as a surrogate for blood gas PCO2, to decrease or increase ventilatory support. IntelliVent® also uses SpO2 to decrease or increase PEEP and FiO2. The two ECPs were studied in children during the weaning phase and the first clinical studies are promising. However, further clinical trials are needed to better assess the efficacy and tolerance of these two ECPs in children and to develop ECP that are dedicated to all ages including neonates.
61.1 Introduction
Discontinuing mechanical ventilation as soon as it is no longer needed is crucial in preventing respiratory and prolonged sedation complications. The weaning process is described in a previous chapter (see section on weaning Part XXII) and can be summarised in six steps according to the sixth international consensus conference on intensive care medicine (Boles et al. 2007) including (1) suspicion that weaning may be possible, (2) assessment of readiness to wean, (3) spontaneous breathing trial (SBT) performed, (4) SBT passed, (5) extubation and (6) assessment of successful or failure of extubation (Fig. 61.1). Between each steps mechanical ventilation has to be adapted to reach the next step until no ventilator support is needed anymore. At present, two explicit computerised protocols on weaning children from mechanical ventilation are implemented in commercialised ventilators. This chapter describes these two explicit computerised protocols: Smartcare/PS® by Draeger Medical (Germany) and IntelliVent® by Hamilton Medical (Switzerland).
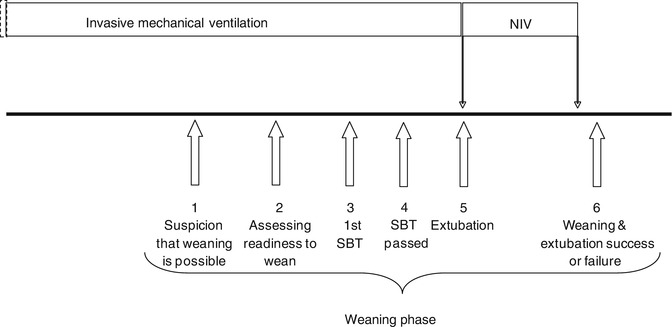
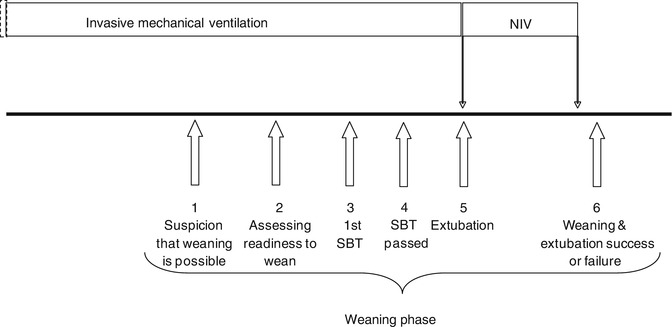
Fig. 61.1
Schematic representation of the different steps during weaning from mechanical ventilation in children
61.2 SmartCare/PS®: Draeger Medical
SmartCare/PS®—PS stands for pressure support—is an autopiloting, knowledge-based software application that provides an ECP for the automated control of pressure support ventilation. This ECP manages, without the need of caregivers intervention but under their supervision, the four following therapeutic procedures: (1) automatic adaptation of the pressure support level to keep the patient inside a “zone of respiratory comfort”, i.e. normal ventilation (see below); (2) a strategy to gradually and progressively decrease the level of pressure support level; (3) an automated SBT when the patient reaches a minimum ventilatory support; and (4) a recommendation of separation from the ventilator when the SBT is successfully passed (Table 61.1).
