Bilateral Large Kidneys
Sara M. O’Hara, MD, FAAP
DIFFERENTIAL DIAGNOSIS
Common
Hydronephrosis
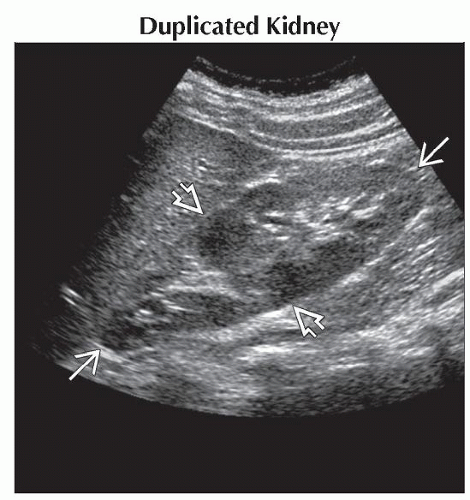
Duplicated Kidney
Pyelonephritis
Glomerulonephritis
Nephrotic Syndrome
Polycystic Kidney Disease
Autosomal Recessive
Autosomal Dominant
Lymphoma/Leukemia
Less Common
Lymphoproliferative Disorder
Sickle Cell Disease
Renal Vein Thrombosis
Hemolytic Uremic Syndrome
Henoch-Schönlein Purpura
Rare but Important
Nephroblastomatosis
Prune Belly Syndrome
Angiomyolipomas
Tuberous Sclerosis
Glycogen Storage Disease
Megacalycosis
Caroli Polycystic Kidney Disease
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Bilaterally enlarged kidneys often abnormal in morphology
Hydronephrotic
Cystic
Mass lesions
Altered cortex or medulla
Duplicated kidney
Exceptions where kidneys may appear large but otherwise “normal”
Pyelonephritis
Glomerulonephritis
Nephrotic syndrome
Refer to pediatric renal size charts to determine if kidneys are large
Rule of thumb for renal length range
Newborn: 3.5-5 cm
7-year-old child: 7-10 cm
Teenager: 10-12 cm
Helpful Clues for Common Diagnoses
Hydronephrosis
Look for site of obstruction
Duplicated Kidney
Look for band of cortex separating upper and lower pole
Look for 2nd renal pelvis and ureter
Pyelonephritis
May have normal echotexture on US
Look for
Altered corticomedullary interface
Focal hypoechoic area
Decreased perfusion on Doppler exam
Bulge in cortex from focal swelling
Striated nephrogram on CT, MR, or IVP
Poorly enhancing areas on contrast studies
Wedge-shaped photopenic area on DMSA scan
Glomerulonephritis
Kidneys are enlarged in acute phase
Kidneys may atrophy over time if insult continues and develop into ESRD
Nephrotic Syndrome
Classically enlarged with poor corticomedullary differentiation
Ascites and anasarca may be clue to diagnosis
Polycystic Kidney Disease
Autosomal Recessive
˜ 10% of all polycystic kidney diseases
More common cause of bilateral large kidneys in pediatric patients than autosomal dominant
Mutation of PKHD1 gene
Problems begin in utero
Many patients die within hours or days of birth
Some patients may live for years with chronic renal insufficiency
Imaging: Huge echogenic kidneys, tiny cysts, and dilated tubules visible with newer ultrasound machines
Autosomal Dominant
˜ 90% of polycystic kidney diseases
Variable penetrance and severity
Cysts replace functional nephrons and impair renal function
Cysts usually visible in 2nd and 3rd decade but can also be seen in infants and children
Lymphoma/Leukemia
Nonenhancing or hypoechoic rounded masses
Occasionally enlarged kidneys without discernible masses
Helpful Clues for Less Common Diagnoses
Lymphoproliferative Disorder
Transplant history or altered immune status
Nonenhancing or hypoechoic rounded masses
Associated adenopathy often impressive
Sickle Cell Disease
Renal medullary hyperechogenicity
RBCs sludging in vasa rectae
Papillary necrosis and hematuria
Renal Vein Thrombosis
Bilateral cases often involve thrombus of inferior vena cava
Kidneys enlarge acutely → infarct and atrophy
Hemolytic Uremic Syndrome
Disease of infants and children
Triad: Hemolytic anemia, thrombocytopenia, acute renal failure
Often follows GI, respiratory, or other febrile illness
Survival > 85% with early dialysis and supportive therapy
Henoch-Schönlein Purpura
Vasculitis often follows respiratory illness
Purpuric rash, arthralgias, fever, glomerulonephritis, bowel wall thickening
Helpful Clues for Rare Diagnoses
Nephroblastomatosis
Persistence of fetal metanephric blastema after 34 weeks gestation
Associated with
Beckwith-Wiedemann syndrome
Hemihypertrophy
Sporadic aniridia
Seen in 1% of infant autopsies
Increased risk of Wilms tumor
Prune Belly Syndrome
Kidneys are enlarged due to marked hydroureteronephrosis
Patulous collecting system without obstruction
Triad: Undescended testes, absent abdominal wall musculature, dilated urinary tract
Angiomyolipomas
Highly vascular tumors most often seen in tuberous sclerosis
Tuberous Sclerosis
Variable severity of renal cysts and angiomyolipomas
Glycogen Storage Disease
Metabolic products deposited in liver and kidneys cause enlargement
Megacalycosis
Nonobstructive caliectasis
Caroli Polycystic Kidney Disease
End of spectrum of autosomal recessive kidney disease with biliary ductal ectasia and hepatic fibrosis
Image Gallery
 Longitudinal ultrasound in the same girl shows a 13.6 cm left kidney (calipers), which is also duplicated. Note the mild prominence of the lower pole collecting system
 . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|