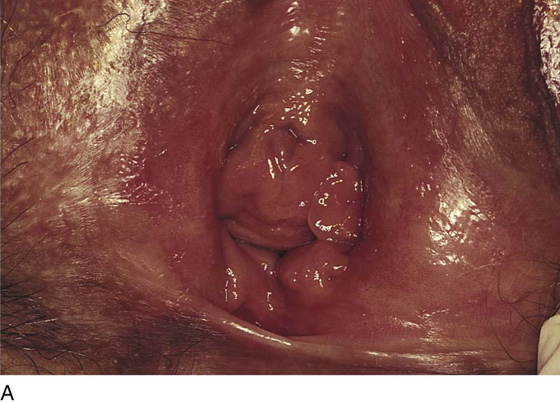
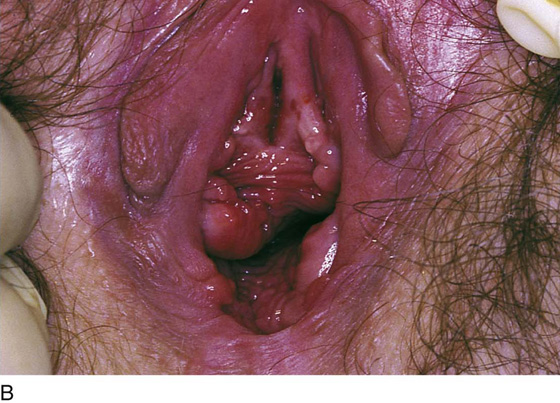
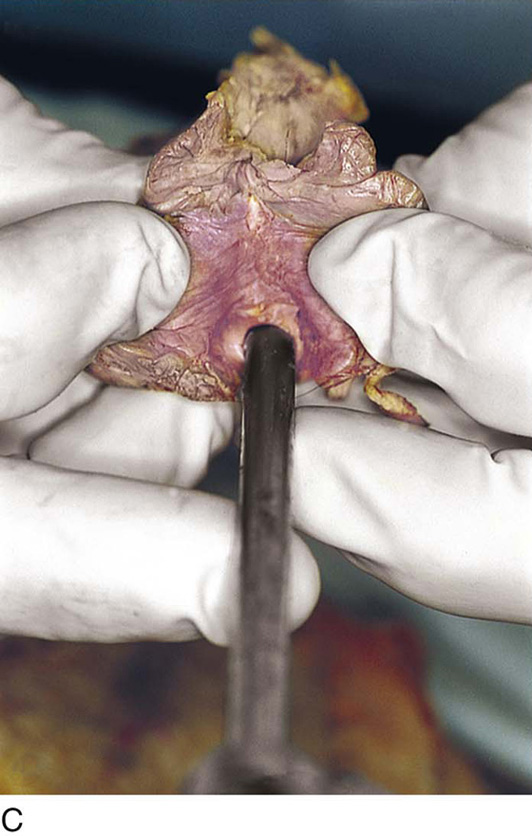
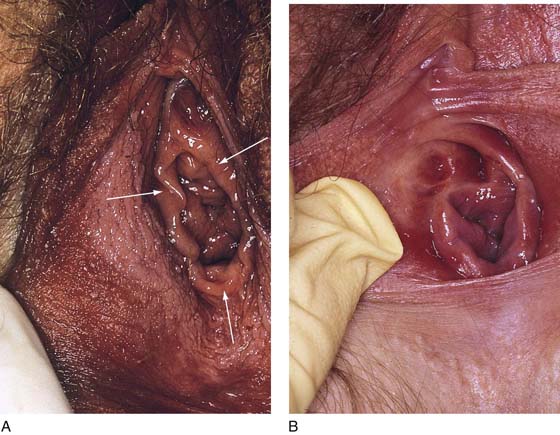
CHAPTER 51 The vagina is a potential space that connects the lower portion of the uterus (cervix) to the outside environment. The vagina measures 8 to 8.5 cm from the hymenal ring to the top of the anterior fornix; 7 to 7.5 cm to the top of the lateral fornix; and 9 to 9.5 cm to the top of the posterior fornix. For the sake of organization, the vagina may be divided into thirds: upper, middle, and lower. The upper third of the vagina is closely related to the cervix uteri, to which it is attached (Fig. 51–1). Throughout its length, the vagina is intimately applied to the bladder and urethra anteriorly and is similarly applied to the rectum posteriorly. In its lower third, the vagina, rectum, and urethra share common walls. The lower third of the vagina also is closely related to the vulva, to which it is attached at the level of the vulvar vestibule (Fig. 51–2A). This particular transitional area can be considered the entry portal to or the exit portal from the vagina. In fact, in the lower third, one might consider the urethra, vagina, and anus–rectum as a single interdependent and interrelated structure rather than as independently functioning anatomic units (Fig. 51–2B, C). By sawing away the symphysis pubis and dissecting the bladder and urethra from the anterior vagina, important relationships can be seen and better understood (Fig. 51–2D through F). The microscopic vagina consists of a mucosa that is made up of multilayered noncornified squamous epithelium. The underlying stroma consists of collagen admixed with elastic tissue. Beneath the stroma is smooth muscle interspersed with collagen. The epithelium measures 0.15 to 0.30 mm from top to bottom (surface to basement membrane). The entire vaginal wall thickness in a menstruating woman ranges from 2 to 3 mm. The hymenal ring forms the boundary between vagina and vestibule (Fig. 51–3A, B). Although the vagina contains no glandular elements under normal circumstances, several mucus-secreting structures are in close proximity: the paraurethral and vestibular glands (Fig. 51–4). The Bartholin glands (greater vestibular glands) are closely applied to the posterolateral wall of the vagina at a level 15 mm deep from the surface of the vestibule (Fig. 51–5A, B). At the 6-o’clock position, the rectum is 3 to 4 mm beneath the vagina, and at 12 o’clock, the urethra is 2 to 3 mm anterior to the vagina (Figs. 51–6A, B and 51–7A). The vagina is highly vascularized, particularly on the anterolateral and lateral walls, from the level of the hymenal ring to the urethrovesical junction (Fig. 51–7B). Large venous sinuses and cavernous sinuses account for this vascularity, which is most plentiful at the level of the bulb of the vestibule. The bulb is encountered at a depth of 1.5 cm from the surface of the vestibule and lies in close proximity to the urethra and the anterolateral wall of the vagina. The urethra is covered on its anterior and lateral aspects with cavernous tissue emanating from the clitoris and the bulb (Fig. 51–8A through G). When one is dissecting in this area, consideration should be given to the pronounced vascularity along the lateral and anterolateral walls and the need for vasoconstrictive agents. The middle third begins just below the urethrovesical junction and crosses beneath the lower margin of the symphysis pubis (posterior-inferior margin) (2.5 to 3.5 cm from the hymenal ring). The levator ani muscle is applied to the lateral and posterior vaginal walls most prominently at the junction of the middle and lower thirds (see Fig. 51–7C). This portion, together with the cranial portion of the lower third, has the greatest degree of mobility compared with the rest of the vagina. The upper vagina is closely