▪ INTRODUCTION
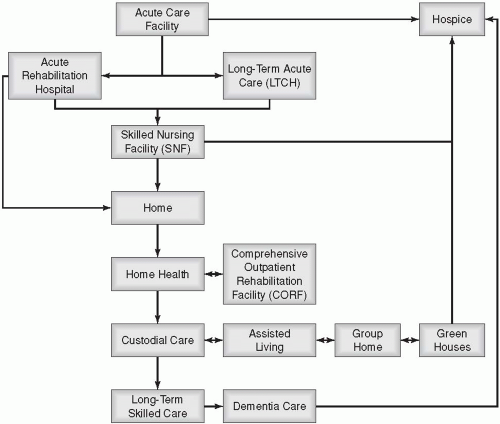
A. This chapter discusses post-acute levels of care, from acute rehabilitation hospitals, to nursing homes, to “aging in place” (
Fig. 6-1).
B. Most of the frail elderly in the United States require at some point or another long-term care or rehabilitation services in acute or sub-acute care facilities. This is mostly due to deconditioning post-acute care hospitalization.
C. Today’s elderly patients who seek health care services encounter a variety of providers and organizations, including primary care physicians, specialists, acute care hospitals, skilled nursing facilities (SNFs), nursing homes, rehabilitation facilities, and home health care.
D. Assessment for placement of the client/patient in a specific level of care should:
Yield the least restrictive level of care possible for safe care;
Be financially feasible and sustainable for the patient/client/family;
Meet the conditions stipulated in either laws and regulations or insurance policies; and
Ensure a reimbursable episode of care.
E. Health insurance plans usually pay for “medically reasonable and necessary” care. However, each insurance company has its own rules and definitions of “medical necessity” and “skilled” versus “unskilled” services that play an integral role in deciding whether to reimburse for care or not.
F. The prospective payment system (PPS) has resulted in patients’ early discharge from the acute care/hospital setting. This has increased the need for follow-up care in settings such as the home, but most commonly in the long-term care and rehabilitation settings.
G. As integrated care delivery systems have become more common, new approaches to care, especially for the elderly, disabled, or functionally impaired, have been created. A common approach is sub-acute care,
which is a level of care that blends acute and long-term care skills and philosophies (
Carr, 2000).
H. Recent changes in health care delivery systems have resulted in an increased demand for case management and the role of the case manager in settings beyond the acute care/hospital; i.e., long-term care and rehabilitation.
I. Care of the elderly requires the services of a multidisciplinary team of health care professionals including geriatricians, nurses, social workers, dieticians, physical therapists, occupational therapists, speech and language therapists, and pharmacists, but especially case managers.
J. To ensure effective care of the elderly, the multidisciplinary team must focus on the following:
Functional and medical assessments to develop a full understanding of the elderly patient’s needs
Physical and mental status examination
Balance and gait test
Dietary assessment
Psychosocial history and support system
Home safety
Battery of laboratory and x-ray (radiologic) tests as necessary
Other tests as indicated by the elderly patient’s condition
K. Care for the aged, chronically sick, and mentally ill has been affected by specific milestones in laws and regulations in the United States.
Almshouses: institutions to house the poor, aged, and mentally ill; regulation in 1873.
County homes: result of regulation; historically, terrible conditions for the older adult.
1935—Social Security Act: provided catalyst for privately funded institutions for the aged.
1965—Medicare and Medicaid reimbursement: allowed expansion of this industry.
1965—Older Americans Act: created primary vehicle for organizing, coordinating, and providing community-based services and opportunities for older Americans and their families.
Office of Nursing Home Affairs of 1971 and Nursing Reform Act of 1987: established minimum requirements for nursing assistants, created a resident rights statement, and implemented a single standard for 24-hour care for all residents in nursing homes.
▪ KEY DEFINITIONS
A. Activities of daily living (ADLs)—Activities related to personal care and include bathing or showering, dressing, getting in or out of bed or a chair, using the toilet, and eating. If a person has any difficulty performing an activity by himself or herself and without special equipment, or did not perform the activity at all because of health problems (physical, mental, or emotional), the person is categorized as having a limitation in that activity. The limitation may be temporary or chronic.
B. Aging in place—Process by which a person chooses to remain in his or her living environment (home) and to remain as independent as possible despite the physical or mental decline.
C. Assisted living—A type of living arrangement in which personal care services such as meals, housekeeping, transportation, and assistance with activities of daily living are available as needed to people who still live on their own in a residential facility. In most cases, the assisted living residents pay a regular monthly rent and an additional fee for the services they receive.
D. Comprehensive outpatient rehabilitation facility (CORF)—A facility that provides coordinated outpatient diagnostic, therapeutic, and restorative services, at a single fixed location, to outpatients for the rehabilitation of injured, disabled, or sick individuals.
E. Continuing care retirement community (CCRC)—A housing community that provides different levels of care based on what each resident needs over time. This is sometimes called
life care and can range from independent
living in an apartment, to assisted living, to full-time care in a nursing home. Residents move from one setting to another based on their needs but continue to live as part of the community. Care in CCRCs is usually expensive. Generally, CCRCs require a large payment before an individual moves in, and then a certain monthly fee.
F. Custodial care—The provision of services that can be safely and reasonably given by individuals who are neither skilled nor licensed medical personnel. These may include personal care, such as help with activities of daily living (bathing, dressing, eating, getting in or out of a bed or chair, moving around, and toileting). It may also include care that most people do themselves, like administering eye drops. In most cases, Medicare does not pay for custodial care.
G. Custodial care facility—A facility that provides room, board, and other personal assistance services, generally on a long-term basis, which does not include a medical component.
H. Independent living—A service delivery concept that encourages the maintenance of control over one’s life based on the choice of acceptable options that minimize reliance on others performing everyday activities.
I. Inpatient rehabilitation facility (IRF)—A free-standing rehabilitation hospital or rehabilitation unit(s) in an acute care hospital that provides intensive rehabilitation programs; patients who are admitted to such facilities must be able to tolerate 3 hours of intense rehabilitation services per day.
J. Instrumental activities of daily living (IADLs)—Activities related to independent living, including preparing meals, managing money, shopping for groceries or personal items, performing light or heavy housework, and using a telephone. If a person has any difficulty performing an activity by himself or herself and without special equipment, or does not perform the activity at all because of health problems, the person is categorized as having a limitation in that activity. The limitation may be temporary or chronic.
K. Limitation of activity—Refers to a long-term reduction in a person’s capacity to perform the usual kind or amount of activities associated with his or her age group due to a chronic condition. This may include a limitation in activities of daily living, instrumental activities of daily living, play, school, work, difficulty in walking or remembering, or any other.
L. Long-term care—A variety of services that help people with health or personal needs and activities of daily living over a period of time. Long-term care can be provided at home, in the community, or in various types of facilities, including nursing homes and assisted living facilities. Most long-term care is custodial care, which few (if any) insurance companies will pay for if skilled care is also not required.
M. Long-term care insurance—A private insurance policy to help pay for some long-term medical and nonmedical care. Some long-term care insurance policies offer tax benefits; these are called tax-qualified policies.
N. Non-covered services—These services are not considered skilled and do not meet the requirements of a Medicare benefit category, are statutorily excluded from coverage on grounds other than 1862(a)(1), or are not considered reasonable and necessary under 1862(a)(1).
O. Nursing facility—See skilled nursing facility (SNF).
P. Nursing home—A residence that provides individuals with a room and meals, and assists with activities of daily living and recreation. Generally, nursing home residents have physical or mental problems that keep them from living on their own. They usually require daily assistance.
Q. Occupational therapy (OT)—Structured activity focused on activities of daily living skills (feeding, dressing, bathing, grooming), arm flexibility and strengthening, neck control and posture, perceptual and cognitive skills, and using adaptive equipment to facilitate activities of daily living.
R. Outpatient care—Medical or surgical care that is provided in a clinic/ambulatory setting and does not include an overnight hospital stay.
S. Personal care services—Nonskilled assistance (bathing, dressing, light housework) provided to individuals in their homes.
T. Physical therapy (PT)—Structured activity focused on mobility skills (bed and chair transfers, wheelchair use, walking), leg flexibility and strengthening, trunk or gait control and balance, endurance training, and use of adaptive equipment to facilitate mobility and physical functioning.
U. Reasonable and necessary care—Health care or services that are required by Medicare recipients and that is considered important for their medical condition. The Medicare program generally covers only items or services that are “reasonable and necessary” for the diagnosis or treatment of illness or injury, or “to improve the functioning of a malformed body member.” This “reasonable and necessary” language is the basis for most Medicare coverage policies, but its meaning remains ill defined and controversial.
V. Rehabilitation—A restorative process through which an individual with a complex, chronic, or terminal illness develops and maintains self-sufficient functioning consistent with his/her capability. Usually provided by licensed health care professionals such as nurses and physical, occupational, and speech therapists.
W. Respite care—Temporary or periodic care provided in a nursing home, assisted living residence, or other type of long-term care program so that the usual caregiver can rest or take some time off.
X. Restorative nursing services (NRS)—Replication of activities initiated by a physical therapist (PT), occupational therapist (OT), or a speech-language pathologist (SLP) and then performed and maintained by the nursing staff. These may include services such as range of motion exercises, dressing, personal hygiene, walking, and feeding.
Y. Skilled care—The provision of services that can be given only by or under the supervision of skilled and licensed medical personnel/health care professionals; that is, skilled and competent staff such as registered nurses; social workers; physical, occupational, and speech therapists; rehabilitation counselors; and registered dietitians/nutritionists. These staff are required to manage, observe, and evaluate the skilled care activities.
Z. Skilled nursing care—A level of care that includes services that can only be performed safely and correctly by a licensed nurse (either a registered nurse or a licensed practical nurse).
AA. Skilled nursing facility (SNF)—A facility (which meets specific regulatory certification requirements) that primarily provides inpatient skilled nursing care and related services to patients who require medical, nursing, or rehabilitative services but does not provide the level of care or treatment available in a hospital.
BB. Skilled nursing facility care—A level of care that requires the daily involvement of skilled nursing or rehabilitation staff. Examples of skilled nursing facility care include intravenous injections, wound care, and physical therapy. The need for custodial care (for example, assistance with activities of daily living, like bathing and dressing) cannot, in itself, qualify for Medicare coverage in a skilled nursing facility.
CC. SNF Co-insurance—For day 21 through 100 of extended care services in a benefit period, a daily amount for which the beneficiary is responsible, equal to one-eighth of the inpatient hospital deductible.
DD. Speech and language pathology (SLP)—Structured activity focused on communication skills, perceptual and cognitive skills, and swallowing.
▪ LONG-TERM CARE
A. Long-term care is necessary when individuals require someone else to help them with their physical and/or emotional needs. This help may be required for many of the activities or needs healthy and active people take for granted.
B. Long-term care and assistance may be necessary as a result of a terminal condition, disability, illness, injury, or merely old age.
C. The need for long-term care may last for a few weeks, months, or years. The length of time needed depends on the underlying reasons and medical/health condition.
D. Long-term care may take the form of temporary or ongoing care.
Temporary long-term care—Need for care for a limited period of time, usually for only a few weeks or months. This may take place to address the following conditions:
Ongoing long-term care—Need for care for an extended period of time, usually many months or years. This may take place to address the following conditions:
E. Long-term services are provided in varied care settings such as:
F. Case management in the home care setting is discussed in
Chapter 5 and case management in the palliative care and hospice settings is discussed in
Chapter 7. Other settings are discussed in this chapter.
G. Health care services provided in the long-term care settings are of two types: custodial and skilled (
Day, 2006).
Custodial services
The provision of services that can be safely and reasonably given by individuals who are neither skilled nor licensed medical personnel.
Services may include personal care such as help with ADLs (bathing, dressing, eating, getting in or out of a bed or chair, moving around, and toileting). It may also include care that most people do themselves, like administering eye drops.
In most cases, Medicare does not pay for custodial care, unless it is provided in combination with skilled services and as part of a skilled plan of care.
Custodial care may include any or all of the following:
Walking
Bathing, personal hygiene, and grooming
Dressing
Feeding and providing meals
Toileting and helping with incontinence
Managing pain
Preventing unsafe behavior such as wandering around aimlessly
Providing comfort and assurance
Providing physical or occupational therapy
Attending to medical needs
Counseling
Answering the phone
Meeting doctors’ appointments
Maintaining the household
Shopping and running errands
Providing transportation
Administering medications
Managing money
Paying bills
Doing the laundry
Writing letters or notes
Maintaining a yard
Removing snow
The individual who requires custodial services is someone who:
Can no longer perform daily tasks necessary to maintain health and safety
Cannot safely perform ADLs or preserve health from further decline
By choice or circumstance has decided to reside in the nursing home as primary residence
Receives nonskilled physical therapy services (restorative nursing by nursing assistants) to maintain function
Skilled services
The provision of services that can be given only by or under the supervision of skilled and licensed medical personnel/health care professionals; that is, skilled and competent staff such as registered nurses, social workers, physical, occupational, and speech therapists, rehabilitation counselors, and registered dietitians/nutritionists.
Members of the professional staff are required to manage, observe, supervise, and evaluate the skilled care activities.
Skilled care activities may include the following:
Monitoring vital signs
Ordering medical tests
Diagnosing problems
Administering intravenous medications
Administering intravenous fluids/nutritional support
Dispensing medications, including injections
Drawing blood
Wound care and dressing changes
Psychosocial counseling and therapy
Physical therapy and exercise
Occupational therapy
Speech therapy
The individual who requires skilled services is someone who:
May have exhausted Medicare Part A benefit period or is not eligible for benefits
Can no longer care for himself or herself
Requires assistance in ADLs, IADLs, taking medication, or skilled treatments
H. Skilled and custodial services do not refer to a specific type of long-term care services; rather, they are referred to based on the people who deliver/provide the care—not the actual care given. The main differentiating factor between these two terms is the employment of 1) skilled versus nonskilled, and 2) licensed versus unlicensed providers (
Day, 2006).
I. Generally, skilled care is available only for a short period of time after a hospitalization. Custodial care is for a much longer period of time. Sometimes both levels of care are provided in the same facility (e.g., nursing home) and the patients (usually called residents) may transfer between levels of care within the facility without having to move from one room or unit into another.
J. A skilled and licensed care provider can provide custodial services; however, a nonskilled and unlicensed provider cannot provide skilled services. In rare situations, skilled services such as blood pressure monitoring, administering medications, or changing wound dressings may be given by a custodial care provider.
K. A long-term care treatment plan usually includes skilled and custodial services (care activities), goals, and expected outcomes. It addresses the following:
Applied therapies
Frequency of the therapies consistent with goals and expected outcomes
Potential for patient’s restoration and prognosis
Time frame in which the physician/provider prescribing the treatment will review the plan and evaluate medical necessity and progress
Maintenance, palliative relief, or measures to be implemented to prevent deterioration in the patient’s status
L. Medicare pays for skilled care. Custodial care is covered under Medicare if it is provided in a skilled care setting and under a skilled plan of care.
M. Medicare and other health insurance plans pay for the care of patients with certain acute medical needs where recovery is anticipated. Patients with chronic medical problems are usually covered under Medicaid.