Chapter 538 Anomalies of the Penis and Urethra
Hypospadias
Clinical Manifestations
Hypospadias is classified according to the position of the urethral meatus after taking into account whether chordee is present (Fig. 538-1). The deformity is described as glanular (on the glans penis), coronal, subcoronal, midpenile, penoscrotal, scrotal, or perineal. Approximately 60% of cases are distal, 25% are subcoronal or midpenile, and 15% are proximal. In the most severe cases, the scrotum is bifid and sometimes there is moderate penoscrotal transposition. As many as 15% of affected boys have a megameatal variant, in which the foreskin is developed normally (megameatus intact prepuce [MIP] variant), and there is either glanular or subcoronal hypospadias with a “fish mouth” meatus. These cases might not be diagnosed until after a circumcision is performed.
Approximately 10% of boys with hypospadias have an undescended testis; inguinal hernias also are common. In the newborn, the differential diagnosis of proximal hypospadias associated with an undescended testis should include forms of a disorder of sexual differentiation, particularly female virilization (congenital adrenal hyperplasia), mixed gonadal dysgenesis, partial androgen insensitivity, and true hermaphroditism. A karyotype should be obtained in patients with midpenile or proximal hypospadias and cryptorchidism (Chapter 577). In boys with penoscrotal hypospadias, a voiding cystourethrogram should be considered because 5-10% of these children have a dilated prostatic utricle, which is a remnant of the müllerian system (Chapter 548). The incidence of upper urinary tract abnormalities is low unless there are abnormalities of other organ systems.
Chordee without Hypospadias
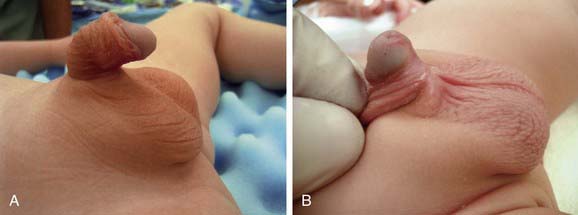
In some boys there is mild or moderate ventral penile curvature (chordee) and incomplete development of the foreskin (dorsal hood), but the urethral meatus is at the tip of the glans (Fig. 538-2). In most of these boys, the urethra is normal but there is insufficient ventral penile skin or prominent, inelastic ventral bands of dartos fascia that prevent a straight erection. In some cases, the urethra is hypoplastic, and a formal urethroplasty is necessary for repair. The only sign of this anomaly in the neonate may be the hooded foreskin, and delayed repair under general anesthesia at 6 mo of age is recommended.
Phimosis and Paraphimosis
Phimosis refers to the inability to retract the prepuce. At birth, phimosis is physiologic. Over time, the adhesions between the prepuce and glans lyse and the distal phimotic ring loosens. In 90% of uncircumcised boys the prepuce becomes fully retractable by 3 yr of age. Accumulation of epithelial debris under the infant’s prepuce is physiologic and does not mandate circumcision. In older boys, phimosis may be physiologic, may be pathologic from inflammation and scarring at the tip of the foreskin (Fig. 538-3), or occurs after circumcision. The prepuce might have been retracted forcefully on 1 or 2 occasions in the past, which can result in a cicatricial scar that prevents subsequent retraction of the foreskin. In boys with persistent physiologic or pathologic phimosis, application of corticosteroid cream to the foreskin 3 times daily for 1 mo loosens the phimotic ring in 2/3 of cases. If there is ballooning of the foreskin during voiding or phimosis beyond 10 yr of age and topical corticosteroid therapy is ineffective, circumcision is recommended.
Paraphimosis occurs when the foreskin is retracted past the coronal sulcus and the prepuce cannot be pulled back over the glans (Fig. 538-4). Painful venous stasis in the retracted foreskin results, with edema leading to severe pain and inability to reduce the foreskin (pull it back over the glans). Treatment includes lubricating the foreskin and glans and then simultaneously compressing the glans and placing distal traction on the foreskin to try to push the phimotic ring past the coronal sulcus. In rare cases, emergency circumcision under general anesthesia is necessary.
Circumcision
UTIs are 10-15 times more common in uncircumcised infant boys than in circumcised infants, with the urinary pathogens arising from bacteria that colonize the space between the prepuce and glans. The risk of febrile UTI (Chapter 532
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree