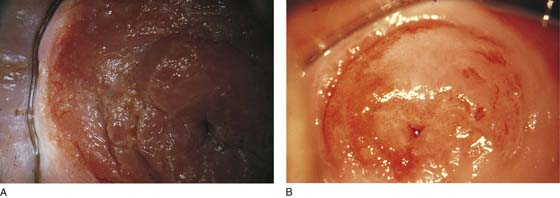
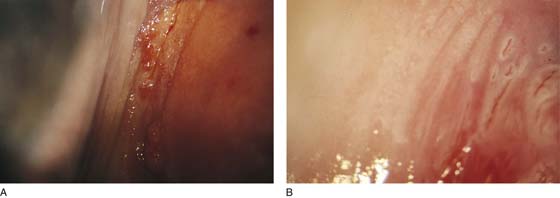
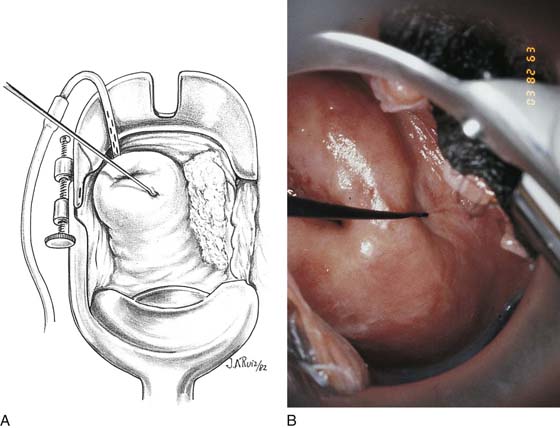
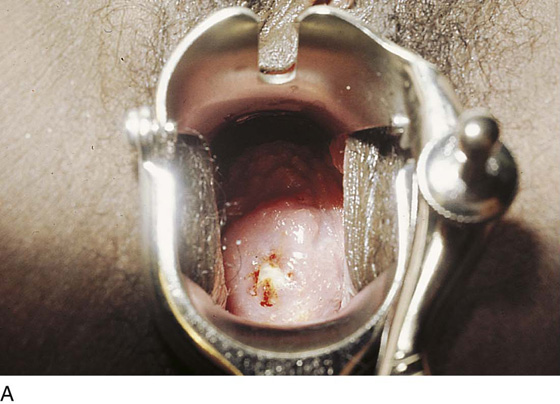
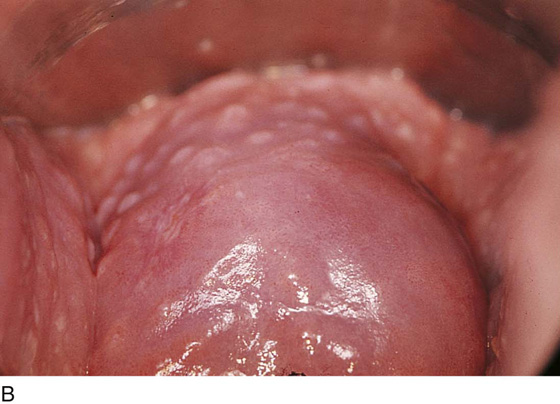
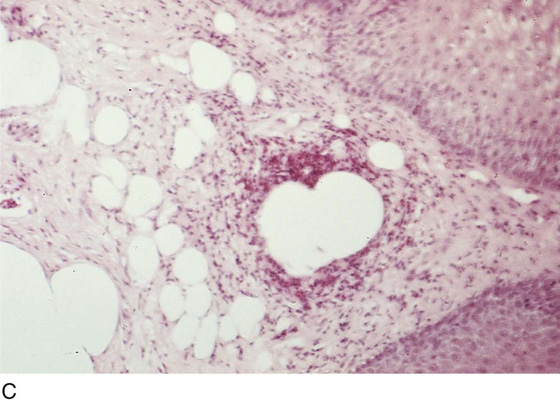
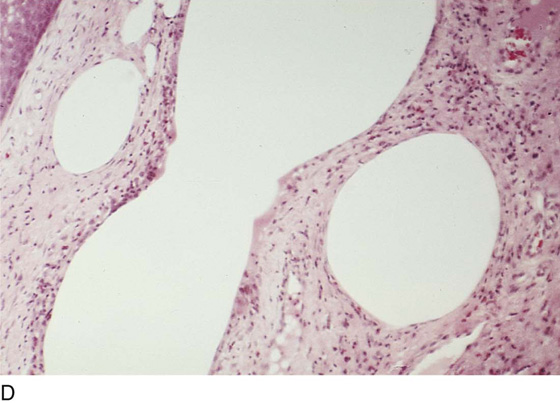
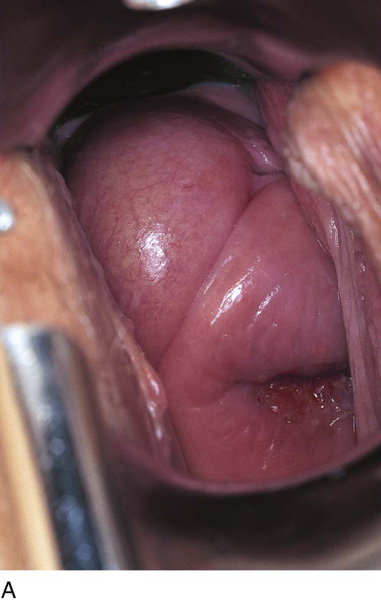
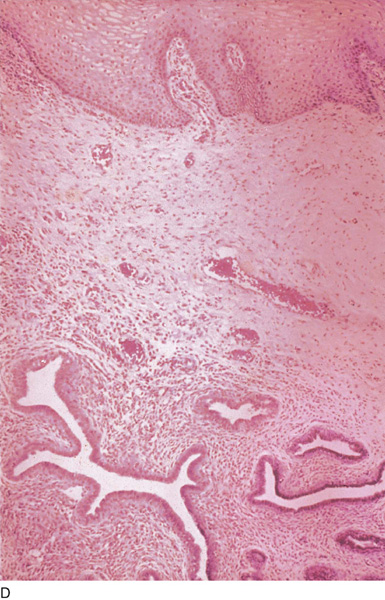
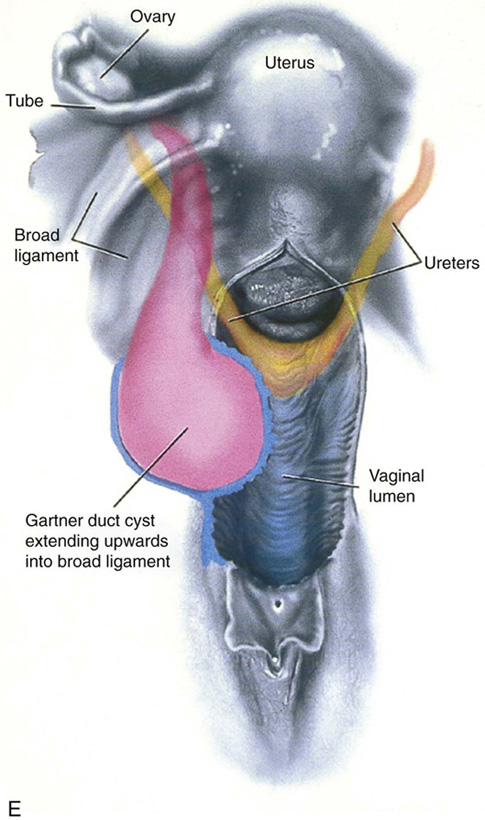
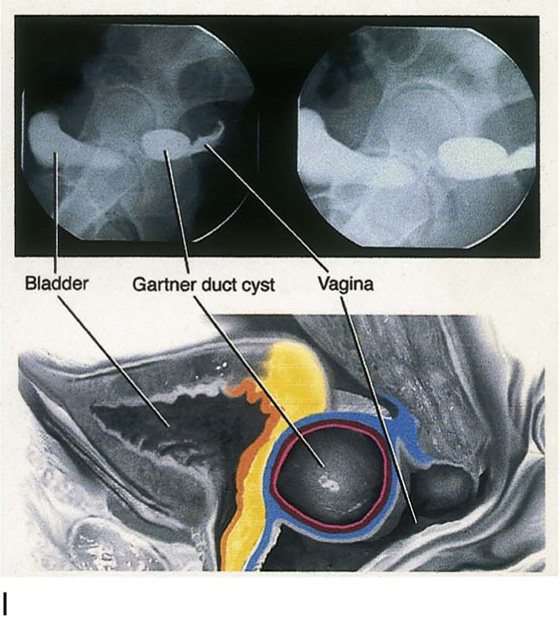
CHAPTER 60 Under normal circumstances, the vagina does not contain any glands. However, when the condition of adenosis exists (i.e., occurs spontaneously or as the result of antenatal diethylstilbestrol [DES] exposure), mucosal and submucosal mucus-secreting glands may be identified (Fig. 60–1A, B). These lesions appear as granulation-like tissue, clefts, holes, or cysts (Fig. 60–2A, B). Whenever adenosis is suspected, the lesion should be biopsied to ensure that adenocarcinoma does not exist within or around it. Additionally, the risk of squamous intraepithelial neoplasia is increased because of the multiple squamocolumnar junctions exposed to environmental factors associated with coitus. Vaginal biopsies are performed in a manner similar to that used for cervical disease (i.e., with a long-shanked biopsy forceps) (Fig. 60–3). Exposure can be a problem for vaginal lesions, and the use of a manipulating hook allows the examiner to properly display the lesion to colposcopic vision (Fig. 60–4A, B). Cysts 2 cm or larger should be excised in the operating room with the patient under local or general anesthesia. Clearly, these lesions may run the gamut from mucous inclusions (adenosis), to squamous inclusions, to Gartner duct cysts (mesonephric remnants). Viewing a cyst from the vagina provides