Women’s health concerns
Pregnancy
Post-partum state
Hormonal contraceptive or replacement therapy
Thrombophilia
Deficiency of antithrombin 3 and protein C and S
Factor V Leiden and prothrombin gene mutation
Antiphospholipid antibodies
Hyperhomocysteinaemia
Infection
Puerperal sepsis, episiotomy or wound infections
Localised infections such as otitis, mastoiditis, sinusitis
Meningitis
Systemic infectious disorders
Chronic inflammatory diseases
Vasculitis
Inflammatory bowel disease
Cancer
Leukaemia
Hematologic disorders
Sickle cell anaemia
Polycythaemia
Essential thrombocytosis
Paroxysmal nocturnal haemoglobinuria
Trauma
Head trauma
Local injury to cerebral sinuses or veins
Jugular venous cannulation
Neurosurgical procedures
Lumbar puncture
Nephrotic syndrome
Pathogenesis
The human brain has a unique cerebral venous system. It has sinuses which are lacking in muscular walls or valves and hence do not have the ability to contract. The sagittal sinuses (superior and inferior) drain into transverse, cavernous, right and left sigmoid sinuses and finally into the internal jugular vein. In susceptible patients, blood can pool, clot and obstruct these sinuses, leading to increased intracranial pressure and cytotoxic and vasogenic oedema of variable degree, which can progress to intracerebral bleeding, ischaemia and infarction (Fig. 23.1). Pathological findings observed in central nervous system as a result of CVT are determined by:
Fig. 23.1
Pathophysiology of cerebral venous thrombosis. CSF indicates cerebrospinal fluid
(a)
Underlying disease pathology
(b)
Nature of sinus/cerebral vein involved
(c)
Interval between the onset and pathological examination
Cortical vein thrombosis usually presents as a cord-like swelling with minimal or absent haemorrhagic infarction of the brain [14]. This discrepancy has been explained on the presence of frequent intercommunications between various cortical veins and sinuses. In case of superior sagittal sinus thrombosis, the sinus is distended and appears blue. Cortical veins are also swollen and may rupture at some places giving rise to haemorrhagic infarction and even intracerebral haemorrhage. In an occasional case, haemorrhagic infarction may appear on the other side due to occlusion of opposite cortical vein (parasagittal). In deep cerebral vein thrombosis, white matter may be involved, e.g. basal ganglia, thalamus, etc. In due course, thrombosis gets recanalised and organised and may even disappear in majority of cases. Cerebral oedema with or without increased intracranial hypertension is a frequent finding in early stage. It may even lead to transtentorial herniation with notching of uncus of temporal lobe [15]. Microscopy shows typical changes of haemorrhage, but specific feature appears to be ‘profuse leukocyte invasion’ because of patent arteries allowing inflow.
The terminology used and the clinical presentation will vary on the location and extent of the thrombosis. In pregnant women, the common sites are thrombosis of the sagittal sinus with extension into the cortical veins or primary thrombosis of a cortical vein [16].
Clinical Features
Clinical presentation can be varied depending on the site and extent of thrombosis (Fig. 23.2). CVT often has an insidious onset, though rarely it can present as an acute episode of sudden neurological illness. The most consistent symptom is unrelenting headache, not responding to analgesia and may be progressive over several days. It may be accompanied by nausea and vomiting. Neurological signs of focal seizures, focal neurological deficits and generalised seizures are sometimes seen. Visual impairment, blurring of vision, diplopia and blindness can result from very high intracranial pressure and papilloedema [17]. When the deep cerebral venous system of thalami is involved, behavioural symptoms such as lethargy, dementia, amnesia, mutism and coma can develop, undoubtedly reflecting a graver prognosis [18].
Fig. 23.2
Major clinical syndromes according to location of cerebral venous thrombosis
The common differential diagnosis is eclampsia. It is differentiated by presence of hypertension and proteinuria, clinical course of pregnancy and delivery, response to treatment and results of brain imaging. The other confusing situation is the postdural puncture headache if spinal anaesthesia is used for delivery [19]. Spinal headache resolves with hydration and posture and has no neurological deficits. Posterior reversible encephalopathy syndrome (PRES), occurring as a squeal to hypertension and eclampsia in recently delivered women, presents as mental confusion, headache, seizures and visual impairment but no neurological deficits. It is diagnosed on MRI, seen characteristically as hyperintensities on T2-weighted images as distinct from CVT.
Diagnosis
The confirmation of a diagnosis of dural venous sinus thrombosis is reliant on demonstration of the thrombus by neuroimaging. The initial evaluation during pregnancy begins with a brain computerised tomography (CT) without contrast. Signs of cerebral venous thrombosis on CT include hyperdensity in the area of a sinus or cortical vein (cord sign) and filling defects, especially in the superior sagittal sinus (empty Δ sign), in contrast-enhanced studies [20]. A partially filled posterior segment of the superior sagittal sinus is seen (empty delta sign) (Fig. 23.3), but this is found only in 20 % of cases [2]. It is seen on axial CT images and represents enhancement with i.v. contrast of the wall of the posterior sagittal sinus, outlining the clot within the lumen anteriorly.
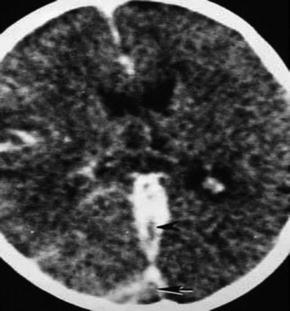
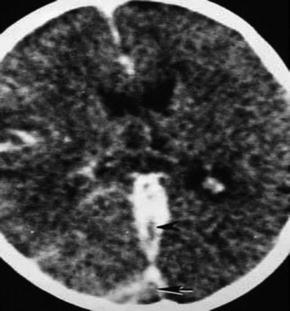
Fig. 23.3
Axial head CT scan demonstrating cerebrovenous thrombosis of the straight sinus (arrowhead) and the empty delta sign (arrow)
Conventional CT can be entirely normal in the presence of CVT and miss the diagnosis in 60 % of cases. The most sensitive non-invasive technique is magnetic resonance imaging (MRI) with MR venography (Fig. 23.4) and is the investigation of choice for demonstrating CVT, as it may exclude significant alternative diagnoses and will also demonstrate cerebral venous infarction complicating cerebral venous occlusion. Difficulties in diagnosis arise due to unusual normal anatomical variants and cases where there is near occlusion of the venous sinus. T1-weighted and T2-weighted images can identify the thrombosed sinuses if done within 5 days of the event and are currently the test of choice [21, 22]. CT venography is the new technique that can provide better details and in experienced hands will show dilated ‘corkscrew’ veins with thrombosis [23].