Bowing Bones
Christopher G. Anton, MD
DIFFERENTIAL DIAGNOSIS
Common
Physiologic Bowing
Blount Disease
Less Common
Rickets
Fibrous Dysplasia
Neurofibromatosis
Osteogenesis Imperfecta
Rare but Important
Congenital Tibial Dysplasia
Congenital Bowing
Achondroplasia
Camptomelic Dysplasia
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Must determine which causes of lower extremity bowing are physiologic vs. pathologic
Isolated or generalized bowing
Cortical thickening along convex side and thinning along concave side of curve
Neonates and infants have normal varus angulation of lower extremities
Correction of bowing by 6 months after beginning to walk or aged 1.5-2 years old
Hint: Considered abnormal if varus angulation of knee in child > 2 years old
Changes to valgus angulation by 1.5-3 years old (11° in 3 year old)
5-6° of valgus angulation by 13 years old
Helpful Clues for Common Diagnoses
Physiologic Bowing
a.k.a. developmental bowing
Exaggerated varus angulation when younger than 2 years old
If exaggerated during 2nd year of life, probably normal but follow to exclude development of Blount disease
More common in early walkers, heavier children, and African-American children
Tibial metaphysis appears prominent, depressed with small beaks of distal medial and posterior tibia and femur
Not fragmented, thickened medial tibial cortex
Tilted distal tibial growth plate laterally
Usually resolves without treatment
Blount Disease
Infantile type: 1-3 years old, bilateral in 60-80%
Must differentiate from physiologic bowing
Adolescent type: 8-14 years old, more commonly unilateral
Thought to result from abnormal stress on proximal medial tibial physis
May reflect normal physiologic bowing that progresses and fails to predictably correct
Diagnosed by progressive clinical bowing on clinical examination in combination with characteristic radiographic changes
Predisposed: Early walkers, obese children, and African-Americans
Medial tibial metaphysis depression and fragmentation, constriction ± bone bridging of proximal medial tibial physis, genu varum
Enlarged epiphyseal cartilage and medial meniscus on MR
Metaphyseal-diaphyseal angle
Angle between line drawn parallel to proximal tibial metaphysis and another line drawn perpendicular to long axis of tibial diaphysis
Abnormal if > 11° on standing radiographs
Indeterminate angle (8-11°), should follow clinically ± radiographically
Helpful Clues for Less Common Diagnoses
Rickets
Generalized bowing, changes at sites of rapid growth
Deficiency in mineralization of normal osteoid, widening zone of provisional calcification
Metaphyseal flaring and fraying
Fibrous Dysplasia
Hamartomatous lesion, replacement of portions of medullary cavity with fibroosseous tissue
Long bone medullary space widening, endosteal scalloping, coarse or obliterated trabeculation
Lytic, ground-glass, or sclerotic
70% monostotic
90% of polyostotic lesions are unilateral
Sarcomatous degeneration: 0.5%
Neurofibromatosis
Anterolateral bowing of tibia, ± hypoplastic fibula, often narrowing or intramedullary sclerosis or cystic change at apex of angulation
Hamartomatous fibrous tissue
Bowing typically at junction of middle and distal 1/3 of tibia
May develop pathologic fracture, pseudoarthrosis of tibia ± fibula, tapering or penciling ends of bones at fracture site
Osteogenesis Imperfecta
History of osteogenesis imperfecta
Bowing results from soft bones
Generalized bowing of long bones, osteoporosis, and multiple fractures
Helpful Clues for Rare Diagnoses
Congenital Tibial Dysplasia
a.k.a. congenital pseudoarthrosis
Rare
70% will eventually be diagnosed with neurofibromatosis (NF)
1-2% of neurofibromatosis patients
Anterolateral tibia bowing or fracture
If fibular bowing is absent, tends to resolve spontaneously
Congenital Bowing
Abnormal intrauterine or fetal positioning
Convex posteromedially, rarely laterally
Calcaneovalgus deformity of ipsilateral foot
± diaphyseal broadening
Tends to resolve
± protective bracing
Achondroplasia
Generalized bowing
Most common form of short-limb dwarfism
Autosomal dominant or spontaneous mutation
Small thorax with short ribs
Short and thick long bones with metaphyseal cupping and flaring, short broad phalanges
Short rectangular iliac bones (elephant ear-shaped), narrow sacrosciatic notches, flat acetabular roof
Bullet-shaped vertebral bodies with posterior scalloping, narrowed interpedicular distances in lumbar spine
Camptomelic Dysplasia
a.k.a. campomelic dysplasia
Autosomal dominant
Often fatal in infancy
Anterolateral bowing of lower extremities > upper extremities
Bowed femur with short-bowed tibia
Pretibial skin dimples
Large skull with small face, hypoplastic scapula, narrow pelvis, dislocated hips, bell-shaped chest
Image Gallery
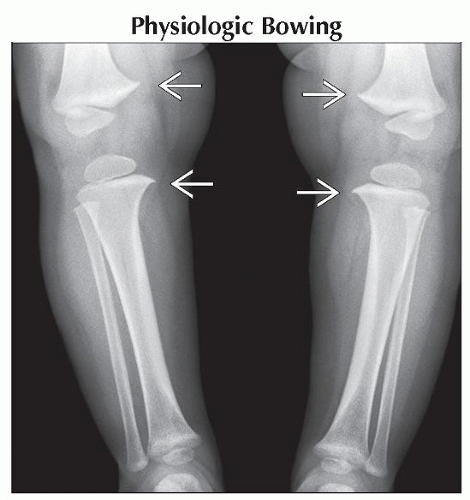 Anteroposterior radiograph shows the typical medial beaking of the bilateral tibia and femur
 and cortical thickening along the convex margin of the tibia. and cortical thickening along the convex margin of the tibia.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|