little insight as to its origin or potential risk(s). An unusual condition that produces small cysts—some up to 1 to 1.5 cm—is vaginitis emphysematosa. This condition is associated with multiple gas-filled spaces (Fig. 60–5A through D). The Gartner duct (mesonephric) is found deep in the lateral wall of the vagina; although it may wander anteriorly or posteriorly, a cyst duct may extend cranially through the entire length of the vagina and via the cervix into the broad ligament (Fig. 60–6A through E). Before embarking on an operation to remove the cyst, it is important for the gynecologist to obtain as much preoperative information about the cyst and its neighboring structures as possible (Fig. 60–6F through H). The technique of excising any vaginal cyst is similar. The relationship of the cyst to the bladder and the ureter must be known (Fig. 60–6I). If necessary, the ureter should be catheterized. FIGURE 60–1 A. The cervix and the vagina of this diethylstilbestrol (DES)-exposed woman reveal total absence of a squamous epithelial covering of the ectocervix. The vaginal fornices likewise contain only glandular tissue. B. Another DES-exposed woman’s cervix and vagina show extensive squamous metaplasia (pink) interspersed with glandular tissue (red). FIGURE 60–2 A. Granulation-like glandular tissue located in the lateral vaginal fornix is diagnostic of adenosis. B. Clefts and gland openings are apparent in this patient’s vagina. A biopsy into this area will reveal mucous glands beneath the surface squamous metaplastic epithelium. FIGURE 60–3 A directed vaginal biopsy is performed under colposcopic guidance. Patients feel little, if any, discomfort if the biopsy is performed in a timely manner with a sharp biopsy clamp. FIGURE 60–4 A. To expose the vaginal fornices to facilitate a directed biopsy, a long-handled titanium hook pulls the cervix out of the way. B. Without the benefit of the hook, it would be exceedingly difficult to obtain an adequate colposcopic view of the lateral fornices. FIGURE 60–5 A. Numerous small cysts are seen in the anterior vaginal fornix. These cysts are filled with gas. B. A magnified view of part A reveals the appearance of vaginitis emphysematosa. C. Microscopic section through the vaginal wall (part A) showing air spaces beneath the epithelial pegs. D. Vaginitis emphysematosa is characterized by gas-filled spaces surrounded by multinucleated giant cells. FIGURE 60–6 A. A large Gartner duct cyst is seen in the right anterolateral wall of the vagina. The cervix is displaced downward and to the left. Preoperatively, the cyst should be injected with radiopaque dye and fluoroscopically studied. An intravenous pyelogram and cystoscopy should be performed to determine the exact location of the bladder and ureter relative to the cyst. Ureteral catheterization is recommended if the cyst will be excised. B. A large cotton swab displaces the cervix posteriorly to better delineate the relationship of the Gartner duct cyst to the urinary bladder. C. Microscopic section through mesonephric duct remnant in the lateral wall of a normal vagina. Obstruction of this duct leads to a Gartner duct cyst. D. Above is the stratified squamous epithelium of the vagina. The glandular structures lying (below) in the vaginal stroma (wall) are remnants of the mesonephric duct and tubules. E. Gartner duct cysts may become quite large, as is illustrated in part A
Benign Lesions of the Vaginal Wall
Biopsies
Cysts
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree