents was necessary for these lesions. This discussion has continued, with some investigators citing the absence of evidence of impact in a substantial number of their reported cases. The criticism of the theory that impact is required cites the crudeness of the doll models used in Duhaime’s study and the fact that no good data exist to inform us about what magnitude of forces are required to injure the infant brain. There are currently ongoing biomechanical studies to try to determine the required forces to produce the classic clinical, radiographic, and pathologic changes due to inflicted childhood neurotrauma. The absence of factual information about the characteristics of all of the structures in the live infant’s head inhibits this effort, but attempts are being made, through biomechanical and animal models, to learn more.
Interviews with confessed perpetrators indicate that the usual trigger for these assaults is inconsolable crying by the infant. Frustrated by attempts to stop the crying, the perpetrator loses control and seizes the infant, either by the chest, under the arms, by the arms, or by the neck, and violently shakes the baby, followed by throwing the baby onto a hard or soft surface. The time of the shaking varies, usually ranging from around 5 seconds to 15 or 20 seconds. It has been estimated by video recordings of a person shaking a doll that the number of shakes ranges between two to four per second. During the
shaking, the head rotates wildly on the axis of the neck, creating multiple forces within the head. The infant stops crying and stops breathing during the shaking, causing decreased oxygen supply to the body, particularly the brain. Recent reports that the respiratory center may be damaged during these traumatic events, leading to dysfunctional respiratory efforts after the shaking has stopped, would partially explain the hypoxic changes seen in the brains of infants who succumb. The infant brain, with much higher water content than the adult brain, is much softer than an adult brain, having the consistency of gelatin. The absence of myelination contributes to the relative softness. These factors make the brain more easily distorted and compressed within the skull. Shaking and the sudden deceleration of the head at the time of impact do several things:
shaking, the head rotates wildly on the axis of the neck, creating multiple forces within the head. The infant stops crying and stops breathing during the shaking, causing decreased oxygen supply to the body, particularly the brain. Recent reports that the respiratory center may be damaged during these traumatic events, leading to dysfunctional respiratory efforts after the shaking has stopped, would partially explain the hypoxic changes seen in the brains of infants who succumb. The infant brain, with much higher water content than the adult brain, is much softer than an adult brain, having the consistency of gelatin. The absence of myelination contributes to the relative softness. These factors make the brain more easily distorted and compressed within the skull. Shaking and the sudden deceleration of the head at the time of impact do several things:
The veins that bridge from the brain to the dura, which is fixed to the inside of the skull, tear open and bleed, creating the subdural hematoma or subarachnoid hemorrhages so characteristic of the syndrome.
There is internal commotion in the brain as well as movement of the brain within the skull, causing direct trauma to the brain substance itself.
Axons are injured, shearing off during the commotion to the brain.
The lack of oxygen during and after the assault causes further irreversible damage to the brain substance.
Damaged neurons release excitatory amines that cause vasospasm, adding to the oxygen deprivation in the brain and destruction of adjacent neurons.
The combined effect is massive destruction of the brain tissue, causing immediate brain swelling and enormous increases in intracranial pressure. This causes compression of the blood vessels, thereby decreasing the oxygen supply to the brain even further. It is these insults to the brain, not the subdural or subarachnoid bleeding, that cause the signs, symptoms, clinical and radiographic findings, and course of SBS/SIS.
Associated Injuries in Shaken Baby Syndrome—Retinal Hemorrhages
There are several theories about the cause of retinal hemorrhages (RHs). The first holds that increased intracranial pressure causes RHs. The chief argument against this theory is that RHs occur much less frequently in nonintentional head injuries than in those resulting from shaking despite the fact that both have increased intracranial pressure. In a recent study of head injuries from a variety of causes, both abusive and accidental, RHs were seen in only 2% of a group of 233 accidentally head-injured children under the age of 6 years and in 33% of the children with inflicted head injury.
The second theory postulates that RHs are due to a disruption of the layers of the retina. There are ten layers in the retina, all richly supplied with blood vessels. Proponents of this theory state that when these layers are subjected to the lines of force associated with shaking, they slide across one another, shearing these vessels so that they bleed. This would explain why the RHs unique to SBS/SIS are flame-shaped or dot/blot as the blood tracks between the layers of the retina. RHs seen in SBS/SIS are usually extensive in distribution in the retina, are not confined to the posterior pole, are numerous, and involve multiple layers of the retina. RHs seen in other conditions are usually closer to the surface, so-called preretinal hemorrhages, and resolve quickly (Box 17.5).
Although retinal hemorrhages are the most commonly found ocular lesion in SBS/SIS, other lesions may also be seen. These include retinal detachment, optic nerve injury, retinal folds, and cupping of the optic nerve secondary to raised intracranial pressure. Although RHs are not pathognomonic of inflicted head trauma, they are present in a high percentage of abuse cases and are not present in most accidental traumas, after cardiopulmonary resuscitation, or after seizures. Other associated injuries may include bruising and/or skeletal injuries such as posterior rib fractures and classic metaphyseal lesions of the long bones. These should be sought by skeletal survey.
