Cardiology
Deepak Palakshappa
Paritosh Prasad
Ana Maria Rosales
EKG Interpretation
Approach to the EKG
Indication for EKG: W/u for chest pain, syncope, cyanotic episodes, drug ingestion, CHD eval, palpitations, pericarditis, Kawasaki dz, myocarditis, rheumatic heart fever, FHx sudden death and electrolyte abn. (Emerg Med Clin North Am 2006;24:195)
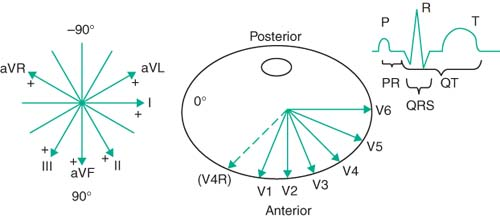
Basic EKG: 12 lead w/ 6 precordial leads and 3 limb leads (BMJ 2002;324:1382)
Paper speed usually 25 mm/sec so each small box 0.04 msec, 5 boxes 0.20 msec
Standard voltage is at 10 mm/mV; 1 mm = 0.1 mV; can be modified at request
Leads: R and L arm, R and L leg give rise to I, II, III, aVL, aVR, aVF.
Dipolar: I, II, III; represent differential from one lead to another
In I, positive deflection of wave is signal traveling toward RA to LA
In II, positive deflection of wave is signal traveling toward RA to LL
In III,– positive deflection of wave is signal traveling toward LA to LL
Unipolar: + deflect = center out to limb; aVR (RA), aVL (LA), aVF (LL)
Pericardial leads: Views cardiac activity in the horizontal plain.
 |
Initial EKG read: Always take a systematic approach; check speed and voltage
Rhythm: Regular or irregular; then if sinus (every P followed by QRS, constant PR)
Rate: # of large (5 mm) boxes btw R waves; 1 = 300 bpm, 2 = 150, 3 = 100; pattern is 300, 150, 100, 75, 60, 50; can also use 1500/# small boxes
Axis: If R + in limb lead, vector goes toward that lead; nml axis based on age
R waves + I and + aVF = 0°-90° (noted as normal axis; but can be abn for age)
R waves + I and – aVF = 0° to -90° (Left axis deviation) actually -30–90
R waves – I and + aVF = 90°-180° (Right axis deviation)
R waves – I and – aVF = neg 90° to -80° (Extreme right/NW deviation)
Neonates w/ transitioning from R sided dominance; initially w/ R axis as nml
P wave axis; if sinus then + I, +aVF, if not consider ectopic atrial pacer (EAP)
P waves: Should be same morphology in a given lead, otherwise multi pacemakers
2.5 mm wide in II and/or biphasic in V1 = p mitrale; left atrial enlargement
2.5 mm high in II = p pulmonale; right atrial enlargement
Q wave: Can be nml (II, III, aVF, V5, V6), max amp at 3–5 yr (0.6–0.8 mV nml)
QRS complex: R:S ratio initially >1 in V1 and V2, and <1 in V5 and V6, at about 3 yo R:S ratio becomes <1 in V1 and V2, and >1 in V5 and V6; some pts w/ juvenile pattern until 8–12 yr. (Heart 2005;91:1626)
EKG assessment of LVH very poor in pediatrics; sens 19.4%, spec 85%
T wave: Progressive changes through childhood, very different than adult pattern
1st 2–3 DOL upright T wave in V1–V3 normal, then inverts in 1st wk of life
T wave becomes upright during childhood, starting w/ V3, then V2, then V1
50% nml 3–5 yos have inverted T in V2, only 5%–10% nml 8–12 yo w/ inverted T.
T wave in V5 and V6 should be upright in all ages. (Heart 2005;91:1626)
Intervals: Interpretation varies based on age group. (Heart 2005;91:1626)
PR: ↑ w/ ↑ vagal tone, heart block, endocarditis w/ abscess, hyperK, digoxin tox, short w/ pre-excitation (WPW), EAP, glycogen storage dz
QRS: >0.08 msec if <8 yo or >0.10 msec if >8 yo = bundle branch block, junctional or ventricular rhythm (not via His Purkinje) (Emerg Med Clin North Am 2006;24:195)
QT: Start of Q to end of T; correct for HR w/ Bazett formula QT/[check mark]RR
Both old and recent reviews place upper limit nml QTc at 450 msec
Age Dependent Changes
(Emerg Med Clin North Am 2006;24:195)
Nml limits prev from Davignon et al. (2141 Caucasian pts), more recent by Rijnbeek et al. w/ higher sampling rate w/ sign. diff in nml limits (Euro Heart J 2001;22:702)
| HR | PR Interval | QRS Axis | QRS Interval | QTc Limit | |
|---|---|---|---|---|---|
| 0–1 wk | 90–160 | 0.08–0.15 | 60°–180° | 0.03–0.08 | <0.49 |
| 1wk–2 mo | 100–180 | 0.08–0.15 | 45°–160° | 0.03–0.08 | <0.49 |
| 2–6 mo | 105–185 | 0.08–0.15 | 0°–135° | 0.03–0.08 | <0.49 |
| 6 mo–1 yr | 110–170 | 0.07–0.16 | 0°–135° | 0.03–0.08 | <0.45 |
| 1–8 yr | 90–165 (1–2 yr) 65–140 (>2 yr) | 0.09–0.17 | 0°–110° | 0.04–0.08 | <0.45 |
| 8–16 yr | 60–130 | 0.09–0.17 | -15°–110° | 0.04–0.09 | <0.45 |
| >16 yr | 50–120 | 0.12–0.20 | -15°–110° | 0.05–0.10 | <0.45 |
Heart Murmurs
Definition
Result of turbulent blood flow; can be 2/2 ↑ blood flow (fever, anemia), abn cardiac structures (abn valve, cardiac defect) or combination
50%–70% seen annual exam, sports physicals, etc. w/ murmur on exam but only 0.8%–1% of pop w/ structural congenital heart disease. (Pediatr Rev 2007;28:e19)
Cardiac Examination
(Pediatr Rev 2007;28:e19)
Observation for syndromic appearance, central cyanosis, breathing, JVP
Palpation for thrills and point of max impulse for displacement, hyperdynamic flow
Pulse exam: Bounding (inc pulse pressure; PDA, AR, hyperthyroid, AVF), pulsus parvus (weak)/tardus (late) in AS, unequal in all 4 ext (aortic coarc)
Abdominal exam: Hepatosplenomegaly (CHF), pulsatile liver (TR)
Auscultation characterizing S1 (AV valves) and S2 (aortic and pulmonic often split)
S3 (rapid filling of ventric) often normal in children; sounds like slosh-ing-in
S4 (snap of stiff ventricle) always pathologic; sounds like a-thick-wall
Heart sound order; S4 — S1 —–S2—–S3; S2 nml split to A2–P2; can mistake for S3
——slosh-ing—in
a——thick- wall—–
Murmurs: Define timing (systolic vs. diastolic; early, mid, late), intensity, location, quality, configuration (crescendo, decrescendo, etc.), duration.
Systolic: Holosystolic (involves S1, cont to S2 at same intensity) and heard w/ AV valve regurg or VSDs; ejection murmurs (begin after S1 w/ cres-decresc) and related to flow in great vessels. (Pediatr Clin North Am 2004;51:1515)
Diastolic: Almost always pathologic (aside from venous hum);
Continuous: Flow through vessel/communication distal to aortic/pulm valves
Pathologic (PDA; continuous machinery murmur) or benign (venous hum)
Innocent Murmurs of Childhood
(Circulation 2005;111:e20; Pediatr Clin North Am 2004;51:1515)
Stills murmur: Most common innocent murmur in children; 1st described in 1909
Typically heard in patients aged 2–6 yo, but can be heard in infants and adolescents
Vibratory systolic murmur, low pitched, best at LLSB radiating to apex
2/2 turbulence in LV outflow tract; change w/ position and dec w/ Valsalva
Pulmonary flow murmur: Cres-decres, early to mid-peaking systolic at LUSB
Rough and dissonant, best heard in supine position; inc w/ expiration, dec upright
Can be difficult to distinguish from ASD murmur but w/ ASD have fixed split S2
Pulm stenosis distinguished by possible presence of thrill, ejection click, soft S2
Peripheral pulmonary artery stenosis: Common <1 yr age, usually gone by 6 mo
Low-/moderate-pitched ejection murmur in early/mid systole best at axilla or back
In utero pulm outflow tract well developed, pulm arterial branches comparatively underdeveloped and arise at sharp angles, which resolves w/ growth
May be difficult to distinguish btw this and pathologic periph pulm artery stenosis w/ Williams or rubella syndrome; murmur may persist beyond S2 w/ these.
Supraclavicular flow murmurs: Cres-descres harsh, high-pitched 2/2 nml bld flow in aorta and head/neck vessels; hear best above the clavicles (e.g., over carotids)
Same sitting or supine; diminished w/ shoulder girdle hyperextension (arms back)
Aortic systolic flow murmur: Systolic ejection in aortic area 2/2 increased cardiac output; anxiety, anemia, hyperthyroidism, fever, extreme fitness.
If murmur inc w/ dec preload (Valsalva, squat to stand) → HOCM
Venous Hum: Most common type of continuous murmur and benign
Best at infraclavicular region while sitting or standing; usually > on R side
Diminished w/ supine position or pressure over jugular vein
Pathologic Murmurs
(Circulation 2005;111:e20)
Systolic – usually longer and louder than innocent counterparts
Pansystolic: Involves/obscures S1; if constant; VSD, MR, TR; if crescendo, then PDA.
Ejection (AS, PS): Signs of pathology are presence of ejection click, abn S2 split
Assess pulses, presence of cardiac failure (JVD, etc.), diastolic murmur as well
Diastolic: W/ exception of venous hum, all diastolic murmurs are pathologic
Often need to reposition patient to best auscultate (sitting up leaning forward for aortic sounds and left lateral decubitus to best hear mitral sounds)
Early: Usually decres; assoc w/ aortic or pulmonic regurgitation
Mid: Cres-descres 2/2 inc flow across nml MV/TV or 2/2 MS/TS
Late: Cres and also assoc w/ mitral or tricuspid stenosis (MS/TS)
Continuous: Harsh machinelike murmur classic for PDA
Further Evaluation
(Circulation 2005;111:e20)
Depends on clinical assessment of patient; if asymptomatic, exam is usually sufficient
Echo is gold standard to assess cardiac structure; ancillary testing w/ EKG or CXR may be helpful; some suggest referral to pediatric cardiology before imaging.
Syncope
Definition
(Pediatr Rev 2000;21:384)
Sudden, often brief loss consciousness and postural tone 2/2 ↓ cerebral blood flow
Presyncope is the feeling one is about to pass out
Etiology
Breath-holding spells: Incidence of 4.6% and primarily occur between 1 and 5 yr
Always provoked by pain, anger, or frustration; normal physical and neuro exam
Cyanotic type (80%): Peaks at 2 yo and resolves by 5 yo
Characterized by a prodromal period of crying then forced expiration and apnea
Involuntary Valsalva → ↑ intrathoracic pressure → ↓ cardiac output → ↓ cerebral blood flow, LOC, and loss of muscle tone
May be assoc w/ generalized clonic jerks, opisthotonos, and brady
Pallid type (20%): Preceded by frustration, pain, sudden startle, or minor trauma
Initial quieting and breath holding → pallor → LOC and loss of muscle tone
Abnormal slowing of HR w/ ocular compression seen in >50%
Ocular compression test w/ at least 3 sec of asystole, followed by pallid syncope, and no epileptiform discharges on EEG confirms dx
Neurocardiogenic (vasovagal): Because of autonomic dysfunction; strong FHx
Usually seen in adolescents after prolonged standing in a crowded, warm environment
Characteristically preceded by nausea, diaphoresis, light-headedness, or yawning
Cardiac syncope
Arrhythmogenic: Prolonged QT, WPW, heart block, sick sinus syndrome, SVT
Structural: HOCM, severe aortic/pulmonic stenosis, pHTN, anom L coronary
POTS (postural orthostatic tachycardia syndrome)
Myxomas
Neuropsychiatric
Seizures/drop attacks
Hyperventilation syndrome/panic attacks
Hypoglycemia: gradual onset w/ weakness, hunger, sweating, agitation, confusion
Migraines assoc w/ vertebrobasilar vascular spasm: HA persists after awakening
Benign paroxysmal vertigo: sudden falling attacks w/ dizziness in pts <6 yo
Cough syncope: Most common in children w/ asthma
Recovery w/i seconds, and consciousness restored w/i minutes
Clinical Manifestations
Hx most important in selecting dx studies and guiding Rx
Should include the time of day, time of last meal, and details of preceding activities
Syncope at rest/recumbent suggests sz or arrhythmias
Syncope w/ exercise suggests HOCM
Syncope while standing suggests vasovagal
Syncope w/o warning suggests primary cardiac
Medication Hx including prescribed, OTC, and illicit drugs
FHx: Sudden unexplained death, deafness, arrhythmias, congenital heart disease, sz, metabolic diseases, or MI at young age
Physical Exam
Cardiac exam: Pulse, BP, orthostatics, murmurs, clicks; detailed neuro exam
Diagnostic Studies:
Guided by History and Physical Exam
Measurement of serum glucose and electrolytes rarely of value unless an acute episode
EKG: Assess rhythm, conduction, premature beats, delta waves, chamber enlargement, PR, QRS, and QTc; further testing w/ exercise tests or 24-hr Holter if needed
Toxicology screen
Echocardiography w/ Doppler studies
Tilt table testing for positional syncope
EEG: In pt w/ prolonged LOC, suspected sz; postictal, drowsiness or confusion
Cardiology c/s indicated for pathologic heart murmur, CP preceding syncope, arrhythmia, ↑QTc, Q waves, RV strain (suggestive of pHTN), or LVH on EKG, or w/ FHx of cardiomyopathy or sudden death
Treatment
Breath-holding spells: Reassurance and explanation of pathophysiology most important
Iron therapy has been shown to decrease incidence in cyanotic type
Consider anticholinergics in pallid type if they become severe or frequent
Neurocardiogenic: Consider PO salt suppl +/- fludrocortisone over a few weeks
Cardiac: Include drug therapy, radiofrequency ablation, or pacemaker placement
Pts w/ long QT should not receive macrolides or cisapride
Seizures: Appropriate anticonvulsants
Chest Pain
Definition
(Pediatr Clin North Am 2004;51:1553)
Chest pain (CP) in the pediatric population is overwhelmingly benign, but can have significant impact on patients; ½ miss school, 69% self-limit activity.
Source can be 2/2 musculoskeletal, respiratory, cardiac, GI, or nervous system.
Incidence of chest pain 2/2 cardiac etiology <5%.
Epidemiology
(Pediatr Rev 1986;8:56)
Primary complaint in 0.3%–0.6% of pediatric patients in ED or outpt care
May be chronic lasting up to 6 mo in 15%–36% of patients, 1 yr in 8%
Mean age of presentation is 12–14 yr.
Clinical Manifestations
Detailed Hx: Describe\pain (location and duration) quality, radiation, severity, temporal assoc (w/ breathing, eating, activity), exacerb or alleviating factors
In younger patients, assess for occult history of ingestion as well.
Chest pain assoc w/ exertion, syncope, light-headedness, or palpitations is concerning.
Family Hx of sudden death, HOCM, MVP, or personal Hx of Kawasaki concerning
Etiologies
(Pediatr Rev 1986;8:56; Pediatr Clin North Am 2004;51:1553)
Cardiac: Rare; responsible for <5% of pediatric chest pain
Mitral valve prolapse: 18% pts w/ MVP have chest pain, though pain not 2/2 valve prolapse, unclear if neuroendocrine or autonomic dysfunction
Check flat, sitting, and standing for midsystolic click and late systolic murmur
Association with anxiety exists; echo is gold standard to diagnose
Pericarditis: Sharp and stabbing, often pleuritic and positional; improved w/ leaning forward; may have recent URI sx’s, fever. Viral cause most common
Can be infectious, inflammatory (w/ CTDs), neoplastic, or 2/2 XRT
Exam w/ pericardial rub; EKG w/ PR depressions and diffuse ST elevations across all leads. PR elevation in aVR most specific finding.
Myocarditis can also p/w chest pain but usually 2/2 assoc pericarditis
Coronary vasospasm: P/w crushing, diffuse chest pain w/ assoc SOB, diaphoresis, radiation to L arm, neck, or jaw; light-headedness/syncope.
Exam may have gallop (S3 and S4), +/- signs of poor cardiac function
Consider cocaine induced, check tox screen, and if suspected use combined α- and β-antagonist (pure β-antagonist → unopposed α activity and periph vasospasm)
Can also see vaso-occlusive dz w/ some systemic dz’s; ex sickle cell
Anomalous coronary artery: Rare; coronary arteries arise from opposite sinus of Valsalva increases risk for ischemia and sudden death
Usually p/w sudden death but 5/27 in 1 study w/ CP in prior 2 yr
Chest pain associated w/ exertion; often nml physical exam; usually silent or S3 and/or S4 (cardiac dysfunction)
EKG and stress test have not shown to be helpful in identifying at-risk pts
Kawasaki disease: If c/b coronary artery aneurysm, can see stenosis or aneurismal thrombus; if Hx prior Kawasaki w/ aneurysm and p/w CP, ischemia until proven not.
LV outflow obstruction: Hypertrophic obstructive cardiomyopathy (HOCM) most common though rarely p/w chest pain; exam w/ systolic murmur at aortic region that amplifies w/ standing or Valsalva
Pulm HTN: Unclear mech; may be 2/2 pulm art stretch or RV ischemia. (Am Fam Physician 2001;63:1789)
Tachyarrhythmias: Abrupt onset and cessation, w/ or w/o activity, often w/ N/V.
Exam usually normal; EKG may demonstrate delta wave if pre-excitation (Wolf-Parkinson-White w/ bypass tract).
Idiopathic: 21% cases no cause identified in prospective study (Pediatrics 1988;82:319)
Avg pt w/ wks to mos intermittent CP, sharp, w/ or w/o exertion, short duration, no assoc sx, recurrence common, PE nml, and pain not reproducible
Musculoskeletal: 15% cases in prospective study (Pediatrics 1988;82:319)
Strain or costochondritis from overuse or trauma. Reproducible on exam.
Hx of exertion/activity, pain usually sharp and radiating, can be pleuritic
Costochondritis w/ tenderness on palpation of site of rib attachment to sternum
Precordial catch syndrome – sharp, well localized twinge of pain, acute onset at rest and lasts sec to min; not reproducible on palpation
Slipping rib syndrome: 8th,9th,10th ribs slip over one another (Pediatrics 1985;76:810)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


