Classification
Placenta praevia is classified according to the proximity of the placenta to the internal os of the cervix. It may be predominantly on the anterior or posterior uterine wall.
Aetiology
This is unknown, but placenta praevia is slightly more common with twins, in women of high parity and age, and if the uterus is scarred (e.g. previous Caesarean) (J Matern Fetal Neonatal Med 2003; 13: 175).
Complications
The placenta in the lower segment obstructs engagement of the head: except for some marginal praevias, this necessitates Caesarean section and may also cause the lie to be transverse. Haemorrhage can be severe and may continue during and after delivery as the lower segment is less able to contract and constrict the maternal blood supply. If a placenta implants in a previous Caesarean section scar, it may be so deep as to prevent placental separation (placenta accreta) or even penetrate through the uterine wall into surrounding structures such as the bladder (placenta percreta). Placenta accreta occurs in 10% of women who have both a placenta praevia and a single previous caesarean scar. This may provoke massive haemorrhage at delivery, often requiring hysterectomy.
Clinical Features
History:
Typically, there are intermittent painless bleeds, which increase in frequency and intensity over several weeks. Such bleeding may be severe. One-third of women, however, have not experienced bleeding before delivery.
Examination:
Breech presentation and transverse lie are common. The fetal head is not engaged and high. Vaginal examination can provoke massive bleeding and is never performed in a woman who is bleeding vaginally unless placenta praevia has been excluded.
Presentation of Placenta Praevia
Incidental finding on ultrasound scan
Vaginal bleeding
Abnormal lie, breech presentation
Investigations
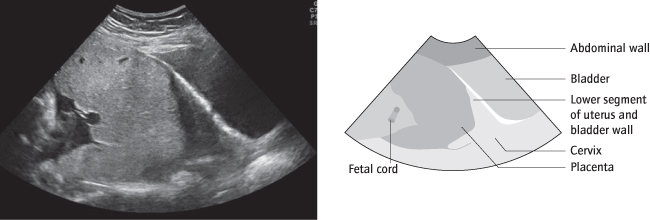
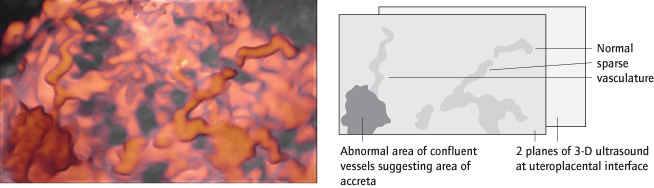
To make the diagnosis, ultrasound is used (Fig. 24.2). Most placenta praevias are now diagnosed prior to any bleeding. If a low-lying placenta has been diagnosed at a second trimester ultrasound, this is repeated, vaginally if the placenta is posterior, at 32 weeks to exclude placenta praevia. A placenta <2 cm from the internal os is likely to be praevia at term. If the placenta is anterior, and under a caesarean section scar, 3-D power ultrasound (Fig. 24.3) is best to determine if there is placenta accreta (Ultrasound Obstet Gynecol 2009; 33:193). This is to be prepared for haemorrhage at delivery.
To Assess Fetal and Maternal Well-Being:
where presentation is with bleeding, cardiotocography (CTG), a full blood count (FBC), clotting studies and cross-match are needed. Fetal distress [→ p.252] is uncommon.
Management
Admission
This is necessary for all women with bleeding. If placenta praevia is then found on ultrasound, such women often stay in hospital until delivery because of the risk of massive haemorrhage. Blood is kept available; anti-D is administered to rhesus negative women; intravenous access is maintained; steroids [→ p.206] are administered if the gestation is <34 weeks. In women with asymptomatic placenta praevia, admission can be delayed until 37 weeks or delivery, provided they can get to hospital easily.
Delivery
This is by elective Caesarean section at 39 weeks by the most senior person available. Intraoperative and postpartum haemorrhage are common because the lower segment does not contract well after delivery. Earlier, emergency delivery is needed if bleeding is severe before this time. Very preterm, pregnancy can often be prolonged with observation and, if necessary, blood transfusion.
Placenta accreta or percreta [→ p.209] should have been anticipated, although the placenta may also occasionally invade the myometrium even if it is not praevia or over a scar. Where it is anticipated, the uterine incision is made away from the placenta, which can be left in situ, or removed with the entire uterus. Partial separation or transection of the placenta by the uterine incision may provoke massive haemorrhage: treatment involves either compression of the inside of the scar after removal of the placenta with an inflatable (e.g. Rusch) balloon or, frequently, hysterectomy.
Differentiation between Placental Abruption and Placenta Praevia
| Abruption | Placenta praevia | |
| Shock: | Inconsistent with external loss | Consistent with external loss |
| Pain: | Common, often severe | No. Contractions occasionally |
| Constant with exacerbations | ||
| Bleeding: | May be absent | Red and often profuse |
| Often dark | Often smaller previous antepartum haemorrhage (APHs) | |
| Tenderness: | Usual, often severe | Rare |
| Uterus may be hard | ||
| Fetus: | Lie normal, often engaged | Lie often abnormal/ head high |
| May be dead or distressed | Heart rate usually normal | |
| Ultrasound: | Often normal, placenta not low | Placenta low |
Placental Abruption
Definition
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree