Antepartum Fetal Assessment
The methods and means for assessing the fetus during the antepartum are selected based on gestational age, patient history and presentation, patient and practitioner preferences, and available technology. The purpose of antepartum testing is to screen for adequacy of uteroplacental function and to determine whether the fetus can safely remain in utero. It is important to consider that antepartum tests currently available are very effective for predicting fetal well-being but are not capable of making definitive diagnosis of fetal hypoxia/acidosis. Antepartum surveillance is also indicated for other conditions affecting or suspected to affect the maternal-fetal unit (see Table 4-1). The American Academy of Pediatrics (AAP) and American College of Obstetricians and Gynecologists (ACOG) have issued research-based guidelines that delineate testing criteria and procedures.1,2
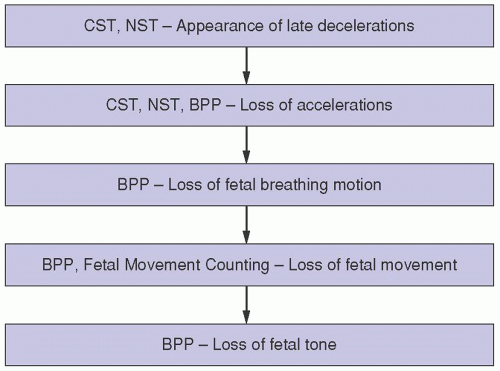
Understanding maternal-fetal physiology is essential to selecting, performing, and managing antepartum testing. The fetal central nervous system matures as gestation advances, and the resulting behaviors that the fetus demonstrates develop in a specific order. Antepartum testing methods assess the fetus for its ability to perform behaviors appropriate to its gestational age in an effort to identify or rule out developing fetal asphyxia. An insidious, chronic loss of oxygenation causes the term or near-term fetus to lose the ability to perform expected functions. This decline in fetal status occurs on a continuum, in an opposite order from which abilities develop (Figure 4-1). Fetal tone begins to be evident by sonographic evaluation at approximately 7.5 to 8 weeks’ gestation followed by fetal movement, which starts to occur at approximately 9 weeks. Fetal breathing becomes regular at 20 to 21 weeks. Heart rate control (the ability to accelerate and decelerate) is last to develop, presenting at the end of the second or beginning of the third trimester.
TABLE 4-1 INDICATIONS FOR ANTEPARTUM FETAL SURVEILLANCE | ||||||
|---|---|---|---|---|---|---|
| ||||||
NONSTRESS TEST
The nonstress test (NST) involves the application of an electronic fetal monitor (EFM) to the maternal abdomen for the purpose of evaluating the fetus’s
ability to perform a specified number of fetal heart rate (FHR) accelerations within a specified period of time. If the fetus is able to accomplish this task, the test is deemed reactive. If the fetus is not able to produce the desired amount of FHR accelerations within the allotted time frame, the test is considered to be nonreactive. The fetus is typically given at least 40 minutes of testing time to produce a reactive NST. This is to allow for the possibility that the time of testing might coincide with a period of fetal sleep. The NST is noninvasive and relatively easy to perform. Activities that affect fetal movement patterns and uteroplacental perfusion (e.g., maternal nutrition, hydration, smoking habits, medication effects, positioning, and time of day) should be considered when scheduling and performing the NST.
ability to perform a specified number of fetal heart rate (FHR) accelerations within a specified period of time. If the fetus is able to accomplish this task, the test is deemed reactive. If the fetus is not able to produce the desired amount of FHR accelerations within the allotted time frame, the test is considered to be nonreactive. The fetus is typically given at least 40 minutes of testing time to produce a reactive NST. This is to allow for the possibility that the time of testing might coincide with a period of fetal sleep. The NST is noninvasive and relatively easy to perform. Activities that affect fetal movement patterns and uteroplacental perfusion (e.g., maternal nutrition, hydration, smoking habits, medication effects, positioning, and time of day) should be considered when scheduling and performing the NST.
The occurrence of two or more accelerations, each rising to ≥15 beats above the FHR baseline and lasting for a period of ≥15 seconds, accomplished within a 20-minute time frame constitutes a reactive NST.1,3,4 A detailed explanation of accelerations is provided in Chapter 3. It is expected that the fetus should be able to meet these criteria by 32 weeks’ gestation. Although not included in the standard definition of a reactive NST, it is reasonable to expect that a fetus meeting these criteria will also demonstrate moderate baseline FHR variability. The FHR baseline would also be expected to fall within normal limits (110-160 bpm).
Some fetuses are able to produce a reactive NST as early as 24 to 28 weeks’ gestation; however, there is a high false-positive rate (as much as 50%) in this population.4 Between 28 and 32 weeks’ gestation, there is a 15% chance that the NST will be nonreactive because the fetal autonomic nervous system may not have reached the maturity necessary to accelerate the fetal heart per NST criteria.5,6 However, when such development is exhibited at an early gestational age, it is expected that the fetus will continue to achieve a reactive result of the same or better standard during all subsequent monitoring sessions.
I am growing up so quickly! Now that I am mature enough to give you a reactive NST, I should do this well or even better every time you test me! If not, beware!
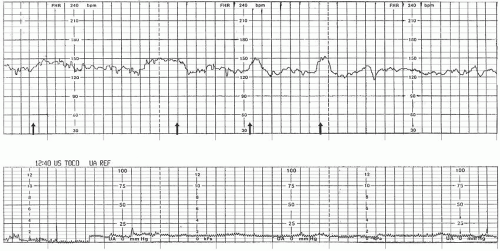
There are variations in the parameters used to define the NST and its results. Both the period of time in which the NST is performed and the number of accelerations required during the defined period to deem the test reactive differ among institutions. Another variation of the NST includes the definition of a qualifying acceleration. Although the standard definition is that the accelerations rise above the baseline by ≥15 bpm and last ≥15 seconds, this definition may vary based on gestational age. For a fetus of less than 32 weeks’ gestation, accelerations of ≥10 bpm that last ≥10 seconds in length are acceptable,7 providing that the fetus has not previously demonstrated ≥15 bpm × ≥15 second accelerations. Implicit understanding of NST performance requirements and results in various institutions may differ to some degree. For example, some institutions may require documentation and/or correlation of instances of perceived fetal movement with accelerations during the NST (Figure 4-2). For clarity and accuracy, it is necessary to be aware of and follow institutional policy.
When the result of the NST is reactive, the patient will most likely be scheduled for testing on a weekly or twice-weekly basis, depending on gestational age and the indication for antepartum surveillance. Women who have maternal or obstetric indications that require twice-weekly testing include, but are not limited to, those with a post-term gestation, intrauterine growth restriction, type 1 diabetes mellitus, and pregnancy-induced hypertension.1,2 Some high-risk conditions may warrant testing on a more frequent basis. Isolated episodes that occur during a normal-risk pregnancy that warrant performance of an NST (such as complaint of decreased fetal movement) and are subsequently ruled out might not be followed with any regular schedule of testing. A reactive NST has a negative predictive value of 99.8%, meaning that the possibility of stillbirth occurring within 1 week after a reactive NST is extremely low.8
If the NST is reactive, but the FHR demonstrates additional components such as variable, late, or prolonged decelerations (Category II tracing), continued monitoring and further evaluation are indicated. If variable decelerations are brief (<30 seconds in length) and occur infrequently, they do not require intervention.9 If repetitive variable decelerations are present, measurement of the amniotic fluid volume by sonographic examination will determine if oligohydramnios is the underlying cause of this pattern (Figure 4-3). It is well established that oligohydramnios is associated with increased perinatal morbidity and mortality10 and requires immediate attention and possible intervention. Further sonographic
examination may reveal structural anomalies of the maternal-fetal unit that may be causing decelerations of the FHR to occur.
examination may reveal structural anomalies of the maternal-fetal unit that may be causing decelerations of the FHR to occur.
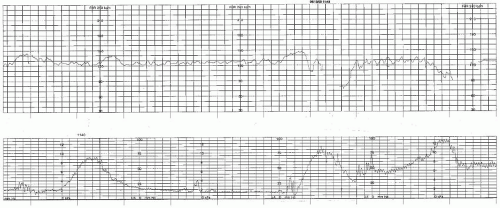
If the NST is judged to be nonreactive, meaning that there are no accelerations or an insufficient number of accelerations produced during a 40-minute time period (extended length of time to account for fetal sleep cycles), additional testing of the fetus is indicated. Intervention is not based solely on a non-reactive NST because 80% to 90% of the nonreactive tracings are due to fetal sleep and are not the result of hypoxia (Figure 4-4).11,12
A nonreactive NST that also demonstrates non-reassuring signs, particularly in combination (e.g., variable, late, or prolonged decelerations; marked or minimal/absent variability; a baseline rate that is not within normal limits; or a sinusoidal pattern), is of great concern. Such findings warrant immediate investigation and possible consideration of the need for delivery.
In summary, whether the tracing is considered reactive or nonreactive, if any part of the tracing is indicative of a FHR pattern not predictive of normal fetal acid-base status, further evaluation is needed.
This may consist of any one or a combination of the tests mentioned in this chapter. It is important to understand that, although the NST is an effective screening tool for the evaluation of fetal well-being and is often used as the primary method of testing, it has poor positive predictive value for determining fetal hypoxia/acidosis.13 Adjunct methods of assessment should be employed any time fetal status is in question.
This may consist of any one or a combination of the tests mentioned in this chapter. It is important to understand that, although the NST is an effective screening tool for the evaluation of fetal well-being and is often used as the primary method of testing, it has poor positive predictive value for determining fetal hypoxia/acidosis.13 Adjunct methods of assessment should be employed any time fetal status is in question.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree