Anterior Mediastinal Mass
Eric J. Crotty, MD
DIFFERENTIAL DIAGNOSIS
Common
Normal Thymus
Rebound Thymic Hyperplasia
Lymphoma
Less Common
Germ Cell Tumor
Lymphatic Malformation
Thymic Cyst
Rare but Important
Langerhans Cell Histiocytosis
Morgagni Hernia
ESSENTIAL INFORMATION
Helpful Clues for Common Diagnoses
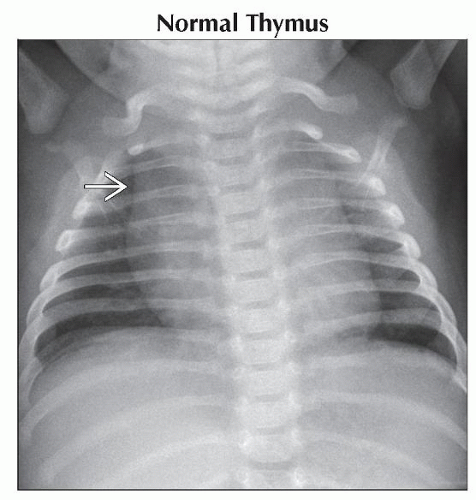
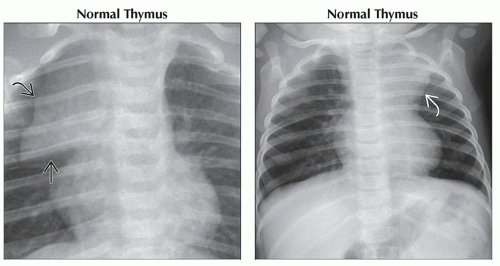
Normal Thymus
Most common anterior mediastinal “mass” in neonates and infants
Has quadrilateral shape in infancy
Gradually becomes triangular-shaped in later childhood and teenage years
Thymus increases in weight until adolescence when it begins to involute
Most prominent in infancy
Visible on frontal radiograph until ˜ 5 years of age
Appearance may change with phase of respiration
Look for “spinnaker sail” sign, “notch” sign, and “wave” sign
May be asymmetric across midline
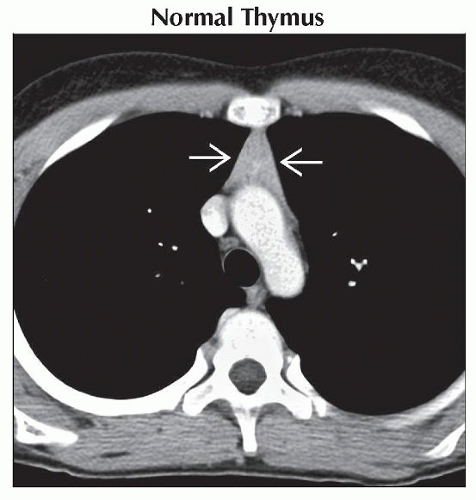
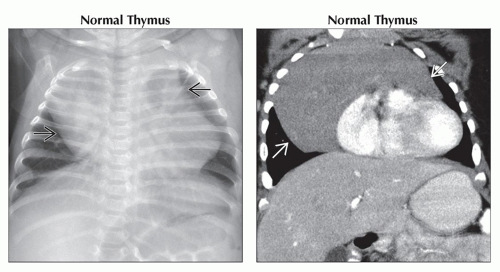
Can extend inferiorly to drape over heart, superiorly into neck, or posteriorly to involute between great vessels and trachea
Homogeneous appearance on CT and MR, enhancing homogeneously following contrast administration
Typical sonographic appearance of multiple linear echoes and discrete echogenic foci
Rebound Thymic Hyperplasia
Thymus can vary in size depending on intercurrent illness and stress
May decrease in size during illness/stress and with subsequent increase in size with recovery
Stressors include burns, surgery, and chemotherapy
Maintains normal attenuation and signal on CT and MR respectively
Maintains normal configuration on cross sectional imaging
Also maintains normal gross architecture and histologic appearance
Lymphoma
Most common anterior mediastinal mass in teenagers
Distorts shape of thymus, which assumes lobulated or biconvex contour
Mass usually crosses midline
May be homogeneous or heterogeneous soft tissue mass on CT and MR
Positron emission tomography (PET) imaging best identifies involved nodes and extent of involvement elsewhere
May become more heterogeneous while it is being treated or if it rapidly enlarges and outgrows blood supply
May be associated with involvement of lymph nodes in hila and in other mediastinal compartments
Pleural and pericardial involvement, especially effusions, not uncommon; lung involvement is unusual
May displace trachea and vessels
Superior vena caval invasion and occlusion may cause SVC syndrome
Helpful Clues for Less Common Diagnoses
Germ Cell Tumor
Pediatric patients (˜ 66%) usually present with symptoms
2nd most common extragonadal site after sacrococcygeal region
Occurs within or near thymus
Majority are mature teratomas (60%); seminoma is next most common
Less common are teratocarcinoma, endodermal sinus tumor, choriocarcinoma, and embryonal cell carcinoma
Tumors have lobulated or smooth contour on radiography; constituent elements may be identified, especially calcification
Intrinsic elements are better identified on CT
CT appearances may be homogeneously cystic or soft tissue in appearance, contain well-demarcated fat, fluid, soft tissue, or calcific elements, or may have heterogeneous soft tissue appearance
Calcifications are usually coarse
May be well demarcated or inseparable from vascular structures
Tumors are more commonly unilateral but may extend across midline
Lymphatic Malformation
Formerly called cystic hygroma or lymphangioma
Usually detected on prenatal imaging or in neonatal period
Most often represents mediastinal extension from neck lesion but can be solely mediastinal
May be associated with more generalized lymphatic problem
Thin-walled fluid-filled structure, which may be focal but may also be multifocal or infiltrative and involve mediastinal compartments
Thymic Cyst
May extend superiorly into neck between carotid artery and jugular vein
Usually thin walled and fluid filled
Rarely may have partial wall calcification
Can be congenital or postinflammatory
Helpful Clues for Rare Diagnoses
Langerhans Cell Histiocytosis
Thymic involvement occurs commonly in multisystem disease
Most commonly presents as diffuse enlargement but can have focal lesion, usually cystic area on CT
Contour may be smooth or lobulated
Involved thymus is heterogeneous in appearance on CT and MR
Irregular calcifications and cystic lesions may be present
Calcifications are usually subtle in comparison to those seen in germ cell tumors and are usually only visible on CT
Enlarged, involved gland can displace trachea and great vessels, unlike normal thymus
Appearance of thymus reverts to normal with therapy
Morgagni Hernia
Anteromedial parasternal defect of diaphragm, adjacent to xiphoid process
90% occur on right side; right cardiophrenic angle on radiography
More commonly asymptomatic than Bochdalek type of congenital diaphragmatic hernia
Contents of hernia are variable but most commonly contain omentum with liver and bowel less common; contents determine radiographic appearance
Nature of contents is more easily assessed on CT and MR
Occasionally diagnosed on barium study
Image Gallery
 (Left) Anteroposterior radiograph shows a large cardiomediastinal silhouette
 . On a lateral view, this was seen to be confined to the anterior mediastinum. The thymus is variable in size and shape, which depends on multiple variables, including the age and health of the patient. It can extend into the neck or other compartments of the mediastinum. (Right) Coronal CECT shows the typical homogeneous attenuation of the thymus draping over the heart . On a lateral view, this was seen to be confined to the anterior mediastinum. The thymus is variable in size and shape, which depends on multiple variables, including the age and health of the patient. It can extend into the neck or other compartments of the mediastinum. (Right) Coronal CECT shows the typical homogeneous attenuation of the thymus draping over the heart  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|