Brief History of Female Pelvic Reconstructive Surgery
Peter L. Dwyer
Bob L. Shull
S. L. Stanton
Introduction
Over the 20th century, advances in medicine have improved the quality and length of people’s lives everywhere. This ballooning of medical knowledge has occurred through diligent research into the causation of disease with a better understanding of pathophysiology and careful and better assessment, leading to accurate diagnosis and appropriate treatment. There has been increasing specialization in medicine with the development of divisions initially into medicine and surgery, then specialist, Colleges of Obstetrics and Gynaecology and subspeciality interest groups such as urogynecology. It is appropriate that the first chapter in this book is devoted to the development of urogynecology as a subspecialty—what were the important contributions that led to advancing our knowledge in the assessment and treatment of disorders of the pelvic floor and lower urinary tract in the female. Our increasing knowledge was not solely by gynecologists but also from scientists, other specialist areas such as urologists and colorectal surgeons, physiotherapists, and nursing colleagues for there should be no barriers to knowledge, just as there are no borders within the pelvis to effective treatment of pelvic floor disorders.
We discuss the people and the events that moved the specialty of urogynecology forward, although this road has not always been smooth and without controversy. The advancement of medical knowledge occurred through the diligence of inquisitive people asking simple questions such as why is that so, or how can I do this better? Chance also played a part, as when Florey found the penicillin mold growing on the petri dish on the windowsill or Sims using the knee-chest position to distend the vagina with air and examine the vesicovaginal fistula with his speculum or Kelly dropping and breaking the glass partition of his primitive cystoscope seeing the inside of the air-filled bladder for the first time. The accumulation of knowledge is slow and is based on improvements in many areas, including technology such as Edison electric light in endoscopy, so his quote “if I see further it is because I sit on the shoulders of giants” is so true.
The evolution of our understanding of urogynecologic conditions and their treatment with improved outcomes has occurred slowly and, at times, erratically. Rather than look at a timeline of milestones and people, we explore the key areas in urogynecology and discuss what events and people in our opinion made a real difference.
The areas to be explored are the following:
Urinary stress incontinence
Endoscopy with cystourethroscopy and laparoscopy and their contribution to the assessment and management of pelvic floor disorders
Painful bladder conditions
Lower urinary tract and anorectal fistulas
Uterovaginal prolapse
STRESS URINARY INCONTINENCE
Anterior Colporrhaphy with Bladder Neck Buttress
The anterior colporrhaphy was being performed in the 1870s. Leon Le Fort, a French surgeon, describes his procedure for partial colpocleisis for prolapse in 1877, and Archibald Donald (1908) and Fothergill (1915), both English surgeons, describe the Manchester repair with vaginal repair, cervical amputation, and reattachment of the uterosacral ligaments. Kelly1 published his classic description in 1913, describing “the torn or relaxed tissues of the vesical neck should be sutured together using two or three vertical mattress sutures of fine silk linen passed from side to side” (Fig. 1.1). Victor Bonney in 1923 stated that “incontinence depends in some way upon a sudden and abnormal displacement of the urethra and urethrovesical junction immediately behind the symphysis.” Aldridge et al.2 in 1952 thought that lack of support of the bladder base and neck and proximal urethra, and prolapse of the urethrovesical junction outside the environment of the intra-abdominal pressure, was associated with incontinence. The vaginal repair was a simple, low-risk vaginal
operation which became the primary surgery used by gynecologists to treat urinary stress incontinence for a century until thinking started to change in the 1970s with the introduction of the Burch colposuspension.
operation which became the primary surgery used by gynecologists to treat urinary stress incontinence for a century until thinking started to change in the 1970s with the introduction of the Burch colposuspension.
The first reported elective hysterectomy was performed by Conrad Langenbeck in 1813 and was through a vaginal approach. Interestingly, after 200 years, despite the vaginal approach having the lowest morbidity and cost, it remains less popular today than the alternatives of abdominal, laparoscopic, and robotic hysterectomy. Trends in medicine are not always driven solely by science.
Urethral Suspensions
The first retropubic operation for the treatment of stress urinary incontinence (SUI), the Marshall-Marchetti-Krantz procedure, was said to be described in a 1949 paper entitled “The Correction of Stress Incontinence by Simple Vesicourethral Suspension.”3 Marshall, a urologist, believed that elevation of the junction to its normal position restores continence. He developed an operation for treating voiding dysfunction that developed after rectal resection in men as a result of pronounced urethral hypermobility. He, with two gynecologists, Marchetti and Krantz, employed a suprapubic approach to suspend the bladder neck by placement of interrupted chromic catgut sutures to the periosteum of the symphysis and posterior rectus sheath for the treatment of SUI in women. However, 30 years earlier in 1920, Thomas Hepburn, a urologist from Hartford, Connecticut, described a retropubic urethral suspension for females with urethral prolapse. Initially performed in children, he reported a further two cases in adult women. “When the neck of the bladder has been freed enough, so that traction on the bladder reduces the prolapse, it is sutured with 20 day catgut” to the periosteum.4 There is no record of him using this operation to treat women with stress incontinence. Hepburn had a large family of six children, including a son who became a urologist and a daughter, Katharine, who became a Hollywood actress.
John Christopher Burch, a professor at Vanderbilt, described his retropubic colposuspension technique in 19615 after noting that when performing a Marshall-Marchetti-Krantz procedure, the sutures in the periosteum of the pubic symphysis often pulled out, and there was the added risk of osteitis pubis.
Robert Zacharin described in 19636 the anatomical supports of the urethra and their importance in the continence mechanism and prevention of urinary stress incontinence. Based on his findings, he developed his
own urethral suspension operation for SUI. Eventually, it was these ideas that lead to the placement of the midurethral slings (MUS) at the midurethral rather than the bladder neck. The midurethral placement of slings without tension decreased the incidence of postoperative voiding difficulty without adversely affecting the continence success rate.
own urethral suspension operation for SUI. Eventually, it was these ideas that lead to the placement of the midurethral slings (MUS) at the midurethral rather than the bladder neck. The midurethral placement of slings without tension decreased the incidence of postoperative voiding difficulty without adversely affecting the continence success rate.
In 1959, Pereyra,7 an American gynecologist, performed the first needle endoscopic bladder neck suspensions, and subsequently, modifications were made by Raz, Stamey, and Gittes. Although initially popular, particularly with urologists in the 1970s and 1980s as it was a simple procedure with low morbidity, the continence outcomes were not as good as the retropubic procedures. Peattie and Stanton8 reported a cure rate in women over 65 years as only 41% at 3 months.
Sling procedures
Allographic slings
The first suburethral sling procedure was described in 1907 by von Giordano who suggested the use of the gracilis muscle by wrapping it around the urethra. In 1910, Goebel9 described detaching the pyramidalis muscle and suturing it beneath the urethra, and Frangenheim10 modified the technique in 1914 by attaching a vertical strip of rectus fascia to the pyramidalis muscle. Price11 described the first sling constructed from fascia lata in 1933, and Aldridge12 in 1942 described a rectus fascia sling with two strips of rectus fascia sutured in the midline below the urethra via a separate vaginal incision. Other autographic material, including fascia lata and round ligament (Hodgkinson), have been used. The Aldridge sling has two bilateral fascial strips, which are left attached medially to the rectus sheath, passed behind the symphysis pubis, and sutured together beneath the bladder neck. These slings were used mainly for recurrent severe SUI by gynecologists. A simple modification named the pubovaginal sling, using a strip of detached rectus fascia fashioned as a free graft through a Pfannenstiel incision and passed under the urethra with a vaginal incision, was popularized by urologists McGuire and Blaivas in the 1970s and 1980s to treat women with severe or recurrent incontinence and/or intrinsic sphincter deficiency.13 Although very successful, fascial slings were associated with an increased rate of voiding dysfunction and morbidity when compared to urethral suspension operations. In the 1990s, the incidence of voiding dysfunction decreased with the MUS placement under minimal tension.
Synthetic slings
The use of synthetic slings was introduced in the 1960s with the Moir’s gauze hammock operation14 and the Morgan sling15 using Mersilene and polypropylene mesh, which they placed under the bladder neck through an abdominal and vaginal incision. Stanton et al.16 used a silastic sling in the 1980s again, which was introduced through abdominal and vaginal incisions. Although all had good results in small trials, they were not widely used. In the 1970s and 1980s, the Burch colposuspension was popularized by Hilton and Stanton17 and performed globally in over 80% of SUI operations with fascial slings less than 10%.18
Midurethral sling procedures
In the 1990s, urinary stress incontinence surgery was revolutionized by the advent of minimally invasive MUS procedures. The tension-free vaginal tape (TVT) was developed by Petros and Ulmsten.19 Petros first met Ulf Ulmsten at a conference in Melbourne in 1989 organized by one of the chapter’s authors. Based on Zacharin’s anatomical studies, Petros was experimenting in animals attempting to recreate pubourethral ligaments initially by the temporary placement of Mersilene tapes placed at the insertion of pubourethral ligaments at the midurethra. This led to a collaboration with Ulmsten and the development of the TVT, a loosely woven suburethral polypropylene sling attached to trocars passed through vaginal and abdominal stab incisions and performed under local anesthesia as same day surgery.20 This proved to be as safe and effective procedure as the Burch colposuspension but required less dissection and had less postoperative complications, pain, and hospital stay. There was a rapid uptake of MUS from 1998 and a corresponding decline in colposuspensions.18 MUS are currently the most commonly performed operations for SUI.
In view of the success of the MUS, it is not surprising there have been further modifications.
The transobturator sling was developed in 2001 by Delorme21 using the obturator foramina approach to place the midurethral tape, and DeLeval22 described an inside-out approach in 2003. These two transobturator approaches could reduce potential injury to the bladder, bowel, and other major vessels compared to the retropubic approach but have a higher incidence of postoperative pain. The third generation of slings was the single-incision mini-slings, also placed at the midurethra, and attached to the obturator fascia and muscle without exit incisions. Potentially, this may cause less postoperative pain, but the longer term effectiveness remains to be proven.
Urethral Injections with Bulking Agents
The first reported use of urethral injections was by Murless in 1938 using sodium morrhuate.
In 1974, Politano injected polytetrafluoroethylene or Teflon first to treat postprostatectomy incontinence in men and then used it in women with urinary stress
incontinence in the early 1980s. This was followed by periurethral and transurethral of bovine dermal collagen. In the 1990s, silicone microparticles and cross-linked polysaccharides and hyaluronic acid in the 2000s. More recently, in the 2010s, autologous fat, skeletal cells, and stem cells have all been studied but not used widely.
incontinence in the early 1980s. This was followed by periurethral and transurethral of bovine dermal collagen. In the 1990s, silicone microparticles and cross-linked polysaccharides and hyaluronic acid in the 2000s. More recently, in the 2010s, autologous fat, skeletal cells, and stem cells have all been studied but not used widely.
The urethral injections can also be performed under local anesthesia as day surgery and have low morbidity which makes them particularly suited to the elderly. With the adverse media attention of synthetic products, there has been a considerable increase in their usage. However, continence success is low on follow-up and the injections frequently need repeating.
ENDOSCOPY
Cystourethroscopy
In 1804, Bozzini, a German physician, investigated possible options to examining “deeply seated organs” including the bladder and urethra. He advocated the inspection of all “interior cavities” by looking through natural openings or at least small wounds.23 He designed a number of long thin funnels, which he called a “lichtleiter” (light conductor), with illumination provided by a light reflected from a box containing a wax candle (Fig. 1.2). He presented his instrument to the Faculty of Medicine of Vienna, but they were reportedly alarmed at his invention. They ridiculed Bozzini’s lichtleiter, which effectively stopped any further development for many decades, and there is no evidence that it was used in a human. However, his ideas lived on, and he foresaw the future of diagnostic and operative endoscopy of the urinary tract (cystourethroscopy) and abdominal cavity (laparoscopy) and vaginal surgery (natural opening). He wrote, “Surgery will not only develop new and previously impossible procedures, but all uncertain operations which rely on luck and approximation will become safe under the influence of direct vision, since the surgeon’s hands will now be guided by his eyes.”
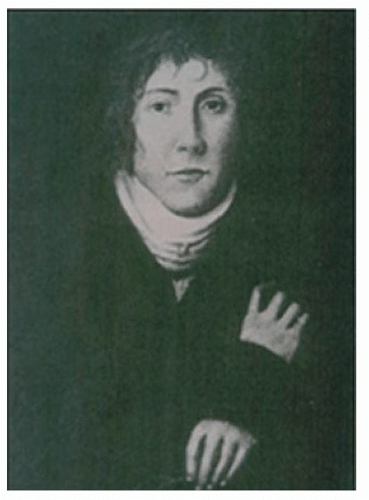 FIGURE 1.2 Philippe Bozzini, a German physician, circa 1804. (Reprinted from Alkatout I, Mechler U, Mettler L, et al. The development of laparoscopy—A historical overview. Front Surg 2021;8:799442.) |
In 1826, Pierre Ségalas had more success using a simplified version of Bozzini’s instrument. It was a funnel with a polished interior to reflect light. It was used to illuminate the bladder and ureteral orifices with illumination from candles and a concave mirror which focused the light which allowed 3 mm of aperture for viewing and heralded the advent of cystoscopy for the diagnosis and treatment of lower urinary tract conditions.24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