applied to the bladder but does not share the common wall encountered at the level of the urethra. A layer of loose areolar tissue permits the bladder to be easily dissected from the upper vagina (see Figs. 51–2D through F). Similarly, the rectum can be easily dissected from the upper vagina. However, as one dissects caudally, the wall shared among bladder, urethra, and vagina allows no easy plane of separation. The vagina terminates around the cervix, and the vaginal vault is divided into fornices by the protruding portio vaginalis of the cervix. The stroma of the vagina is actually inseparable from the cardinal and uterosacral ligaments (see Fig. 51–7D). Between the latter is a bloodless entry point between the posterior fornix of the vagina and the cul-de-sac (i.e., the entry into the peritoneal cavity). The relationships of the upper vagina to the bladder, urethra, and cervix require precise anatomic knowledge of the retroischial and retropubic (extraperitoneal) spaces. Many gynecologists refer to the lateral areas as paravaginal, but in reality these areas constitute the perivesical spaces in their entirety. The anterior boundary of the retropubic space is the symphysis pubis and the pubic bone. The posterior boundary is the main body of the urinary bladder. The perivesical spaces extend on either side of the bladder and end above at the pubic bone and the obturator internus muscle, and below at the obturator internus muscle and the ischial bone. The levator ani muscle originates from the lower margin of the inferior pubic ramus and the fascia of the obturator internus and funnels downward to the junction of the middle one third and the lower one third of the vagina and into the perineal and perianal areas. The anatomy can be demonstrated only by sawing away a portion of the pubic bone (Fig. 51–9A through D). FIGURE 51–1 The upper third of the vagina is closely related to the uterus, particularly the cervix uteri. The rugous vaginal mucosa can be seen to merge with the smooth cervical mucosa on the far periphery of the portio vaginalis of the cervix. The central cervix creates the vaginal fornices at the vault. FIGURE 51–2 A. The lower third of the vagina forms a unit with the labia minora, vestibule, urethra, and rectum. The urethra is incorporated into the anterior vaginal wall. The anterior and posterior walls are in apposition. B. Compared with the lower vagina, seen in Figure 51–2A, this woman’s vagina is agape with a definite space visible between the anterior and posterior walls. Note the size and shape of the enlarged external urethral meatus. C. The bladder, the urethra, and a portion of the vestibule have been dissected free of the anterior wall of the vagina and have been removed. A metal cannula traverses the urethra into the bladder. D. The pubic bone has been cut away with a saw (large arrow). The previously excised bladder (B) and urethra (U) (see Fig. 51–2C) have been replaced in the pelvis. The bladder covers the retroverted uterus, and the sigmoid colon (C) covers the uterus, which lies in the cul-de-sac. The small arrow points to the right ureter. E. The bladder-urethra complex has been removed, exposing the anterior (outside) wall of the vagina (V). The surgeon’s finger is in the partially incised vagina and is located in the right lateral fornix (arrow). The scissors are directly lateral to the ureter. F. Detail of Figure 51–2E. The tip of the scissors is pointing to the pubocervical fascia of the vaginal wall. The blades of the scissors lie on that fascia and over the anterior vaginal fornix (F). Note the two sawed edges of the pubic bone overlying the surgeon’s gloved hand. FIGURE 51–3 A. The hymenal ring (arrows) separates the vagina from the vestibule. B.
Anatomy of the Vagina
Lower Third
Middle Third
Upper Third
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Mickey M. Karram
Mickey M. Karram