Fig. 1.1
Embryology of abdominal wall musculature
Anatomy
The first layer encountered just deep to the skin and subcutaneous tissues of the anterior abdominal wall is a fascial plane consisting of two layers: a fatty superficial layer which is called Camper’s Fascia and a deeper membranous layer, Scarpa’s Fascia. Scarpa’s Fascia runs inferiorly to attach to the thigh laterally and fuses medially with the perineal membrane as the inferior border of the superficial perineal pouch through which the urethra passes.
Deep to the superficial fascia lies the anterolateral muscles, which run in three separate directions, creating a strong latticework of muscle fibers. The most superficial of these muscle groups is the external oblique muscle, which runs caudal and medially from the lower eight ribs to the pelvis. The inferior border of the external oblique forms the inguinal ligament. A defect in the inguinal ligament, the superficial inguinal ring, affords passage of the round ligament from the abdomen to the pelvis. Deep to the external oblique, the internal oblique muscle fibers run cranially and laterally from the lower six costal cartilages to the pelvis, where they fuse with the muscle layer deep to it, the transversus abdominus, forming the conjoint tendon.
Medially, the rectus abdominus muscle originates at the pubic bone and runs superiorly to insert in the fifth, sixth, and seventh costal cartilages and the xiphoid process. It is encircled by the rectus sheath, which varies in composition depending on its location. Superiorly, the internal oblique splits to cover the rectus muscle both anteriorly and posteriorly. These layers are reinforced by the external oblique anteriorly and the internal oblique posteriorly. Caudally, all three anterolateral muscle groups pass anteriorly to the rectus. Above the coastal margin, the external oblique covers the rectus along its costal cartilage insertion. Together, these muscle fibers provide support for the abdominal organs. The ability to contract these muscles results in a rise in intraabdominal pressure, which aids processes of micturition and defecation.
Blood Supply
Running along the posterior aspect of the rectus sheath, the superior epigastric artery comes off of the internal mammary artery and anastomoses with the last five intercostal arteries above, and the inferior epigastric artery below. It supplies the upper abdominal wall. The inferior epigastric artery, a branch of the external iliac artery, comes through the abdominal inguinal ring, where it courses medially toward the superficial inguinal ring between the transversalis fascia and the peritoneum. This vessel passes through the transversalis fascia into the rectus muscle and meets the superior epigastric artery. The inferior epigastric artery supplies the lower abdominal wall.
Branches of the external iliac artery, mostly by way of the deep circumflex iliac artery, supply the lower abdominal wall. Traveling along the anterior superior iliac spine between the transversus and the internal oblique muscles, it anastomoses with the iliolumbar artery. The deep circumflex iliac artery also anastomoses with the inferior epigastric artery.
Nerves
The lower six thoracic nerves run between the internal oblique and the transversus muscles, penetrare the rectus sheath and muscle, and end as cutaneous branches. The 12th thoracic and first lumbar nerves join to form the iliohypogastric nerve, supplying the psoas and the quadratus lumborum before veering anteriorly to supply the transversus and the internal oblique muscles. The ilioinguinal nerve also comes off of the last thoracic and first lumbar nerve and communicates with the iliohypogastric nerve. The iliohypogastric nerve divides into the iliac branch, which supplies the lower internal and external oblique muscles above the iliac crest, and the hypogastric branch, which supplies the inferior portions of the transversus and the internal oblique muscles, the external oblique aponeurosis, the skin, and the symphysis pubis. This nerve then meets the ilioinguinal nerve near the anterior superior iliac spine.
Bony Pelvis
Embryology
The embryologic development of the bony and muscular pelvis is similar to that of the abdominal wall musculature. During the third week of gestation, the bilaminar embryonic disc transforms into the trilaminar embryonic disc, composed of ectoderm, mesoderm, and endoderm. A thickening of cells forms at the caudal region (primitive streak) and migrates cephalad, creating a depression on the ventral aspect of the trilaminar disc. This area of cells is called the embryonic mesoderm. Three clusters of mesodermal cells form by the end of the third week of gestation. They are the paraxial mesoderm, the lateral plate mesoderm, and the intermediate mesoderm. The paraxial mesoderm gives rise to the axial skeleton. The lateral plate mesoderm becomes the lateral and ventral body wall as well as the gut. The intermediate mesoderm will evolve into the urogenital ridge, and ultimately the reproductive and urinary tracts.
Anatomy
The pelvis can be separated into two compartments separated by the iliopectineal line: the greater (false) pelvis and the lesser (true) pelvis (Fig. 1.2). The iliac fossa and the sacrum form the boundaries of the greater pelvis, which houses the sigmoid colon and segments of the small intestine. The lesser pelvis lies below the pelvic brim and contains the pelvic organs, including the bladder, reproductive organs, the rectum, and the anus. It is bordered by the sacrum and coccyx posteriorly, the pubic symphysis anteriorly, and the obturator internus laterally. The pelvic brim demarcates the roof of the lesser pelvis while the pelvic musculature constitutes its floor.
Fig. 1.2
The bony pelvis, divided into two compartments divided by the iliopectineal line: the greater (false) pelvis and the lesser (true) pelvis
The bony pelvis is composed of three bones: the ilium, the ischium, and the pubis (Fig. 1.3). The amalgam of these three bones is called the innominate bone. The ilium sits posteriorly, and articulates with the acetabulum, the ischium, and the pubis. The superior border of the ilium is called the crest, extending inferiorly, ending at the iliac spines. The components of the ischium include the body, the superior and inferior rami, and the tuberosity. The posterior border joins with the ilium to form the greater sciatic notch. The inferior ramus meets the pubis to form the ischiopubic arch. The pubis is made up of a body and two rami. The obturator sulcus is located inferior to the superior ramus. The symphysis is a synarthrodial joint within the pubic bone.
Fig. 1.3
The bony pelvis is composed of three bones: the ilium, the ischium, and the pubis
The muscular attachments (Fig. 1.4a, b) to the ilum, ischium, and pubis create the bowl of the pelvic floor. The external oblique, the internal oblique, the transversus abdominus, latissimus dorsi, quadratus lumborum, tensor fascia latae, and Sartorius muscles all attach to the ilium. The rectus femoris muscle connects to the iliac spine. The iliacus muscle sits in the iliac fossa, and the tendon of the psoas inserts between the iliac spine and the iliopectineal eminence. Both the gluteus maximus and minimus muscles attach to the ilium.
Fig. 1.4
The muscular attachments to the bony pelvis
The ischium gives rise to the obturator internus muscle. The coccygeus and levator ani muscles attach to the ischial spines deep in the pelvis. The transversus perinei muscle originates from the lower border of the ischium. Laterally, the adductor magnus muscle connects to the ischial tuberosity. The obturator externus muscles and adductor longus muscles come off of the superior ramus of the pubis, while the obturator internus muscles and levator attach on the anterior surface. The rectus and pyrimidalis muscles attach on the superior border. The anterior surface of the inferior ramus attaches to the abductor brevis, magnus, and the obturator internus. See Fig. 1.5a, b.
Fig. 1.5
The muscularture of the bony pelvis, with an abdominal view
The sacrum is formed by the fusion of 5–6 sacral vertebrae. The body of the sacrum articulates with the fifth lumbar vertebrae through a fibrocartilage disk, where it juts out anteriorly and is labeled the sacral promontory. The lamina and spines of the third, fourth, and fifth sacral vertebrae are absent, leaving a wide space called the sacral hiatus. The coccyx is formed by 3–5 caudal vertebrae that fuse and join the sacrum at the sacrococcygeal joint. Muscular attachments to the sacrum include the piriform muscle, sacrospinalis muscles, and the gluteus maximus muscle. Muscles that connect to the coccyx include the coccygeus and the iliococcygeus musles.
The sacrospinalis ligament connects the lateral border of the sacrum and the coccyx to the ischial spine. The sacrotuberous ligament extends from the sacral vertebrae to the tuberosities of the ilium. This is a deep posterior ligament with fibers that connect to the hamstrings. The iliolumbar ligament joins the iliac crest with L4-5. The iliofemoral ligament attaches the crest of the ilium to the acetabulum. See Fig. 1.6.
Fig. 1.6
The ligaments of the bony pelvis
Blood Supply
The blood supply to the innominate bones comes from branches off of the iliolumbar, deep circumflex iliac, and obturator arteries, which all come off of the hypogastric (internal iliac) artery. The lower part of the bone receives nutrients from branches of the gluteal arteries, which also comes off of the hypogastric artery.
The sacrum receives its blood supply from the middle sacral artery, a branch of the aorta, and the lateral sacral arteries, which comes off of the hypogastric artery (internal iliac). These vessels anastomose with the lumbar arteries and the superior gluteal artery.
Nerve Supply
The innominate bones derive their nerve supply from the superior hypogastric plexus, which sits over the sacral promontory. It receives nerve fibers from inferior mesenteric and lumbar sympathetic ganglia. The superior hypogastric plexus gives rise to the middle hypogastric plexus and then divides into two lateral hypogastric nerves. They travel in the uterosacral ligament into the rectum and the vagina. At this juncture, they are labeled the pelvic plexuses. The fibers that make up the pelvic plexuses come from the S2-4 parasympathetic and sympathetic trunks. As the nerves descend into the pelvis, they innervate the bones and ligaments through which they pass.
Pelvic Muscles
Embryology (Fig. 1.7a, b)
The pelvic diaphragm arises out of all three layers of the embryonic tissue: the endoderm, the mesoderm, and the ectoderm. The endoderm develops into the primitive gut, which gives rise to the cloaca. At week 6 of gestation, the cloaca divides into the urogenital sinus and the anorectal canal. The mesoderm gives rise to the urogenital ridge, which becomes the urinary tract, the uterus and upper vagina, and the lateral plate mesoderm. The lateral plate mesoderm divides into the somatic and splanchnic mesoderm. The somatic mesoderm gives rise to the lateral and ventral walls, and the splanchnic mesoderm evolves into the visceral peritoneum. The ectoderm gives rise to the skin of the external genitalia and the nervous system.
Fig. 1.7
(a) Embryology of the pelvis muscles. (b) Embryology of the pelvic floor musculature
Anatomy
Pelvic Floor Musculature
In addition to providing support to the pelvic and abdominal organs and ensuring that they stay in their proper anatomical locations, the pelvic floor apparatus aids in the evacuation of both urine and feces. Additionally, the female pelvic floor has a central role in the acts of conception and parturition.
The pelvic floor is comprised of two main components; a visceral fascial layer, the endo-pelvic fascia (comprised of connective tissue), and a muscular layer, collectively referred to as the levator ani and coccygeus muscles. The endo-pelvic fascia provides a passive support mechanism when the genital hiatus is open, and provides an apical tethering point for the pelvic viscera. Conversely, the musculature provides an active support mechanism by contracting and closing the genital hiatus.
The pelvic diaphragm refers to the bowl of muscle that provides a supportive plate on which the bladder, uterus, and rectum sit. Perforated by the urethra, the vagina, and the rectum, these muscles serve as the support structures of the pelvic floor. The bony supports include the pubic bone anteriorly, the sacrum posteriorly, and the ischium bilaterally. The three main muscle groups that comprise the pelvic support include the levator ani, anteriorly and inferiorly, the obturator muscles laterally, and the coccygeus muscle, posteriorly.
Divided into three parts, the levator ani muscle is comprised of the Iliococcygeus muscle, the pubococcygeus muscle, and the puborectalis muscle. The iliococcygeus muscle arises laterally from the arcus tendineus it extends from the symphysis to the ischial spine, where it meets the obturator internus muscle. Medially it meets the pubococcygeus, and posteriorly, it inserts into the coccyx. The pubococcygeus is a strap of muscle that runs anterior to posterior from the pubis to the coccyx where it meets the sacrococcygeal ligament, forming a strong raphe over the sacrum. The puborectalis muscle creates a band of tissue around the rectum, which supports the posterior pelvis. The levator ani muscles function to both contract around the urethra, vagina, and rectum, and to counteract intraabdominal and intrathoracic pressures on the pelvic organs. See Fig. 1.8.
Fig. 1.8
Pelvic muscles groups and their attachments
Arising from the pubic rami and the ischium, the obturator internus muscle connects the pelvis to the hip, where its fibers insert into the trochanter. The obturator vessels and nerves traverse the notch on the lateral aspect of the obturator foramen. Intrinsic to the functioning of the inner thigh, the obturator muscle is involved in lateral rotation, abduction, and extension of the upper leg.