BOX 17.5 Differential Diagnosis of Retinal Hemorrhages
Vaginal delivery: Occurring in 40% of children delivered vaginally, these fine petechial preretinal hemorrhages usually resolve within 10–14 days of delivery and resolve spontaneously, leaving no residuals.
Bleeding disorders: Isolated retinal hemorrhages in coagulopathies have not been described. When they occur, they are in association with other sites of bleeding.
Arteriovenous malformations: Extremely rare in infancy
Increased intracranial pressure: Present in most cases of serious childhood neurotrauma, both from nonintentional and inflicted injuries
Bacterial meningitis: Even when bacterial meningitis was common (before vaccines made this a rare disease), the incidence of retinal hemorrhage in meningitis was only seen in 1% of cases. With the rarity of bacterial meningitis in clinical pediatrics in this era, this cause for retinal hemorrhage would be extraordinarily rare. It is also not likely that meningitis would not be diagnosed by clinical assessment and culturing and examination of cerebrospinal fluid.
Accidental head trauma: Recent literature on the incidence of retinal hemorrhages in nonintentional head trauma indicates their rarity in these cases.
Clinical Manifestations of Shaken Baby Syndrome
Symptoms and physical findings are variable depending on the length and severity of the shaking and whether the infant was thrown onto a surface. The syndrome can be seen as a continuum from a short duration of shaking with little or no impact, to severe, prolonged shaking and major impact (Fig. 17.1). All of the symptoms are caused by axonal damage from trauma and/or hypoxia, diffuse or focal cerebral edema, and resultant increased intracranial pressure. In moderate to severe cases, the signs and symptoms begin almost immediately after the shaking and reach their peak within 4 to 6 hours.
Diagnosis of Abusive Head Trauma
Laboratory Studies
Children with head trauma severe enough to be admitted to the hospital should also have laboratory studies to support diagnoses of associated trauma in other organ systems, to anticipate hematologic and biochemical alterations sometimes attendant to head trauma, and also to seek for the manifestations of their neurologic status. These studies are displayed in Box 17.6.
One study examining coagulopathy in pediatric abusive head trauma found that there were prothrombin time prolongations in 54% of patients with parenchymal damage and in 20% of those without demonstrable parenchymal damage. Other coagulation markers (partial thromboplastin time, platelet counts, and fibrinogen levels) were also altered. The authors hypothesize that these abnormalities in coagulation elements are due to tissue factor release from damaged parenchymal cells, which, when complexed with factor VII, activate coagulation via the extrinsic pathway, leading to disseminated intravascular coagulation.
Imaging Studies
In most instances of moderate to severe head injury, the first imaging modality should be CT head scans without contrast for evaluation of the intracranial structures. It is readily available in most hospitals and can be performed safely with life support systems operating during the procedure. Bone windows should be employed along with the standard scan. Plain radiographs of the skull will usually show existing skull fractures better than CT will. Magnetic resonance imaging (MRI) is ordinarily used as a confirmatory test rather than an initial one due to the longer scan times and need for life support, but MRI gives superior detail in showing parenchymal changes and smaller subdural hematomata.
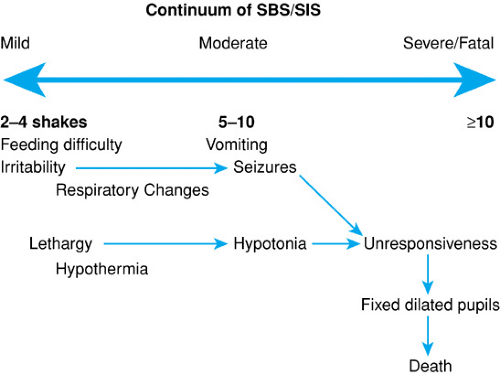 FIGURE 17.1. Conceptual model of the “dose response” in shaken baby/shaken impact syndrome (SBS/SIS). |
Skeletal surveys are recommended in serious head trauma since the diagnosis of abuse may be made or supported if unsuspected or occult traumatic injuries are found in other parts of the appendicular skeleton. Such accompanying skeletal fractures are seen in roughly half of the cases of abusive head injury. Posterior rib fractures are present in some cases of shaken infants and may be seen acutely with bone scintigraphy or by follow-up thoracic films in 10 to 14 days to see callus formation at the site of these fractures.
BOX 17.6 Laboratory Examinations in Inflicted Childhood Neurotrauma
Complete blood count with morphology
Serial hematocrits
Serum electrolytes, BUN, creatinine, serum and urineosmolality
Urinalysis
AST, ALT, alkaline phosphatase
Creatine phosphokinase (CPK)
Cultures of blood, urine, cerebrospinal fluid (if safe toperform lumbar puncture)
PT, PTT, TT, platelet count, fibrinogen, and FDP
Stool for blood
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


