8 Benign Changes Fibroadenomas are mixed fibroepithelial tumors. Depending on the endotumoral distribution of the stromal and epithelial components, they are classified as intracanalicular and pericanalicular fibroadenomas. This differentiation is of no clinical importance. In younger women, fibroadenomas typically show a high proportion of epithelial tissue (myxoid fibroadenomas). With increasing age, and especially in postmenopausal women, the fibrotic component of these tumors increases and predominates. In this phase, progressive hyalinization and calcification takes place (fibrotic fibroadenomas).
Fibroadenoma
 If there is any doubt concerning histology, a percutaneous biopsy is indicated to verify a fibroadenoma. This is preferably performed under ultrasound guidance.
If there is any doubt concerning histology, a percutaneous biopsy is indicated to verify a fibroadenoma. This is preferably performed under ultrasound guidance.
Fibroadenoma: General information | |
Incidence: | The most common benign breast tumor (~10% of all women). |
Age peak: | All ages. Peak between 20 and 50 years. |
Risk of malignant transformation: | No increased risk. |
Multifocality: | 10%–15%. |
Findings | |
Clinical: | Small fibroadenomas are clinically occult. Larger tumors are well-circumscribed, movable, painless nodules. |
Mammography: | Small fibroadenomas and ones that are within dense parenchymal areas are often mammographically occult. Larger tumors appear well-circumscribed, homogeneously dense, oval or lobulated (typically no more than 3 lobuli). Occasional halo sign. Fibrotic fibroadenomas may display endotumoral dumbbell-shaped and/or popcorn macrocalcifications. Note: In the beginning stages of calcification, fibroadenoma-associated calcifications may appear as suspicious clustered, pleomorphic microcalcifications. |
Ultrasonography: | Small fibroadenomas within lipomatous breast tissue may be sonographically occult. Larger tumors appear smooth-bordered, oval or lobulated, with homogeneous internal echotexture. The longitudinal axis is parallel to the skin. The surrounding architecture is undisturbed. Depending upon their water content, they display a moderate to strong posterior acoustic enhancement and possibly a lateral posterior acoustic shadowing. Fibrotic fibroadenomas with endotumoral calcifications may display acoustic extinction posterior to macrocalcifications. Lesion compressibility is slight to good, depending upon histological composition. |
Myxoid fibroadenomas are the most common benign solid tumors in young women. With increasing age, the water content of these tumors decreases, and the fibrotic component increases. | |
 MR Mammography: Fibroadenoma
MR Mammography: Fibroadenoma
T1-Weighted Sequence (Precontrast)
Small fibroadenomas located within the parenchyma are not usually visible in the precontrast examination. Larger tumors are oval or lobulated lesions with well-circumscribed borders (Fig. 8.2b). Myxoid fibroadenomas have a higher water content than the surrounding parenchyma and are therefore usually hypointense (Fig. 8.1c). With progressing fibrosis, however, they gradually become isointense (Figs. 8.5c, 8.6b). Fibroadenomas located within fatty tissue are more easily detected (Figs. 8.7c, 8.8c). Dystrophic macrocalcifications cause endotumoral signal extinction. In rare cases, a lipomatous peripheral border may be present (MR equivalent of halo sign) (Fig. 8.3c).
T2-Weighted Sequence
The signal intensity of a fibroadenoma in the water-sensitive T2w series is also dependent upon its histological composition.
Myxoid fibroadenomas. Myxoid and predominantly myxoid fibroadenomas are tumors with a high internal water content. Because of this, they typically have a high signal intensity in the T2w images (Figs. 8.1b, d, 8.3b, d), sometimes making the differentiation from a cyst difficult (Fig. 8.5b). The previously described internal septations are sometimes more easily seen in the T2w images than in the subtraction images (Fig. 8.2c).
Fibrotic (hyalinized) fibroadenomas. Fibrotic fibroadenomas are tumors with a low internal water content that usually have intermediate (Fig. 8.6c) or absent signal (Fig. 8.8b,d) in the T2w images. Partially fibrotic fibroadenomas only show a higher signal intensity in the less fibrotic areas within the tumor (Fig. 8.7b,d).
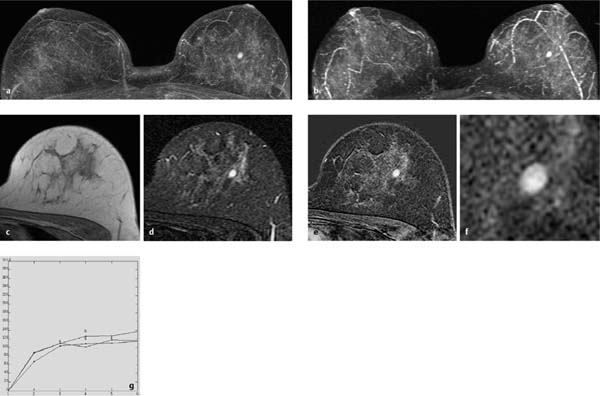
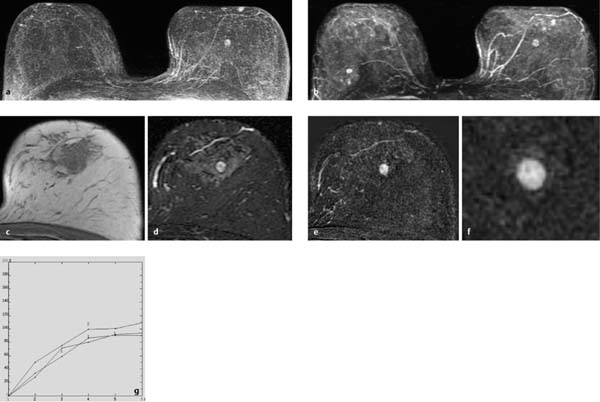
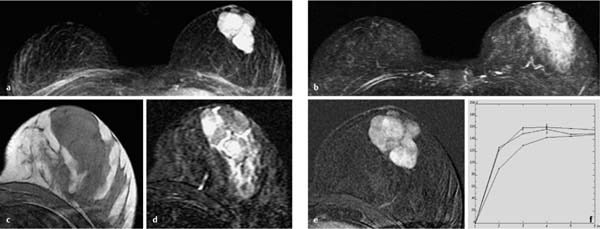
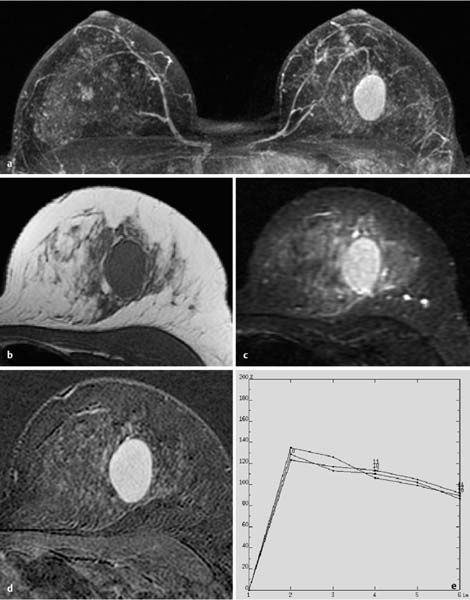
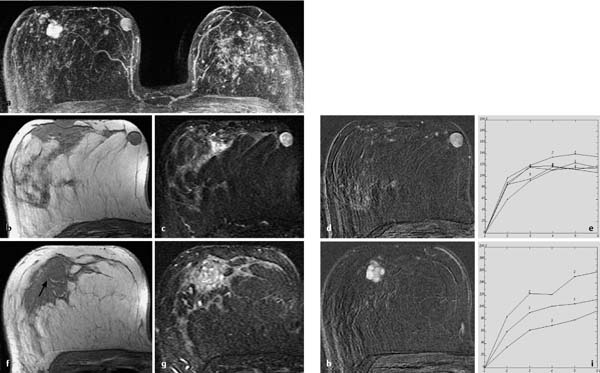
Fig. 8.1a–g Myxoid fibroadenoma.
a Subtraction MIP: solitary oval, well-circumscribed mass lesion in the left breast.
b T2w MIP: high signal intensity (water content).
c T1w precontrast slice image: well-circumscribed, oval, hypointense lesion.
d IR T2w slice image: high water content.
e Early subtraction slice image: homogeneous hypervascularization.
f Zoomed subtraction image.
g Time–signal intensity curve (TIC): moderate initial enhancement (just under 100%) and postinitial plateau.
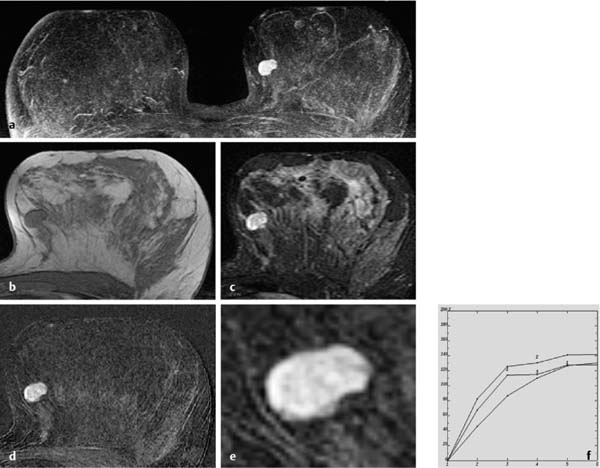
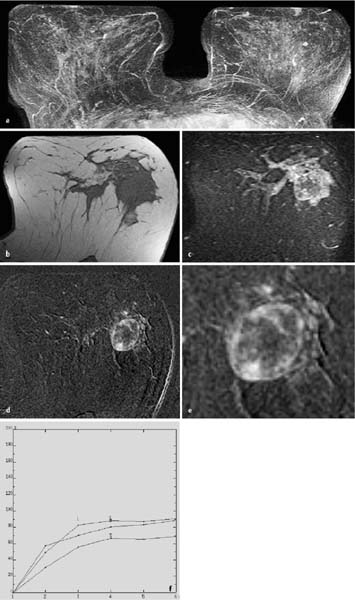
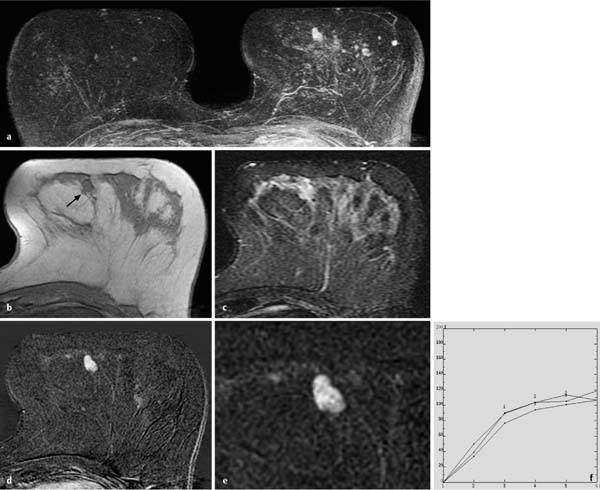
Fig. 8.2a–f Myxoid fibroadenoma with internal septations.
a Subtraction MIP: solitary lobulated, well-circumscribed mass lesion in the left breast.
b T1w precontrast slice image: well-circumscribed, lobulated, homogeneously hypointense lesion.
c IR T2w slice image: high signal intensity (water content). Depiction of several internal septations with lower signal intensity.
d Early subtraction slice image: inhomogeneous hypervascularization. Dark internal septations with lower vascularization.
e Zoomed subtraction image.
f TIC: rapid initial enhancement (max. 120%) and persistent postinitial enhancement.