Table 61.1
Characteristics of the SmartCare/PS® Draeger Medical and IntelliVent® Hamilton Medical explicit computerised protocols
Characteristics | SmartCare/PS® | IntelliVent® |
|---|---|---|
Mode of ventilation | PS | ASV |
Body weight range for use (kg) | ≥15 | ≥7 |
Weaning steps managed (see Fig. 61.1) | 2–4 | 1–4 |
Primary goal of the ECP | Wean patient while maintained innormal ventilation (see Table 61.2) | To maintain in a normal  , RR and SpO2 ranges , RR and SpO2 ranges |
Initial settings | IBW, humidification system, medical history | IBW, medical history |
Setting modification displayed but needcaregiver prescription (open loop) | No | Yes |
Input data | 2min V t, 2minRR,  , PEEP, PS level, ventilator messages , PEEP, PS level, ventilator messages | RR,  , SpO2 , SpO2 |
Rules displayed to caregivers when applied | No | ± |
Output data | Parameter display, e.g. PS level | MV, PEEP, FiO2 |
Therapeutic messages “SBTsuccessful” | SBT duration | |
SBT | Yes | Yes |
SBT duration | 1–2 h according to initial PS level(Jouvet et al. 2007) | Adjustable |
Recommendation of separation from the ventilator | Yes | No |
SmartCare/PS® is available on Draeger’s Evita XL and the latest generation of Draeger Medical ventilators: Evita Infinity V500. It is applicable in two applications that slightly differ: (a) for patients with ideal body weight (IBW) between 15 kg and 35 kg as well as for (b) patients with IBW between 36 kg and 200 kg. The ECP comprises of the three different phases “adaptation”, “observation” and “maintain” to perform ventilation procedures (1) to (4). It will also manage patient instabilities, e.g. transient tachypnoea, and it can cope with certain patient care situations like suctioning and pauses during specialised therapeutic situations like nebulisations or during specific ventilator alarm.
61.2.1 Basics of SmartCare/PS®
61.2.1.1 Initiation of SmartCare/PS®
Initiating SmartCare/PS® is recommended when a child, with IBW greater than 15 kg, fulfils ready-to-wean criteria that were used in two prospective clinical studies (Jouvet et al. 2007; Jouvet et al. 2010a). These weaning criteria are as follows:
The attending physician evaluates that the patient is able to breathe spontaneously or the patient is already breathing spontaneously.
No significant vasopressors or inotropic medications, excluding digoxin or low-dose dopamine (≤5 μg/kg/min).
Slight or no endotracheal tube gas leakage ([V ti−V te]/V ti ≤20 %).
Mechanical ventilation with a plateau pressure above PEEP ≤25 cmH2O.
PEEP ≤8 cmH2O.
FiO2 ≤60 % with SpO2 ≥95 %.
Pressure support test passed. During the pressure support test, the patient is mechanically ventilated in pressure support mode for 30 min, with a level of pressure support set to ±5 cmH2O of the current plateau pressure. The pressure support test is stopped before 30 min if the patient shows evidence of respiratory distress (respiratory rate below 10 breaths per min or above 40 breaths per minute and FiO2 >60 % in order to obtain a SpO2 ≥95 %). The test is passed when, after 30 min, the patient remains stable with a respiratory rate between 10 and 40 breaths per min, an expiratory tidal volume higher than 6 ml/kg and SpO2 ≥95 % with FiO2 ≤0.6.
When the child fulfils all the above mentioned criteria, IBW, which is also a surrogate for lung volume (see chapter on explicit computerised protocols), is prescribed on the ventilator by the user. The next step is to prescribe the humidification system and the medical history (presence or not of neurologic disorders or COPD) if the child’s IBW is above 35 kg. These user-given settings will determine certain thresholds and specific rules of the ECP (Table 61.2).