Not comprising many muscle fibers, the coccygeus appears more as an aponeurosis than as a muscle. It arises from the ischial spine and extends into the fourth and fifth sacral vertebrae, as well as the coccyx. Besides supporting the pelvic organs, it helps with flexing and abducting of the coccyx.
Perineum and Structures from Below
From the perineal perspective, the fascial supports overlying the organs play a crucial role in both the pathophysiology of pelvic organ prolapse and the methods of repairing those defects. An extension of the transversus abdominus muscle, the endopelvic fascia lays over the abdominal portion of the pelvic musculature. The levator ani muscles are covered from the perineal side by the same facial material but it is divided into three sections depending on what structures are being covered.
From the vaginal view, looking at the anterior vaginal wall, the urethropelvic (also called the pubourethral) ligament creates a bridge extending from the inferior aspect of the pubic ramis from side to side, thus supporting the urethra. If there were any weakness or damage to this fascial layer, stress incontinence would be the end result. The pubocervical fascia (sometimes called the vesicocervical fascia) is the component of the sheet of support under the bladder. It is not discrete and cannot be visually separated from the urethropelvic ligament, except by determining the organ under which it sits. This fascial layer can be torn, causing a central defect, which results in a cystocele. Correcting central defects in the pubocervical fascia requires replacing that fascia support from below. See Fig. 1.9.
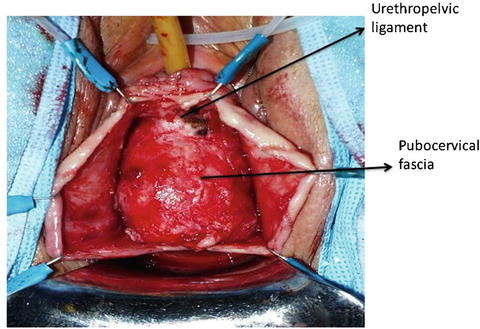
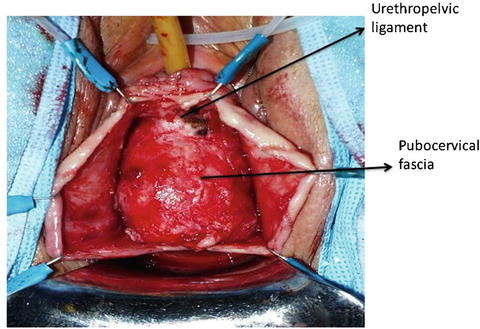
Fig. 1.9
Fascial layers of the pelvic organs: vaginal view
The urethropelvic fascia and the pubocervical fascia insert into the pelvic sidewall where the levator ani muscles meet the obturator internus. From the view looking into the pelvis from above, the endopelvic fascia can be seen inserting into the same place. This condensation of both fascial layers into the same insertion point is called the arcus tendineus. An important support for the pelvic organs, the arcus tendineus can be damaged in surgery, pregnancy, or childbirth, resulting in the pelvic organs sliding down the sidewall and causing a prolapse. See Fig. 1.10.
Fig. 1.10
Ligaments of vaginal support
The posterior section of the support under the anterior vaginal wall is the cardinal ligament, which supports the uterus and the apex of the vagina. The cardinal ligament extends from the sciatic foramen, encircles the cervix, and fuses with the sacrouterine ligament posteriorly. The sacrouterine ligament is a non-discrete condensation of fibers that originates from the second through fourth sacral vertebrae and merges with the pubocervical fascia at the vaginal apex. If the fibers of the sacrouterine ligament are intact, they can be used to support a prolapse repair. Deep to the sacrouterine ligament is the sacrospinous ligament, which runs from the sacrum to the ischial spine. It is a strong, fibrous true ligament, in that it joins two bony structures.
The posterior vaginal wall support structures include the rectovaginal septum, the pararectal fascia, and the perineal body. At the apex of the vaginal, the rectovaginal septum fuses with the cardinal ligament/sacrouterine ligament complex. Disruption of the cardinal ligaments through surgery, pregnancy, or childbirth can lead to weakness of the septum and posterior apical prolapse. The perineal body is a central point where the deep and superficial transverse perineal muscles, the anal sphincter, the bulbocavernosus muscle, and the levator ani muscles all converge. Flexibility of the perineal body allows for absorption of pressure during valsalva, and contraction increases both vaginal compression and stability. See Fig. 1.11.