Perinatal Mortality Rate
In developed countries the perinatal mortality rate has been declining since the 1930s: in the UK it has declined from >50.0 to 7.5 per 1000 births in 2008 (data are collected separately in Scotland) (Fig. 34.1). The stillbirth rate was 5.1 per 1000 births. The lowest rates are found in Scandinavian countries and the highest in Bangladesh and Central Africa.
Risk Factors for Perinatal Mortality
Perinatal mortality is a reflection of obstetric care to only a limited extent and its decline has been more to do with better general health and nutrition, smaller families and improved neonatal care. The perinatal mortality rate is higher among lower socioeconomic groups, in those below 17 or above 40 years of age, in women who smoke, are obese, abuse drugs or have medical illnesses or poor nutrition. It is higher in highly parous women, in those of Asian or Afro-Caribbean extraction (approx twofold) and in those with multiple pregnancies.
Causes of Perinatal Mortality
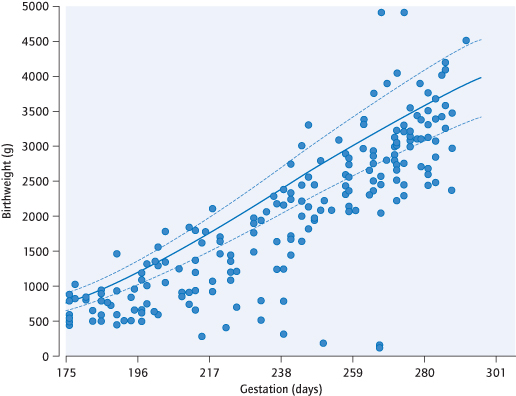
Causes of death are classified by the Extended Wigglesworth and supplemented by the Obstetric Aberdeen classification system, with a new (2010) classification of IUGR defined as <10th centile of birthweight in comparison to what would be expected from constitutional factors such as fetal gender [→ p.216] (Fig. 34.2). Many causes overlap: for instance, antepartum haemorrhage is associated with chronic compromise, pre-eclampsia, preterm labour and intrapartum hypoxia. Perinatal mortality for the UK was last systematically reported in 2010, for the year 2008. Because of separate reporting for still birth and neonatal mortality, of overlapping causes and of detailed classification, the list below is a simplification of the results.
Unknown: This represents approx 20% of perinatal mortality. New data suggest that mothers sleeping not in the left lateral (i.e. allowing aortocaval compression, Fig. 29.2) may be contributory (BMJ 2011: 342: 3403).
Preterm delivery is the most common cause of neonatal mortality.
Intrauterine growth restriction (IUGR): Using current (above) criteria this accounts for >10% of stillbirths, but a further 10% had placental lesions associated with chronic compromise and IUGR.
Antepartum haemorrhage occurs in at least 10% of deaths.
Intrapartum still birth accounts for 9% of still births, but >60% are preterm. Term intrapartum still birth is most commonly attributed to hypoxia, but infection and inflammation, trauma and fetal exsanguination can occur.
Major congenital abnormalities accounts for 10% of still births and about 25% of neonatal mortality. Rates vary between regions and are dependent on detection rates and cultural attitudes to termination.
Pre-eclampsia contributes in multiple ways, including preterm delivery and IUGR, but also at term.
Infection contributes to mortality most via preterm birth, but infection may also occur in term labour. Fetal infections in pregnancy (see Chapter 19) are a rare cause of mortality.
Fig. 34.2 Birthweight of previously unclassified stillbirths after adjustment for constitutional factors.
Principal Causes of Perinatal Mortality
| Unexplained antepartum stillbirth |
| Intrauterine growth restriction (IUGR) |
| Prematurity |
| Congenital anomalies |
| Intrapartum hypoxia |
| Antepartum haemorrhage |
Maternal Mortality
Definitions
A maternal death is the death of a woman during pregnancy, or within 42 days of its cessation, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
A late maternal death is when a woman dies from similar causes but more than 42 days and less than a year after cessation of the pregnancy.
These are subdivided into ‘direct’ deaths, which result from obstetric complications of the pregnancy, and ‘indirect deaths’, which result from previous or new disease, which was not the result of pregnancy but nevertheless aggravated by it.
Recent new classifications are ‘coincidental maternal deaths’, such as accidents or incidental death, which would have happened irrespective of the pregnancy, and ‘pregnancy-related death, including all ‘maternal deaths’ plus coincidental deaths, and therefore irrespective of the cause of death.
Maternal Death Rate
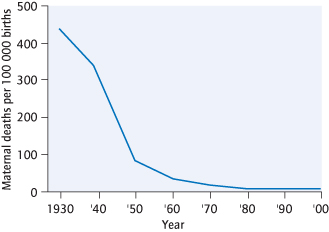
In the UK, the maternal death rate (direct and indirect, 2006–2008) was 11.4 per 100 000 pregnancies (CMACE 2011) (Fig. 34.3). The rate in developed countries has fallen dramatically since the 1930s, when it was similar to that found at present in developing countries; in recent years this decline has slowed. Deaths in less developed countries are far higher: rates of about 500 per 100 000 pregnancies are found in parts of Africa.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree