Fig. 1
PA radiograph of a skeletally immature wrist in a 10-year-old male patient demonstrating a scaphoid fracture. The distance between the scaphoid and lunate is apparently widened due to the proximal pole not yet being ossified. The scapholunate ligament was found to be intact and uninjured upon direct inspection at the time of surgical treatment
All of the carpal bones are completely cartilaginous at birth. The ossification center of the capitate is the first to appear and is usually visible by the third or fourth month of life. This is followed very closely by the hamate ossific nucleus. The triquetrum begins to ossify next between 7 months and 2 years of age. Subsequently, the lunate becomes visible between 3 and 4 years of age. The trapezium, trapezoid, and scaphoid all begin to ossify around the same age, between 3 and 6 years. The last ossific nucleus to appear is that of the pisiform, around 8–12 years of age. Completion of the carpus ossification process occurs between 8 and 12 years of age (Hsu and Light 2006).
Assessment of Carpal Fractures
Signs and Symptoms
Children generally present following a fall onto an outstretched arm. Additionally, sports and other extracurricular activities are common mechanisms of injury. Children may complain of pain; however, they may be more stoic than adults. A hesitance to report an injury or pain to their parents or other authority figures may be present as a result of their desire to continue playing a sport.
A thorough evaluation of wrist and digital range of motion is necessary as well as an evaluation of the entire extremity in order to identify any potential concomitant areas of injury. Swelling and ecchymosis are usually present in the region of the carpus. Tenderness to palpation overlying the injured area is common, and the wrist range of motion may be limited due to pain and/or swelling. It is important to perform a thorough neurovascular exam in order to identify any deficiencies as children may not readily describe neurologic complaints to the treating physician due to unfamiliarity with the sensation, a lack of recognition of its importance in the evaluation, or difficulty in describing it accurately.
Nafie specifically looked at clinical signs and symptoms present in pediatric carpal fractures . In these patients, the most common signs of a carpal fracture included dorsal wrist swelling, tenderness in the anatomical snuffbox and/or over the distal radius, and painful extension of the wrist and/or thumb (Nafie 1987).
Imaging and Other Diagnostic Studies
Plain radiographic evaluation of potential carpal fractures should include standard posteroanterior (PA) and lateral views centered on the wrist. If there is a high suspicion of a scaphoid fracture based on physical examination, then the addition of two other dedicated wrist views is indicated, including an oblique view and a PA view of the wrist in ulnar deviation. Initial radiographs can be negative for any appreciable fracture; however, an underlying fracture may be present. Therefore, immobilization is reasonable as an initial treatment form in patients who demonstrate clinical signs and symptoms consistent with a fracture even in the setting of normal initial radiographs. Reexamination clinically in conjunction with repeat plain radiographs should be performed 2–3 weeks following the injury to look for a fracture when it may become more obvious radiographically. MRI can be helpful in diagnosing an occult carpal fracture as well, particularly in the immature wrist (Nafie 1987).
Injuries Associated with Carpal Fractures
Distal radius fractures are the most common injury associated with carpal fractures in the pediatric population (Gholson et al. 2011). The combination of a scaphoid and distal radius fracture is most common (Fig. 2); however, fractures of the lunate and pisiform have also been reported in association with distal radius fractures in children (Anz et al. 2009).


Fig. 2
A 14-year-old male fell onto an outstretched hand while playing basketball sustaining a displaced physeal fracture of the distal radius with a minimally displaced scaphoid waist fracture
In addition, fracture of the scaphoid has been reported in association with a fracture of the capitate , the so-called scaphocapitate syndrome (Anderson 1987). Injuries to the scapholunate and lunatotriquetral interosseous ligaments are quite rare in the pediatric population (Zimmerman and Weiland 1990).
Classification
Classification of pediatric scaphoid fractures is most commonly based on the anatomic location of the fracture, as in the adult population: avulsion distal pole, transverse distal pole, waist and proximal pole (Fig. 3) (Anz et al. 2009). Fractures are further classified as displaced or undisplaced. Additionally, scaphoid fractures in children can be classified based on the amount of ossification present. Type I fractures are purely chondral, occurring in children less than 8 years of age. The fracture line may be purely chondral or involve part of the ossific nucleus. These chondral fractures require MRI for diagnosis. Type II fractures are osteochondral in nature and occur in children 8–11 years of age. Lastly, type III fractures are osseous in nature. These are the most common type, occurring in children 12 years of age or older. No classification system exists specific to fractures of the other carpal bones in the pediatric population (Anz et al. 2009).
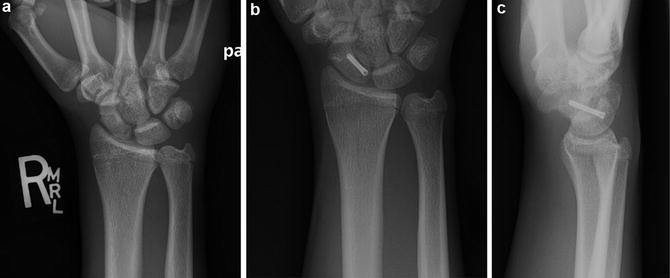
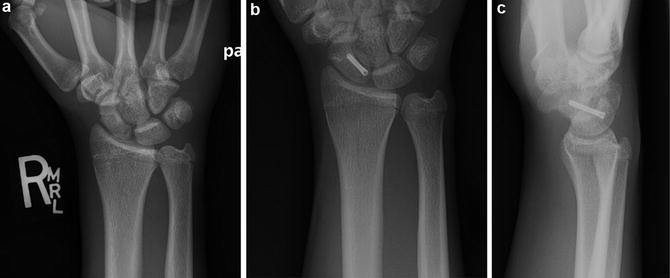
Fig. 3
(a) A nearly skeletally mature 16-year-old male with a proximal pole fracture of the scaphoid after a fall onto an outstretched hand. (b and c) Patient was treated via an open dorsal approach with a small headless compression screw resulting in successful union
Treatment Options
Nonoperative Management
Indications
Nonoperative management is the most commonly utilized method of treatment of pediatric carpal fractures . Observed immobilization is indicated in patients with closed nondisplaced carpal injuries without joint subluxation or dislocation. Most carpal fractures in skeletally immature patients require a short period of below the elbow immobilization ranging from 4 to 6 weeks. In skeletally mature patients and adolescents with carpal fractures, the immobilization time needed for bony union is more similar to that seen in adults requiring between 6 and 12 weeks.
Contraindications
Nonoperative treatment is contraindicated in open, displaced, or unstable carpal fractures or in the setting of joint subluxation or dislocation (Table 1).
Table 1
Noperative Treatment of Pediatric Carpal Fractures
Indications | Contraindications |
|---|---|
Undisplaced, stable fracture | Displaced, unstable, or open fracture |
No joint subluxation or dislocation | Joint subluxation or dislocation |
Operative Treatment
Indications
Indications for operative treatment of carpal fractures in the pediatric population include open fracture, displacement, fracture instability, associated joint subluxation or dislocation, associated neurovascular compromise, associated compartment syndrome, and established nonunion of the fracture. The scaphoid is the most commonly fractured bone treated operatively in the pediatric population. Specifically for scaphoid fractures in pediatric patients at or near skeletal maturity, operative treatment should be considered if fracture displacement is greater than 1 mm, the fracture is comminuted or involves the proximal pole, there has been a delay in diagnosis and initial treatment, or the intrascaphoid angle is greater than 45° on the lateral view (Anz et al. 2009).
Contraindications
It is important to remember that the large majority of pediatric carpal fractures are treated nonoperatively with simple cast immobilization. Closed, stable, undisplaced carpal fractures without evidence of joint instability should be treated with cast immobilization and followed with routine radiographs to ensure displacement does not occur. It should be noted that late displacement in this setting is extremely rare (Table 2).
Table 2
Operative Treatment of Pediatric Carpal Fractures
Indications | Contraindications |
|---|---|
Displaced, unstable, or open fracture | Undisplaced, stable fracture |
Joint subluxation or dislocation | No joint subluxation or dislocation |
Failure to heal with adequate period of immobilization |
Scaphoid Fractures
Scaphoid fractures are the most commonly seen fractured bone in the immature carpus representing 2.9 % of hand and wrist fractures seen in children (Light 2000). The incidence of scaphoid fractures peaks around 15 years of age in the skeletally immature population. The mechanism of injury is usually a fall onto an outstretched hand with the wrist extended. As previously mentioned, initial plain radiographs may not reveal a fracture. In clinically suspicious cases, radiographs should be repeated in 2–3 weeks while immobilizing the patient in the interim. The fracture can become more obvious radiographically at this time. Occasionally, MRI is used to confirm the diagnosis.
Historically, the most commonly fractured area in the skeletally immature scaphoid is the distal pole which is quite different from that seen in adults with scaphoid fractures. This is likely due to the eccentric ossification pattern seen in childhood. Adolescents, however, do commonly demonstrate the classic mid-waist pattern of scaphoid fracture as seen in adults. Historically, up to 87 % of fractures in the pediatric scaphoid are undisplaced and involve the distal pole (Wulff and Schmidt 1998). These fractures are amenable to successful nonoperative treatment with 4–6 weeks of cast immobilization. A short-arm thumb spica cast is usually sufficient immobilization in this setting to result in fracture healing. Undisplaced waist fractures in this population may require a slightly longer immobilization period of 7–8 weeks to achieve healing (Elhassen and Shin 2006).