Table 61.2
Normal ventilation definition in SmartCare/PS®
Definition | Parameters value | IBW ≤35 kg | 35 kg <IBW ≤55 kg | IBW >55 kg |
|---|---|---|---|---|
Normal ventilation: | RR low (bpm) | 18 | 10–15 | 10–15 |
RR low ≤ RR < RR high | RR high (bpm) | 40 | 20–40 | 20–40 |
34 for COPD & neurological disorders | 34 for COPD & neurological disorders | |||
V T low ≤ V T | V t low | 6 ml/kg | 250 ml | 300 ml |
 < <  high high |  (mmHg) (mmHg) | 55 | 45–65 | 45–65 |
65 for COPD | 65 for COPD | |||
RR max (bpm) | 50 | 36 | 36 | |
61.2.1.2 Primary Goal: To Safely Maintain the Child in a Zone of Respiratory Comfort (Normal Ventilation)
In contrast to conventional ventilation modes, SmartCare/PS® continuously adapts the pressure support level to maintain normal ventilation. Normal ventilation corresponds to a respiratory pattern that is determined by lower and upper thresholds of tidal volume, respiratory rate and  (Table 61.2). In turn, these thresholds are defined within acceptable limits as reported by a large panel of paediatric intensivists (Santschi et al. 2007). To keep the patient in normal ventilation, the pressure support level is increased or decreased according to the implemented rules of the knowledge base that represents the ECP (Fig. 61.2) (Mersmann 2009).
(Table 61.2). In turn, these thresholds are defined within acceptable limits as reported by a large panel of paediatric intensivists (Santschi et al. 2007). To keep the patient in normal ventilation, the pressure support level is increased or decreased according to the implemented rules of the knowledge base that represents the ECP (Fig. 61.2) (Mersmann 2009).
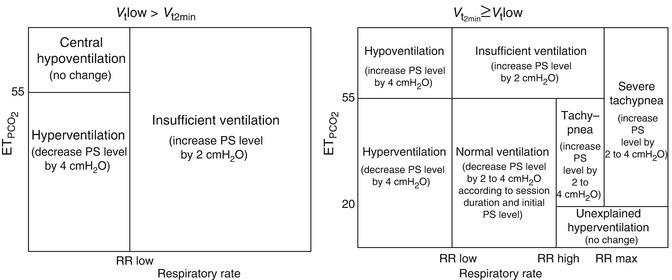
 (Table 61.2). In turn, these thresholds are defined within acceptable limits as reported by a large panel of paediatric intensivists (Santschi et al. 2007). To keep the patient in normal ventilation, the pressure support level is increased or decreased according to the implemented rules of the knowledge base that represents the ECP (Fig. 61.2) (Mersmann 2009).
(Table 61.2). In turn, these thresholds are defined within acceptable limits as reported by a large panel of paediatric intensivists (Santschi et al. 2007). To keep the patient in normal ventilation, the pressure support level is increased or decreased according to the implemented rules of the knowledge base that represents the ECP (Fig. 61.2) (Mersmann 2009).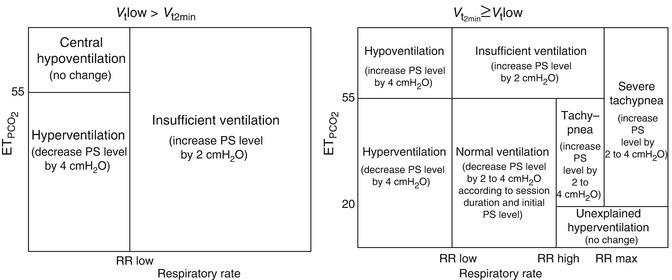
Fig. 61.2
Classification of ventilation by SmartCare/PS® Draeger Medical. Pressure support level is modified according to values of tidal values (below Vtlow: panel a, above Vtlow: panel b), respiratory rate and end-tidal PCO2 at 2–5 min intervals (SmartCare waits 2 min for the next “Classification of Ventilation” if PS was not changed and waits 5 min if PS was changed (either by SmartCare or by the user))
61.2.1.3 Weaning of Ventilatory Support
When the child remains in normal ventilation for a predefined period of time (60, 30 and finally 15 min), the PS level is gradually decreased (Jouvet et al. 2007), which is called a regular weaning step. During the entire execution of the ECP, duration of stability and duration of instabilities are balanced and taken into account when assessing the patient’s needs. When the patient’s respiratory pattern is outside the limits of normal ventilation, an instability is noted. A maximum of two instabilities will be tolerated by SmartCare/PS® before the pressure level will be increased.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