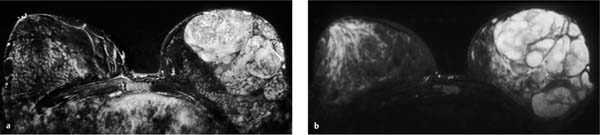
Fig. 8.3a–g Bilateral myxoid fibroadenomas. Left fibroadenoma displays a halo sign.
a Subtraction MIP: solitary lobulated (3 lobuli), well-circumscribed mass lesion in the left breast. Solitary oval, well-circumscribed mass lesion in the right breast.
b T2w MIP: high signal intensity (water content) of both lesions.
c T1w precontrast slice image (left): well-circumscribed, lobulated, homogeneously hypointense lesion with peritumoral border of fat-equivalent signal intensity (halo sign).
d IR T2w slice image: high signal intensity (water content). Depiction of multiple internal septations with lower signal intensity.
e Early subtraction slice image: inhomogeneous hypervascularization. Dark internal septations without vascularization.
f Zoomed subtraction image.
g TIC: rapid initial enhancement (max. 180%) and postinitial plateau.
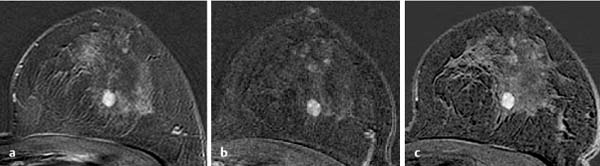
Fig. 8.4a–c Myxoid fibroadenoma. Unchanged in follow-up over several years.
a Subtraction slice image: sound, well-circumscribed mass lesion with strong hypervascularization and dark internal septations.
b Breast MRI 1 year later shows unchanged lesion characteristics.
c Breast MRI 2 years later continues to show unchanged lesion characteristics.
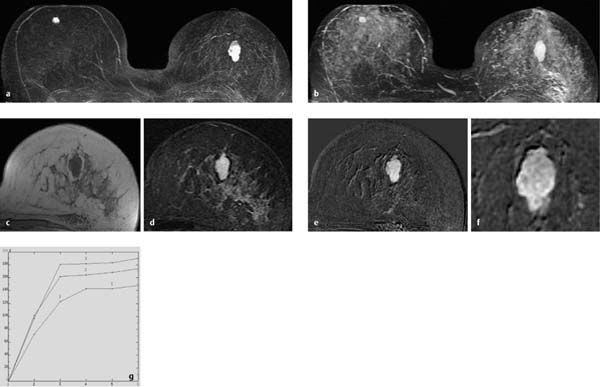
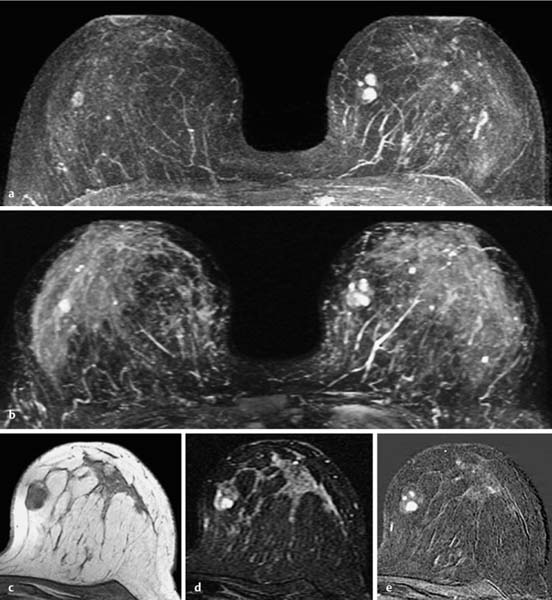
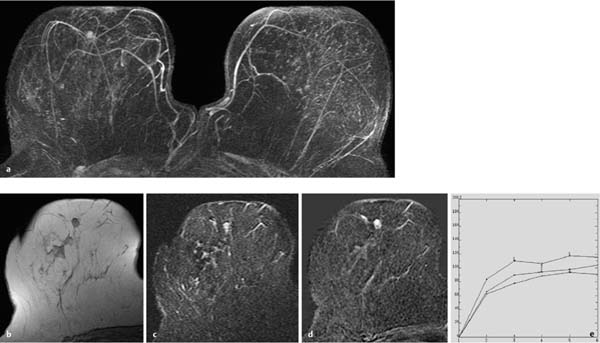
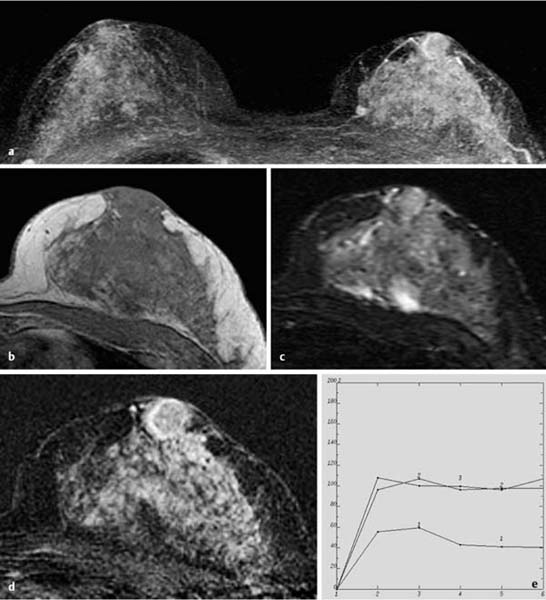
Fig. 8.5a–g Partially fibrotic fibroadenoma.
a Subtraction MIP: solitary round, well-circumscribed mass lesion in the left breast.
b T2w MIP: inhomogeneous high signal intensity (water content). Depiction of a few small cysts in both breasts.
c T1w precontrast slice image: well-circumscribed, partially hypointense, partially isointense (compared to surrounding parenchyma) lesion with halo sign.
d IR T2w slice image: partially high, partially low signal intensity.
e Early subtraction slice image: inhomogeneous hypervascularization.
f Zoomed subtraction image.
g TIC: moderate initial enhancement (max. 50%–80%) and persistent postinitial enhancement.
T1-Weighted Sequence (Contrast Enhanced)
The signal behavior of a fibroadenoma after contrast administration is dependent upon the histological composition of the tumor.
Myxoid fibroadenomas These are tumors with a high proportion of epithelial tissue, more frequent in younger women. Myxoid fibroadenomas are oval (Fig. 8.1a, e, f) or lobulated (Fig. 8.2a) lesions with well-circumscribed borders. The tumor matrix displays a rapid and strong enhancement. Dark internal septations often pass through the matrix and represent less vascularized fibrotic strands (Figs. 8.2 d, e, 8.3a, e, f). Myxoid fibroadenomas typically have a strong CM uptake. The initial enhancement phase rarely shows a slow or medium (Fig. 8.1g), often a rapid (Fig. 8.2f), and occasionally a very rapid enhancement (up to several hundred percent), sometimes with values higher than those found in malignant tumors (Fig. 8.3g). The postinitial signal phase usually displays a continuous increase (Fig. 8.2f) or plateau (Fig. 8.1g). A postinitial signal washout is extremely rare (< 1% in our data collection). The transition from a myxoid to a fibrotic fibroadenoma usually takes many years (Figs. 8.4, 8.5a, e, f).
Fibrotic (hyalinized) fibroadenomas. These are tumors with a high proportion of fibrotic tissue, more frequent in older women. Fibrotic fibroadenomas are oval or lobulated lesions with wellcircumscribed borders. Depending on the degree of fibrosis, there is little CM uptake (partially fibrotic fibroadenoma) (Figs. 8.6a, d, e, 8.7a, e) or no CM uptake (completely fibrotic fibroadenoma) (Fig. 8.8a,d). Only the less fibrous portion of a partially fibrotic fibroadenoma will show hypervascularization. The classic fine internal septations seen in myxoid fibroadenomas are only rarely present. Instead there are wide areas of extensive sclerosis. If there is any enhancement at all, initial enhancement will be slow to moderate, and postinitial enhancement is persistent or shows a plateau (Figs. 8.5 g, 8.6f).
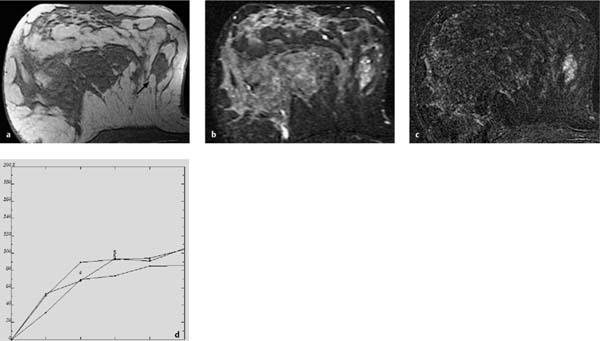
Fig. 8.6a–f Partially fibrotic fibroadenoma.
a Subtraction MIP: unremarkable findings in large breasts with strong parenchymal enhancement.
b T1w precontrast slice image: vague mass lesion with isointense signal in comparison with surrounding parenchyma.
c IR T2w slice image: indistinct mass lesion with higher signal intensity in peripheral tumor areas.
d Early subtraction slice image: well-circumscribed, oval mass lesion with peripheral hypervascularization and central areas without hypervascularization.
e. Zoomed subtraction image.
f TIC: moderate initial enhancement (max. 50%–80%) and persistent postinitial enhancement.
Special Types of Fibroadenomas
Juvenile fibroadenomas and giant fibroadenomas are variants that occur in addition to the common adult type of fibroadenoma. Apart from their greater size, they have the same image characteristics as the typical myxoid fibroadenoma. Despite the fact that they are benign lesions without an elevated risk of malignant transformation, they are usually excised because of their large size.
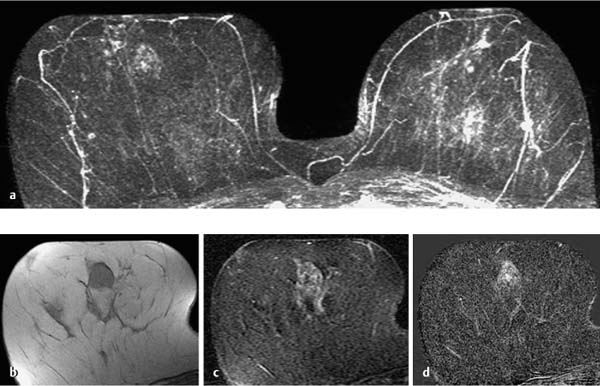
Fig. 8.7a–e Special case: Partially fibrotic fibroadenoma.
a Subtraction MIP: conglomerate of several foci and well-circumscribed mass lesions in the medial aspect of the left breast.
b T2w MIP: foci and masses display high signal intensity (water content).
c T1w precontrast slice image: the described conglomerate is localized within a larger lobulated, well-circumscribed lesion.
d IR T2w slice image: partially high, partially low signal intensity within larger lesion.
e Early subtraction slice image: homogeneous hypervascularization of areas with high water content.
Assessment: BI-RADS 2 lesion. The differential diagnosis includes a hamartoma and a fibroadenoma. Histology revealed a partially fibrotic fibroadenoma.
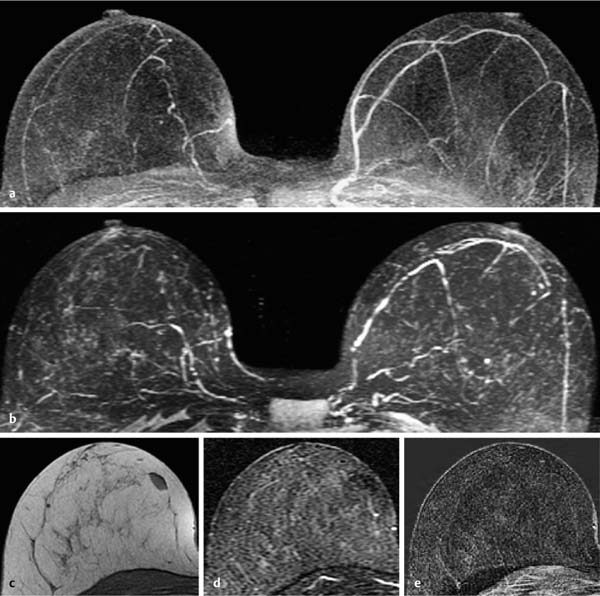
Fig. 8.8a–e Fibrotic fibroadenoma.
a Subtraction MIP: unremarkable findings.
b T2w MIP: unremarkable findings.
c T1w precontrast slice image: well-circumscribed, oval lesion easily identified within the fat tissue of the right breast.
d IR T2w slice image: no increased signal in the water-sensitive image.
e Early subtraction slice image: no enhancement.
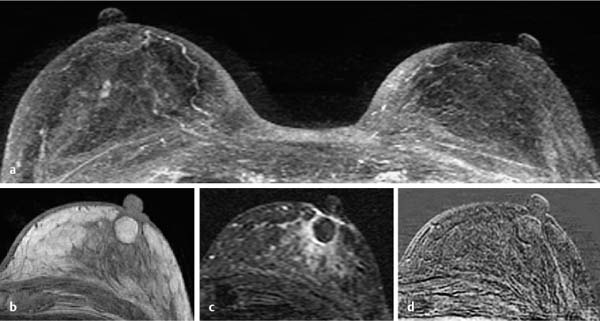
a Subtraction MIP: conglomerate of several lobulated, well-circumscribed, hypervascularized mass lesions in the left breast.
b T2w MIP: high signal intensity (water content) of all lesions and surrounding parenchyma.
c T1w precontrast slice image: several well-circumscribed, isointense lesions.
d IR T2w slice image: lesions display partially high, partially low signal intensity.
e Early subtraction slice image: inhomogeneous enhancement.
f TIC: rapid initial enhancement (max. 100%–160%) and postinitial plateau.
The patient opted for the operative excision of the tumor.
Fig. 8.10a, b Giant fibroadenoma. Massive volume increase of the left breast.
a Subtraction MIP: size asymmetry caused by extremely large, wellcircumscribed, hypervascularized tumor with multiple dark internal septations in the left breast.
b IR T2w slice image: homogeneous high signal intensity with exception of the internal septations.
Operative excision of the tumor.
Juvenile fibroadenomas. These are rapidly growing lesions that appear during adolescence (i.e., puberty), and can reach a size of several centimeters. They make up ~0.5%–2% of all fibroadenomas (Fig. 8.9).
Giant fibroadenomas. These are large lesions with a diameter > 5 cm. They appear with a higher frequency during pregnancy and the lactation period (Fig. 8.10).
 MR Mammography: Juvenile and Giant Fibroadenomas
MR Mammography: Juvenile and Giant Fibroadenomas
T1-Weighted Sequence (Precontrast)
Round, oval, or lobulated lesion with an isointense or slightly hypointense signal in comparison with parenchyma (Fig. 8.9c).
T2-Weighted Sequence
Typically hyperintense signal (Fig. 8.9b). Internal septations or localized areas with a lower signal intensity are often seen (Fig. 8.10b).
T1-Weighted (Contrast Enhanced)
Strong, often inhomogeneous contrast enhancement (Figs. 8.9a, 8.10a). Dark internal septation and/or localized areas with reduced vascularization are typically seen (Figs. 8.9e, 8.10b). Sharp demarcation from surrounding tissue. TICs are uninformative, often showing a rapid initial enhancement and a postinitial plateau (Fig. 8.9f). They typically show no criteria that are suspicious for malignancy.
