Chapter 36 Benign tumours, cysts and malformations of the genital tract
MALFORMATIONS OF THE GENITAL TRACT
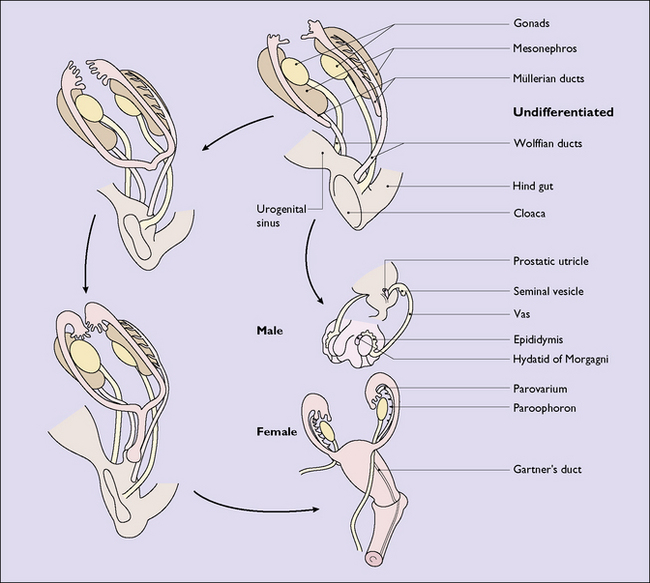
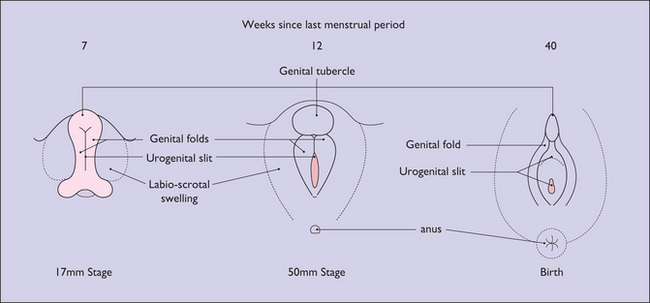
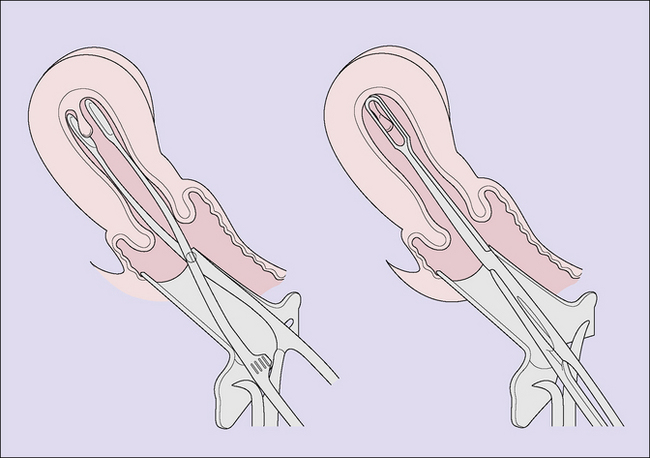
In a female fetus the Müllerian ducts develop from the paramesonephric ducts, growing caudally on each side. By the 35th day after fertilization the lower part of the ducts change direction and grow towards the midline, where they meet and fuse with each other and then grow caudally once again. By the 65th day they have completed the fusion and their medial walls have gradually disappeared to form a single hollow tube (Fig. 36.1). The most caudal portion, which will become the vagina, becomes solid and fuses with an ingrowth of endodermal cells from the cloaca. By the 20th gestational week, the solid growth has recanalized and the external genitalia have formed (Fig. 36.2).
Failure of recanalization
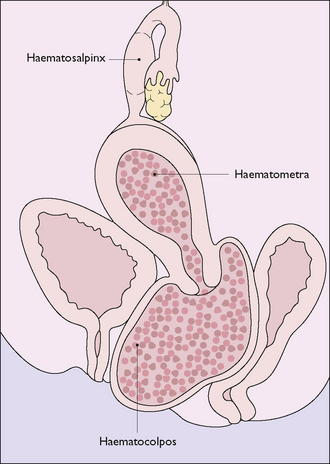
The most common defect is an imperforate hymen or transverse septum, which should be detectable during the examination of the neonate. If it is not detected until after puberty, menstrual discharge may collect in the vagina and, in long-term cases, may distend the uterus and tubes (Fig. 36.3). Treatment is to make a cruciate incision in the hymen septum and permit the inspissated fluid to escape slowly. Less common defects produce complete or partial vaginal atresia.
Failure of the ducts to form or to fuse
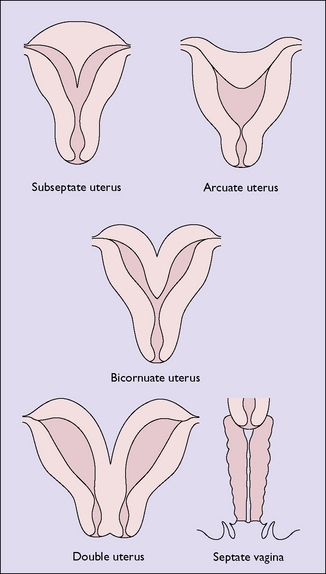
Failure of the two Müllerian ducts to fuse leads to one of several malformations (Fig. 36.4). Most of these malformations do not reduce the woman’s fertility, but should pregnancy occur there is an increased risk of late miscarriage and premature labour. A subseptate uterus may lead to recurrent abortion, and can be treated by excising the septum by surgery or laser. If the woman has a bicornuate uterus and becomes pregnant, the fetus may present as a transverse lie in late pregnancy.
UTERINE TUMOURS
Endometrial polyps
Endometrial polyps may occur in association with endometrial hyperplasia and may be a cause of abnormal uterine bleeding. They are detected by curettage, provided a polyp forceps is also introduced into the uterus (Fig. 36.5), or by hysteroscopy.
Uterine fibroids (leiomyomata, fibromyomas)
These are the most common tumours of the genital tract. A uterine fibroid is composed of smooth muscle bundles interspersed with strands of connective tissue, surrounded by a thin capsule (Box 36.1). The tumour may arise in any part of the Müllerian duct, but occurs most often in the myometrium, where several may develop simultaneously. The tumour may vary from the size of a pea to that of a football.
Box 36.1 Fibroids
| What are they? | Encapsulated smooth muscle fibres interspersed with strands of connective tissue usually developing in the myometrium. They may remain intramural or grow outwards or into the uterine cavity. Dependent on an intact blood supply |
| Aetiology | Unclear |
| Prevalence | Increases from 5% to 20% of women during their reproductive years. More common in nulliparous women and those of low parity. Very slow growing in response to oestrogen. Regress after menopause |
| Diagnosis | Examination and confirmatory ultrasound |
| Symptoms | Depend on size and position and are frequently symptomless. Two most common symptoms are abnormal vaginal bleeding, usually heavy and/or prolonged, and pelvic discomfort, crampy or pressure |
| Management | Depends on rate of growth, size, symptoms and desire for pregnancy • Myomectomy to preserve fertility, possibly in conjunction with a GnRh analogue to shrink the tumour temporarily |
| Outcome | Hysterectomy is the treatment of choice for women comfortable with its psychological and physical sequelae Myomectomy is associated with a 40% chance of successful conception and a 5% recurrence of the fibroid or menorrhagia |
| Pregnancy complications | Early pregnancy bleeding, premature rupture of membranes, obstructed labour and postpartum haemorrhage |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree