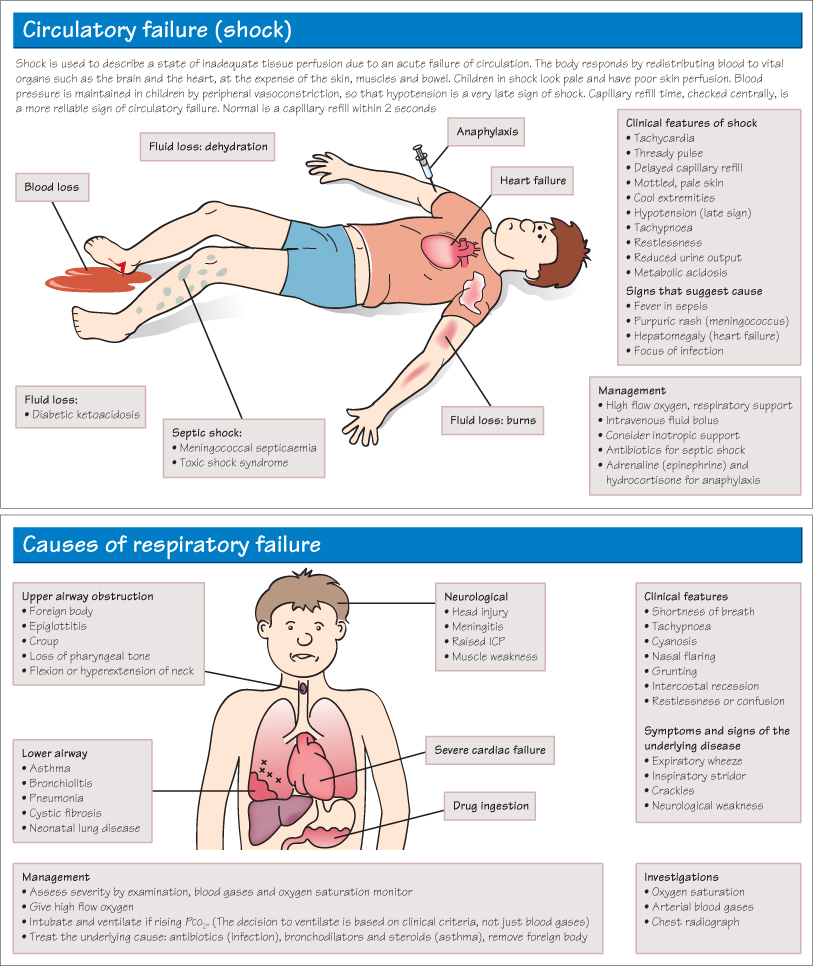
Respiratory Failure
Respiratory failure is defined as inadequate respiration to maintain normal arterial oxygen and carbon dioxide concentrations. Respiratory failure is obvious if the child is apnoeic or deeply cyanosed, but it is important to be able to detect impending respiratory failure and to intervene quickly. Tachypnoea >50/min, grunting and oxygen saturation <95% are signs of serious respiratory distress.
Acute Upper Airway Obstruction
Acute upper airway obstruction is a medical emergency. It can be due to infection (epiglottitis, croup) or inhalation of a foreign body (especially common in toddlers who put small objects in their mouths). Presentation is with acute sudden onset of choking, coughing and cyanosis, followed by collapse. There may be an inspiratory stridor (see Chapter 24) and marked intercostal recession. If epiglottitis is suspected do not examine the child’s throat. The management of choking is described in Chapter 56.
Septic Shock
Meningococcal septicaemia is one of the most life-threatening causes of septic shock and is due to Gram-negative diplocccus Neisseria meningitides infection. 40–50% will present with meningitis (see Chapter 57), 40% with meningitis and septicaemia and 10% with septicaemia alone. Within hours of the onset of non-specific flu-like symptoms, a rash develops. This may initially be erythematous or petechial but rapidly becomes purpuric. Parents are advised to perform the ‘glass test’ (pressing on the skin with a glass beaker—see Chapter 52) to check whether any rash is non-blanching and seek urgent medical advice if positive.
Meningococcal disease should be suspected if there is:
- Fever and a non-blanching rash, especially if also
- The child looks ill
- The non-blanching lesions are >2 mm (purpura)
- There is neck stiffness
- The capillary refill time is ≥3 seconds.
Fulminant septicaemia can develop within hours, leading to endotoxin-mediated severe septic shock and coma. The case fatality rate is around 10%. Any child with purpura and a fever should be given intramusular ceftriaxone and transferred to hospital immediately. The meningococcus C vaccine does not protect against the more common B strain. As 20–30% of the population may be nasopharyngeal carriers of Neisseria meningitides, close contacts should be given rifampicin prophylaxis.
Staphylococcal toxic shock syndrome presents very acutely with high fever, muscle pain, a desquamating rash and severe circulatory failure. It is mediated by Staphyloccocus aureus exotoxins. The original site of infection may be trivial, such as a graze, or in girls may be associated with menstruation. Circulatory support and high-dose antibiotic treatment with flucloxacillin or clindamycin is required.
Neurological Warning Signs
Signs of an actual or impending serious neurological disorder include
- Drowsiness, lethargy or other altered level of consciousness
- Severe headache, especially if associated with vomiting
- Irritability or a high-pitched cry
- Bulging fontanelle (infants)
- Neck stiffness
- Sudden onset of muscle weakness
- Any new cranial nerve lesion
- Abnormal movements
- Convulsions
These signs should prompt a thorough search for the cause. Consider raised intracranial pressure, central nervous system (CNS) infection and whether neuroimaging with CT or MRI scan is required.
KEY POINTS
- Early recognition of impending cardiorespiratory failure is vital.
- Irritability may be an early sign of hypoxia or CNS infection.
- A non-blanching rash in an ill child should be assumed to be meningococcal septicaemia and is a medical emergency.