Adenomas
Adenomas of the breast are composed of benign epithelial elements with a sparse stromal component, features that differentiate them from fibroadenomas. Adenomas are commonly divided into two major groups: tubular adenomas and lactating adenomas. Tubular adenomas present in young women as well-circumscribed tumors composed of proliferating small tubular structures that are separated from adjacent breast tissue by an enveloping pseudocapsule. Lactating adenomas develop during pregnancy or the postpartum period and are composed of glands with an increased secretory activity.
The nipple adenoma is a rare, usually benign variant of intraductal papilloma involving the terminal portion of the nipple ducts. Microscopically there is a florid epithelial proliferation and adenosis, with a variable amount of sclerosis (Fig. 8.15).
Adenoma: General information | |
Incidence: | Rare breast tumor. |
Age peak: | Especially younger women. |
Risk of malignant transformation: | No increased risk. |
Multifocality: | Rare |
Findings | |
Clinical: | Small adenomas are clinically occult. Larger tumors are well-circumscribed, movable, painless nodules. |
Mammography: | Small adenomas are mammographically occult. Larger tumors appear round, oval, or lobulated, well-circumscribed, and homogeneously dense, and may display a halo sign. Occasional macrocalcifications; less common than in fibroadenomas. |
Ultrasonography: | Small adenomas are sonographically occult. Larger tumors appear round, oval, or lobulated, well-circumscribed, with a homogeneous internal echotexture. Moderate to strong posterior acoustic enhancement; possible bilateral acoustic shadowing. No or slight lesion compressibility. No criteria suspicious for malignancy. |
Adenomas of the breast show similar characteristics to fibroadenomas in the various imaging techniques. If there is uncertainty about the histology, a percutaneous biopsy is indicated to rule out malignancy (preferably ultrasound-guided). | |
 MR Mammography: Adenoma
MR Mammography: Adenoma
T1-Weighted Sequence (Precontrast)
Small adenomas are not usually visible in the precontrast examination. Larger tumors, especially when located within lipomatous tissue are well-circumscribed, round (Figs. 8.11b, 8.15a), oval (Fig. 8.13b) or lobulated (Figs. 8.12b, 8.14b) lesions with an isointense or slightly hypointense signal. Sometimes a halo sign may be present.
T2-Weighted Sequence
Usually inhomogeneous (Fig. 8.12c) or high signal intensity (Figs. 8.11c, 8.13c), comparable to the signal intensity of myxoid fibroadenomas. Occasional internal septations.
T1-Weighted (Contrast Enhanced)
Hypervascularized focus or mass lesion with round, oval or lobulated shape (Figs. 8.11a, 8.14a, d, e) and well-circumscribed borders. Usually homogeneous contrast enhancement (Figs. 8.11d, 8.13a, d). Occasional inhomogeneous enhancement (Fig. 8.12a,d). Rare dark internal septations. No rim enhancement. In most cases rapid initial enhancement (Fig. 8.11e) with variable postinitial signal behavior (Fig. 8.14f: persistent postinitial signal increase, Fig. 8.11e: plateau, or Figs. 8.13e and 8.15e washout).
Fig. 8.11a–e Small adenoma.
a Subtraction MIP: solitary focus (4 mm) in the retromamillary region of the right breast.
b T1w precontrast slice image: corresponding well-circumscribed, round, isointense lesion within surrounding lipomatous tissue.
c IR T2w slice image: homogeneous high signal intensity with horizontal septation (hamburger sign).
d Early subtraction slice image: homogeneous enhancement.
e TIC: unspecific dynamics with initial signal enhancement ~100% and postinitial plateau.
Fig. 8.12a–d Medium-sized adenoma.
a Subtraction MIP: solitary focus (4 mm) in the retromamillary region of the right breast.
b T1w precontrast slice image: corresponding well-circumscribed, round, isointense lesion within surrounding lipomatous tissue.
c IR T2w slice image: inhomogeneous, intermediary signal intensity.
d Early subtraction slice image: inhomogeneous enhancement. Because no suitable ROI placement is possible, no informative TIC can be plotted.
Fig. 8.13a–e Large adenoma.
a Subtraction MIP: well-circumscribed, oval, hypervascularized tumor in the left breast.
b T1w precontrast slice image: well-circumscribed, oval, isointense lesion.
c IR T2w slice image: inhomogeneous high signal intensity.
d Early subtraction slice image: homogeneous enhancement.
e TIC: rapid initial signal enhancement ~140% and postinitial washout.
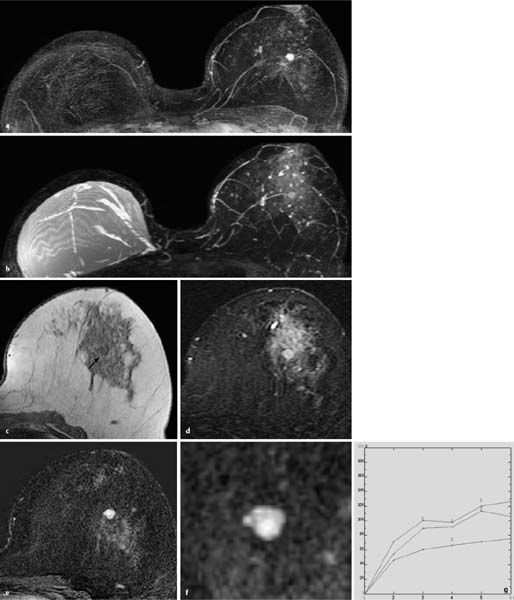
a Subtraction MIP: lobulated, hypervascularized mass lesions in the left breast. Additional bilateral harmless foci.
b T1w precontrast slice image: partially well-circumscribed, oval, isointense lesion within an area of parenchyma (arrow).
c IR T2w slice image: high signal intensity.
d Early subtraction slice image: inhomogeneous enhancement of a well-circumscribed, lobulated lesion.
e Zoomed subtraction image.
f TIC: moderate initial enhancement (max. 70%–90%) and persistent postinitial enhancement.
a Subtraction MIP: strong enhancement of parenchyma in both breasts. Round mass lesion with peripheral hypervascularization behind the left nipple.
b T1w precontrast slice image: widened isointense retromamillary region without clear demarcation of circumscribed lesion.
c IR T2w slice image: unremarkable findings.
d Early subtraction slice image: oval hypervascularized lesion behind the left nipple with thin rim-enhancement and intermediary vascularization of central tumor areas.
e TIC: varying curves due to difficult adequate placement of ROI. Conspicuous curve features are a rapid initial enhancement (> 100%) and a slight postinitial washout.
Benign Phyllodes Tumor
Synonyms: benign phyllodes tumor, fibroadenoma phyllodes.
The phyllodes tumor is a distinctive fibroepithelial tumor of the breast without counterpart in any other organ of the body. The benign form of this tumor is characterized by its structural similarity to the fibroadenoma, a low mitotic activity (0–4 mitoses/10 HPF at 400 × magnification [HPF = high power field]), no nuclear atypia, and a tumor growth pattern that displaces the surrounding tissue. The tumor stroma can show fibrous, lipomatous, chondral, myxoid, and myoid differentiation. In addition, tumors often show signs of hemorrhage and ulceration.
 MR Mammography: Benign Phyllodes Tumor
MR Mammography: Benign Phyllodes Tumor
T1-Weighted Sequence (Precontrast)
Benign phyllodes tumors are well-circumscribed round (Fig. 8.17b) or lobulated (Figs. 8.16c, 8.18a) lesions without pseudocapsular demarcation. Signal intensity is equivalent to that of parenchyma (isointense). Occasionally cystic or necrotic changes are seen as round inclusions with a comparatively hypointense signal.
T2-Weighted Sequence
Well-circumscribed round or lobulated lesion with iso- to hyperintense signal (Fig. 8.16b,d). Occasionally cystic or necrotic changes are seen as round inclusions with a hyperintense signal (Figs. 8.17c, g, 8.18b).
T1-Weighted (Contrast Enhanced)
The solid areas within a benign phyllodes tumor show a moderate to strong signal enhancement (Figs. 8.16a, e, f, 8.17d). In the course of the examination there is increasing demarcation of existing cystic or necrotic areas. Initial contrast enhancement is often > 100%. The postinitial signal phase usually displays a persistent increase or a plateau (Figs. 8.17e, i, 8.18d). If no liquid inclusions are seen, differentiation from a myxoid fibroadenoma is not possible.
Benign phyllodes tumor: General information | |
Incidence: | Rare breast tumor (~0.3% of all breast tumors). |
Age peak: | 30–50 years. |
Risk of malignant transformation: | No increased risk. Note: High local recurrence rate of ~30%. |
Findings | |
Clinical: | Rapidly growing, smooth or tuberous mass, diameter up to 10 cm or more. Larger tumors show skin changes (thinning and/or livid discoloration). |
Mammography: | Round or lobulated, well-circumscribed, homogeneously dense mass (similar to a fibroadenoma). Occasionally displays a halo sign due to compression of surrounding tissue. Rarely has micro- or macrocalcifications. |
Ultrasonography: | Round or lobulated, well-circumscribed mass with posterior acoustic enhancement. Cystic inclusions are a characteristic diagnostic attribute. |
The differential diagnosis between a phyllodes tumor and a fibroadenoma is occasionally difficult. Rapid growth and the documentation of cystic inclusions are indicative of a phyllodes tumor. Benign and malignant forms cannot be differentiated on the basis of imaging characteristics. The term “cystosarcoma phyllodes” is historical and should no longer be used. | |
Fig. 8.16a–g Benign phyllodes tumor.
a Subtraction MIP: hypervascularized, lobulated mass lesion in the left breast. Mastectomy and reconstruction with prosthesis implantation on the right after breast cancer.
b T2w MIP: relative high signal intensity (water content) of left lesion. Right silicone prosthesis shows harmless radial folds.
c T1w precontrast slice image (left breast): vague demarcation of a hypointense lesion.
d IR T2w slice image: lesion shows slightly elevated signal intensity relative to the surrounding parenchyma (water content).
e Early subtraction slice image: inhomogeneous hypervascularization within a well-circumscribed, lobulated lesion.
f Zoomed subtraction image.
g TIC: moderate initial enhancement (max. 50%–100%) and persistent postinitial enhancement.
Fig. 8.17a–i Benign bifocal phyllodes tumor.
a Subtraction MIP: two hypervascularized mass lesions with different configurations in the right breast. Incidental finding: size asymmetry.
b T1w precontrast slice image (right medial lesion): round, wellcircumscribed lesion.
c Corresponding IR T2w slice image: inhomogeneous water content.
d Corresponding early subtraction slice image: inhomogeneous hypervascularization.
e Unspecific TIC.
f T1w precontrast slice image (right central lesion): round lesion with halo sign (arrow).
g Corresponding IR T2w slice image: microcystic inclusions.
h Corresponding early subtraction slice image: inhomogeneous, confluent-nodular hypervascularization.
i TIC: moderate initial enhancement and persistent postinitial enhancement is indicative of a benign lesion.
Fig. 8.18a–d Benign phyllodes tumor.
a T1w precontrast slice image: oval, microlobulated lesion within surrounding fatty tissue (high signal intensity) of the right breast (arrow).
b Corresponding IR T2w slice image: few microcystic inclusions within lesion with inhomogeneous intermediary signal intensity.
c Corresponding early subtraction slice image: inhomogeneous hypervascularization with dark internal septations.
d TIC: moderate initial enhancement and persistent postinitial enhancement.
Lipomas
Lipomas of the breast are composed of encapsulated nodules of mature fat cells. These rare lesions must be differentiated from mixed tumors with macroscopically visible adipose tissue.
Subcutaneous lipomas can be located in the breast, as well as in other body areas.
 MR Mammography: Lipomas
MR Mammography: Lipomas
T1-Weighted Sequence (Precontrast)
Often oval, well-circumscribed lesion with hyperintense, fatequivalent signal. Occasionally a thin, hypointense capsule can be seen (Fig. 8.19b). No nonadipose internal structures.
T2-Weighted Sequence
Often oval, well-circumscribed lesion with intermediary signal intensity equivalent to that of subcutaneous fat. In fat suppressed sequences (e.g. IR T2w) lipomas will appear hypointense due to suppression of the fat peak (Note: fat suppression is usually stronger in a lipoma than in normal fat tissue) (Fig. 8.19c).
T1-Weighted Sequence (Contrast Enhanced)
No contrast enhancement (Fig. 8.19a,d).
Lipoma: General information | |
Incidence: | Rare breast tumor. |
Age peak: | All ages. |
Risk of malignant transformation: | No increased risk. |
Findings | |
Clinical: | Often occult. Occasionally soft, more rarely firm, movable nodule. |
Mammography: | Well-circumscribed, fully or partially encapsulated radiolucent tumor. |
Ultrasonography: | Large lesions are seen as well-circumscribed, highly compressible masses with an echogenicity similar to that of breast parenchyma. Note: Because the fat cells in lipomas are arranged differently than in normal fat tissue, they typically have a higher echogenicity. |
Lipomas of the breast are rare, usually clinically occult lesions, often demonstrated solely in mammography as an incidental finding. The mammographic appearance is pathognomonic and no further diagnostic examinations are necessary. | |
Fig. 8.19a–d Lipoma.
a Subtraction MIP: unremarkable findings with two harmless foci in the right breast (unchanged over years).
b T1w precontrast slice image: round, wellcircumscribed hyperintense mass in the left retromamillary region.
c Corresponding IR T2w slice image: complete suppression of internal lesion signal in fat-suppressed water-sensitive sequence.
d Corresponding early subtraction slice image: no lesion enhancement.
Fibrocystic Breast Condition
The term fibrocystic breast condition, synonymous with fibrocystic breast disease, fibrocystic changes, and mammary dysplasia, is used to describe a proliferation of hormone-dependent mesenchymal and epithelial structures of the breast. Fibrocystic breast condition encompasses a heterogeneous group of abnormalities that may occur separately or together. The morphological components, present in various degrees, comprise cysts, lobular hyperplasia, adenosis, ductal and alveolar hyperplasia (papillomatosis or epitheliosis), and stromal fibrosis. The etiology of such changes is presumed to be a hormonal imbalance.
 MR Mammography: Fibrocystic Breast Condition
MR Mammography: Fibrocystic Breast Condition
T1-Weighted Sequence (Precontrast)
Hypointense round lesions within breast parenchyma correlate with cystic component. No other specific changes (Fig. 8.20c) are seen.
T2-Weighted Sequence
Hyperintense lesions of various sizes (cysts) (Fig. 8.20b). Occasionally parenchyma displays a diffusely increased signal intensity (especially in the second half of the menstrual cycle and under hormonal stimulation).
T1-Weighted Sequence (Contrast Enhanced)
Breast parenchyma can display no, weak, or strong, sometimes patchy enhancement, leaving out the cystic lesions (Fig. 8.20a,d). Signal increases persistently within representative ROIs. Otherwise there are no specific changes. Note: Parenchymal enhancement in breast MRI does not correlate with the risk of malignant transformation.
Fibrocystic breast condition: General information | |
Incidence: | ~50% of all women. |
Age peak: | 40–60 years. |
Findings | |
Clinical: | Variable symptoms (small to middle-sized palpable lumps and increased diffuse breast firmness), usually symmetric. Symptoms fiuctuate with the menstrual cycle, peaking premenstrually. |
Mammography: | Often diffuse, rarely circumscribed structural hyperdensities, usually symmetric. Macro- and microcalcifications may be present, sometimes difficult to differentiate from malignancy. |
Ultrasonography: | Increased hyperechoic structures. Multiple hypoechoic tubular patterns (dilated ductal structures). Often multiple anechoic lesions with posterior acoustic enhancement (cysts). Usually symmetric findings. |
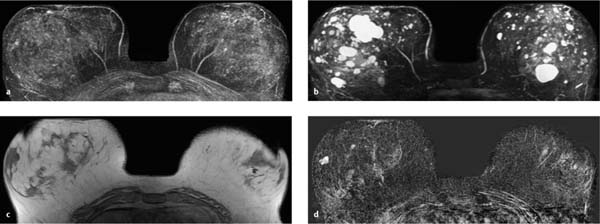
Fig. 8.20a–d Fibrocystic breast condition.
a Subtraction MIP: confluent-stippled enhancement in both breasts. No suspicious abnormalities.
b T2w MIP: diffuse distribution of multiple small and large cysts in both breasts.
c T1w precontrast slice image: representative example with multiple lesions in both breasts.
d Corresponding early subtraction slice image: lesions display varying degrees of vascularization (none to high).