Waters and Bae et al. found that male sex, high-energy mechanisms of injury, closed physes, and high body mass index in adolescents have been shown to be associated with more adult injury patterns including scaphoid waist and proximal pole fractures . Treatment of acute fractures with appropriate immobilization resulted in a 90 % union rate in their retrospective analysis of 351 pediatric and adolescent scaphoid fractures. Interestingly, they found that the most common location for scaphoid fractures was the waist (71 %) followed by the distal pole (23 %) and the proximal pole (6 %). Chronic fractures, displaced fractures, and proximal pole fractures that were treated with cast immobilization alone more often resulted in nonunion. Increased time to union was seen in patients with older fractures, displaced fractures, proximal pole fractures, and fractures seen in the setting of osteonecrosis. Encouragingly, the union rate following surgical treatment of nonunions in their series was 96.5 %. Increased time to union was seen in association with open physes, use of bone graft, fracture displacement, proximal pole fracture, and the type of screw used for fixation at the time of surgery (Gholson et al. 2011).
Displaced fractures of the scaphoid in children require open reduction with internal fixation either with k-wires or a headless compression screw. Fortunately nonunion in the pediatric population is rare if appropriate treatment is carried out (D’Arienzo 2002). Nonunion is most commonly seen in scaphoid waist fractures in patients between the ages of 11 and 15 years. Many cases of nonunion can be attributed to delay in or failure to diagnose the fracture. In fact, acute scaphoid fractures in children and adolescents that are treated promptly with immobilization very rarely result in nonunion (0.8 %) (Fabre et al. 2001). Most of the reported cases of scaphoid nonunion occur at the waist (Wulff and Schmidt 1998; Fabre et al. 2001; Chloros et al. 2007).
In pediatric patients who present with a nonunion of the scaphoid and have never had treatment with immobilization, this is the recommended first course of action. One can consider the use of a bone stimulator to help with healing.
However, in pediatric scaphoid fracture patients who have not gone on to achieve union despite appropriate diagnosis and immobilization, surgical treatment is warranted. Fortunately, results of open reduction with internal fixation and bone grafting, usually nonvascularized, are uniformly good in this population with very good rates of healing and low complication rates (Mintzer and Waters 1999; Waters and Stewart 2002). There have been no reports of growth disturbance of the scaphoid with this treatment.
Injuries of the less commonly fractured carpal bones in the immature carpus will be discussed briefly. However, the discussion of the surgical treatment in detail will be limited to the scaphoid as this is the most commonly encountered fracture requiring surgical intervention in the pediatric population.
Capitate Fractures
The capitate is the second most commonly fractured bone in the immature carpus. Fractures of the capitate are extremely rare in isolation and are usually undisplaced in this setting. Most commonly these fractures are amenable to simple immobilization as treatment (Young 1986). Capitate fractures are more commonly seen in association with scaphoid fractures and likely represent an injury on the spectrum of a trans-scaphoid, trans-capitate perilunate-type injury. In these scenarios, displaced fractures of the capitate are treated with concomitant open treatment of the scaphoid with simple pinning of the capitate fracture. It is important to remember that the retrograde blood supply in the capitate makes displaced fractures of the capitate susceptible to avascular necrosis of the proximal pole, thus necessitating prompt treatment.
Lunate Fractures
Isolated lunate fractures are extremely rare in the pediatric population and only a few case reports exist. Most of the lunate injuries seen are similar to those seen in the adult population, including isolated lunate dislocations or perilunate dislocations with or without an associated distal radius fracture (Sharma et al. 2007). These injury patterns should be treated with urgent closed reduction and cast immobilization with appropriate treatment of concomitant injuries as indicated.
Trapezium and Trapezoid Fractures
Fractures of the trapezium and trapezoid are extremely rare in the pediatric population. The general mechanism of injury postulated remains a fall onto an outstretched extended wrist. Most are undisplaced and routine immobilization is the recommended treatment.
Hamate Fractures
Hamate fractures in the skeletally immature patient are also extremely rare. Direct trauma to the ulnar aspect of the hand and crush injuries can result in this fracture. The most commonly seen fractures are fractures involving the hook of the hamate and those associated with carpometacarpal fracture dislocations of the ring and small fingers. Hamate hook fractures should be treated with simple immobilization in the pediatric population, as they rarely go on to nonunion in these patients. Displaced and unstable carpometacarpal fracture dislocations should be treated with reduction and fixation (Goddard 2010).
Triquetrum Fractures
Fractures of the triquetrum are also very rarely seen in the pediatric population. The mechanism of injury is generally a hyperextension force to the wrist. These fractures occur most commonly between the ages of 11 and 13 years (Letts and Esser 1993). The majority of triquetrum fractures can be described as subtle avulsion-type or impingement-type fractures. Oblique radiographs may be required to diagnose them, and therefore, the diagnosis is often delayed or missed. Tenderness over the triquetral point located dorsally and just distal to the ulna should arouse the suspicion of this fracture to the examiner. These injuries can be associated with soft tissue injuries to the lunatotriquetral ligament or the triangular fibrocartilage complex. Cast immobilization for 3–4 weeks is recommended with uneventful healing generally expected (Letts and Esser 1993).
Pisiform Fractures
Pisiform fractures of the immature carpus are extremely rare. When seen in isolation, they are generally undisplaced and routine immobilization is recommended. Pisiform fractures can be seen along with other carpal bone fractures. There are a few case reports of pisiform dislocations, some in association with physeal fracture of the distal radius (Ashkan et al. 1998; Mancini et al. 2005). Dislocation of the pisiform can generally be treated with closed reduction followed by cast immobilization for 3–4 weeks and appropriate treatment of other associated injuries.
Surgical Procedure: Operative Treatment of the Acute Scaphoid Fracture
Preoperative Planning
Plain radiographs should be examined for fracture location, the presence of comminution and the presence of other associated injuries to the distal radius or other carpal bones. The location of the fracture may determine which surgical approach is used. Distal pole fractures are more easily approached from volarly, while proximal pole fractures are more easily stabilized from dorsally.
Evaluation of the size and skeletal maturity level of the patient to determine choice of implant (k-wires, absorbable pins, headless compression screw) should be performed using plain radiographs (Table 3).
Table 3
Operative Treatment of Acute Scaphoid Fractures – Preoperative Planning
Supine position |
Radiolucent hand table |
Mini or standard c-arm |
Nonsterile tourniquet |
Special equipment: drill, k-wires, headless compression screw of choice, all lengths and sizes available |
Positioning
The patient is placed supine with a radiolucent hand table attached on the operative side. All bony prominences should be well padded. The hand table should be centered using the patient’s shoulder as a guide. A mini c-arm or standard sized fluoroscopy unit should be used intraoperatively. A nonsterile pneumatic tourniquet is applied to the upper arm and the limb is exsanguinated prior to inflation.
Surgical Approaches
Dorsal Open Approach
Lister’s tubercle is palpated on the dorsal aspect of the distal radius. A transverse or longitudinal incision is made at the level of the radiocarpal joint just distal to Lister’s tubercle. Careful blunt dissection is used to expose the extensor tendons distal to the true extensor retinaculum specifically identifying the extensor tendons of the second, third, and fourth compartments. The interval between the third and fourth compartments is developed to expose the dorsal wrist capsule. A small release of the distal aspect of the extensor retinaculum over the third and fourth compartments will help facilitate exposure and not result in bowstringing of the tendons. Once the dorsal wrist capsule is exposed, a limited arthrotomy is performed. This can be oriented longitudinally, obliquely, or transversely. Care is taken to avoid injury to the scapholunate ligament during the arthrotomy as it often has attachments to the undersurface of the wrist capsule in this area. With flexion of the wrist, the proximal pole of the scaphoid and the scapholunate ligament are easily visualized and accessed.
Volar Open Approach
The two externally palpable landmarks of the distal pole of the scaphoid and the flexor carpi radialis (FCR) tendon are palpated on the volar radial surface of the distal portion of the wrist. A zigzag-type incision is used to cross the wrist flexion crease between these two landmarks and end proximally on the radial side of the FCR tendon. The distal pole of the scaphoid is easily palpable and identifiable in the distal aspect of the incision. Once the distal pole is identified, it is exposed sharply to isolate the entry point for fixation. Extreme extension of the thumb can aide in exposure of the distal pole and facilitate placement of fixation in the optimal center-center position of the scaphoid. A small portion of the proximal radial edge of the trapezium can be removed if needed to facilitate exposure to the distal pole of the scaphoid. The exposure can be extended proximally if visualization of the scaphoid waist is required by longitudinally incising a portion of the radioscaphocapitate ligament deep to the FCR tendon sheath. The incised ligament must be preserved for meticulous repair following fixation of the scaphoid fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


