Fig. 1
Multiple digit amputation caused by a young child placing fingers in a paper shredder. A severe crushing and avulsive mechanism of this sort may make replantation impossible (Courtesy of Joshua Ratner, MD)
Obtaining an accurate history of the injury mechanism also provides the surgeon with information that may affect surgical treatment. Compartment syndrome should be considered following crushing injuries to the hand or forearm, and replantation should be accompanied by appropriate emergent fasciotomies. In the case of severe contamination, such as in farm injuries, more aggressive debridement should be planned, and broad-spectrum antibiotics, including penicillin for clostridium coverage, should be started immediately. Avulsion-type injuries are often indicative of a larger zone of injury than is readily apparent. This injury mechanism can involve disruption of the more proximal musculotendinous junction and inflict long segment vascular injury requiring a vein graft for successful replantation (Buncke et al. 2003).
As with any trauma, the “ABCs” (airway, breathing, circulation) should be addressed first and only then should the focus be on the amputated part. Partington et al. showed that in a 7-year period, with a total of 1,100 patients that were referred for emergency microvascular surgery, there was a 1 % incidence of occult injuries that ultimately changed the original plan of care (Partington et al. 1993). The pediatric patient, unlike an adult, may be unable to provide a reliable history, and therefore witnesses (parents or ambulance crew) become extremely important in understanding the extent and timing of trauma. Amputations of the hand are self-evident, but it is also important to determine the level of injury to suggest associated more proximal injuries. Determining the time of injury and the field management of the amputated part should provide the surgeon with the assessment of the cold and warm ischemia insult sustained by the amputated part and the urgency of reperfusion. Digit replantation is considered feasible if warm ischemia time is limited to 6–12 h. Due to the lack of ischemia-sensitive muscle, a well-preserved and cooled digit, cold ischemia can likely be tolerated for up to 24 h after amputation prior to replantation (Lin et al. 2010; Waikakul et al. 2000). Cases of delayed digit replantation have reported even after 33 h and 94 h of warm and cold ischemia, respectively (Chiu and Chen 1984; Wei et al. 1988). The limits of tolerated ischemia time in distal amputations are thus poorly defined. Indeed, Lin et al. studied ischemia time in 31 cases of hand and finger replantation that exceeded 24 h and found no correlation between ischemia time and postoperative outcome (Lin et al. 2010).
Fingertips amputated distal to the lunula in the pediatric population, typically age three or younger, can be replaced as a composite graft without a vascular anastomosis as their survivability, and outcomes have been reported as excellent (Shenaq and Kattash 1998). Heistein et al. evaluated factors affecting composite graft survival in fingertip amputations distal to the DIP joint. After performing a multivariate analysis, smoking was found to be the only significant risk factor for graft failure. Age older than 18 was initially thought to lead to higher failure rates, but later this was found to be closely linked to smoking. There was a trend for higher graft failure in crush injuries compared to avulsion or sharp amputations, but this did not reach statistical significance (Heistein and Cook 2003).
Innis provided a methodical description of the proper handling of amputated parts . The amputated part should be wrapped in clean moist gauze, placed in a bag, and sealed without any direct ice contact (Fig. 2). The bag with the part should then be placed in another container with ice. A bulky pressure dressing should be applied to the injured extremity to prevent hemorrhage, and the patient should either be transferred to the emergency department or a tertiary care institution (Innis 1995).


Fig. 2
Amputated part wrapped in moist sterile gauze. Subsequently, the part should be placed in a waterproof bag and then in a bucket of ice (Courtesy of Joshua M. Abzug, MD)
Bleeding vessels can be routinely controlled by application of pressure and appropriate bandages. Application of vessel clamps in the field or emergency department to control bleeding should be avoided if possible, so that inadvertent injury to the adjacent structure (i.e., nerves) can be avoided, and more extensive arterial injury prevented. Use of tourniquets in the field or during transport should be discouraged unless all attempts at pressure dressing hemostasis have been exhausted. The use of field tourniquets risks further nerve and muscle damage if field management is prolonged or performed by those unfamiliar with tourniquet technique. Parts that are nearly amputated but attached should be placed into near anatomical alignment and splinted. This will prevent further damage to the part that might occur from kinking of remaining vascular structures (Michalko and Bentz 2002).
Determining concomitant medical conditions enables the surgeon to ascertain the risk of lengthy or complex surgical interventions. If the patient has not received a tetanus vaccination, it should be provided in the emergency department. If rabies transmission is a risk from a rabid animal bite, one should start treatment immediately. The disease is usually fatal, and for this reason, the child should receive rabies immune globulin and then a series of five doses of rabies vaccine over the following 2 weeks.
Imaging
All hand injuries should be evaluated with three views of the hand (PA, oblique, and true lateral). Dedicated finger x-rays should be obtained for all digits that are injured. Two views of the extremity (AP and lateral) are needed if there is an injury to the forearm or upper arm. If the mechanism of injury is suspicious for a larger zone of injury, then the adjacent joints should also be imaged. The amputated part should be imaged to fully understand the pattern of injury, extent of bone loss, joint involvement, and comminution.
Radiographs of the pediatric hand are limited by the ossification progression of the bones. Understanding the normal ossification center anatomy is important to accurately interpret a pediatric hand radiograph. At birth, all carpal bones are cartilaginous and thus unable to be evaluated by radiographs. Ossification progresses in a predictable manner with the capitate and hamate ossifying within the first 3 months followed by the triquetrum and lunate within the first 2–4 years of life. By age 6, the trapezium, trapezoid, and scaphoid have also typically ossified, while the pisiform ossifies during puberty. The epiphyses of the metacarpals and phalanges become recognizable between 12 months and 3 years of life. The physis is located distally in all metacarpals except the thumb and proximally in all phalanges (Gilsanz and Ratib 2012). It is important to locate, protect, and prevent any further damage to the physis when planning a replantation surgery in children.
Replantation of the Injured Part
Indications
In 1995 Tan and Teoh published their experience from 8 children with 10 digits that were replanted from 1993 to 1994. They suggested that replantation was always indicated in children because of the possibility of obtaining good functional results in young patients. They described an 11-year-old boy with a complete avulsion amputation of the right ring finger who regained 100° flexion at the PIP joint and 10° at the DIP joint with his physis remaining open 5 months after replant. Another 8-year-old boy, 13 months after replantation of the left index finger following a sharp crush injury at the level of the DIP joint, had excellent function with 40° flexion of the joint (Tan and Teoh 1995). Cheng et al. published their series of 44 amputated digits that were replanted in children with long-term follow-up of 9–15 years (Cheng et al. 1998). While surgical success in replantation does not assure functional success, these studies support broadened indications for pediatric replantation due to the greater healing potential and adaptability in this population (Shenaq and Kattash 1998).
Dautel classified fingertip amputations and proposed several indications for replantation in children by addressing three categories: mechanism of injury, vascular anatomy, and level of amputation within the fingertip. Since the majority of pediatric amputations are caused by crush or avulsion injuries and sharp or clean-cut injures are rare, he felt that the mechanism of injury should have no influence on the decision to attempt replantation. He proposed that it is best to evaluate the part under the microscope in order to decide upon replantation or revision amputation. Microscope magnification and microvascular techniques have made replantation for even very distal amputations feasible. There is often an arterial branch that courses close to the midline within the pulp of the digit, and this branch can typically be anastomosed. Lastly, Dautel noted that each level of fingertip amputation poses technical challenges that differ according to the zone of amputation . He proposed four zones within the fingertip, all distal to the DIP joint:
Zone 1: No bone fragment; distal tip pulp with no vessels suitable for anastomosis. The part may be replaced as a composite graft.
Zone 2: Amputation through the nail bed, preserving at least one half of the sterile matrix. The part may contain an artery that courses close to the midline within the pulp and it can be used for anastomosis. In this zone, there are often no dorsal veins available; venous drainage can be controlled by either retrieving a palmar vein or controlled bleeding.
Zone 3: Similar to zone 2; however, the sterile matrix remaining on the digit is minimal or absent.
Contraindications
In children many authors have advocated attempting replantation of any digit amputation. However, relative contraindications are worthy of consideration. Boulas proposed the following contraindications:
Warm ischemia time more than 12 h for digits where muscle is absent and more than 6 h where muscle is present
Severely crushed parts or the mangled extremity where the majority of the tissue components are damaged
Extensive avulsion injuries which are associated with extensive damage to vessels, nerves, and musculotendinous elements
Multilevel or segmental amputation injury of the extremity
Severe major psychiatric disorders where the patient cannot comply with postoperative instructions
Prior nonfunctional or limiting functional conditions of the injured extremity
Damage to the part by inadequate transport care , such as when the part is placed directly on ice, causing freezing and formation of intracellular ice crystals, capillary damage with micro thrombosis, and irreversible vasoconstriction (Table 1).
Table 1
Operative Indications & Contraindications for Pediatric Replantation
Operative indications | Operative contraindications |
|---|---|
In general, pediatric digital amputations should undergo attempt at replantation | Other life-threatening injuries |
Severe contamination | |
Relative contraindications | |
Multilevel or mangled amputation | |
Extensive avulsion injury | |
Excessive warm ischemia time |
There are two strict contraindications that are proposed:
The extremely contaminated injury which could place the patient at risk for sepsis and/or necrotizing infection
Concomitant life-threatening injuries, where the priority should always be to preserve life and not limb (Boulas 1998)
Anesthesia
Most pediatric hand trauma cases, and especially those that will endeavor replantation, should be done under general anesthesia as they are particularly long procedures. An adjunct to general anesthesia is the use of regional blocks which can enhance vasodilatation via sympathetic blockade. The procedure has proven to be safe and effective in the pediatric population and in the acute setting (Ivani and Mossetti 2008).
Operative Techniques
The sequence of repair of various structures involved in replantation may vary according to a surgeon’s preference, but general principles may be observed. In general, skeletal shortening and fixation is performed first, with other macroscopic work, such as tendon repairs, prior to performing more delicate microsurgery. Surgeons may prefer alternative techniques. Kim et al. advocated first addressing skeletal fixation, then arterial repair, followed by venous repair, tendons, and lastly coaptation of nerves (Kim et al. 2005) (Table 2).
Table 2
Preoperative Planning for Pediatric Replantation
OR table: standard table with radiolucent hand table attachment |
Position: supine with arm on hand table |
Fluoroscopy location: same side as hand table |
Equipment/supplies: fluoroscopy, operating microscope, Doppler with sterile probe, microsurgical instruments, wire driver, Kirschner wires, 4–0 nonabsorbable suture, 6–0 monofilament, 10–0 nylon, warm saline, papaverine, heparinized saline irrigation with 24-gauge Angiocath, and arterial and venous microsurgical vessel clamp |
Tourniquet: nonsterile |
Addressing multiple digit amputations in children is technically challenging and time consuming. Some surgeons advocate attempting to replant all parts and restoring hand anatomy and function as close as possible to its original state (Kim et al. 2005). Others feel that the surgeon should try to replant enough digits to restore two main functions: pinch and grasp. These goals mandate that at the very minimum, a thumb and an opposing digit be replanted (Buncke et al. 1991; Bennett 1975). This decision depends on the condition of the amputated parts. In difficult situations, the surgeon may choose to borrow parts from a non-salvageable digit for use in reconstructing other digits. In cases of multiple digit replants, Kim et al. advocate a “structure-by-structure” replantation technique as opposed to the less time-efficient digit-by-digit scheme. In structure-by-structure replantation, skeletal fixation is achieved in all digits before subsequently addressing tendons, nerves, arteries, and veins in that sequence (Kim et al. 2005).
Amputations at the level of the hand or wrist tend to be avulsion- or crush-type injuries in the pediatric population. A thorough debridement of devitalized or contaminated tissue is important to prevent subsequent infection, but the surgeon should also attempt to preserve as much healthy tissue as possible for reconstruction. As with digital amputations, bony fixation of the involved metacarpals, carpals, and radius and ulna should be the first step of the replant procedure. This can be accomplished with Kirschner wires, intraosseous wiring, screws, or plates (Kim et al. 2005). As in adult replantation, bone loss or skeletal shortening may require partial or total wrist arthrodesis. However, particular effort is made in avoiding loss or damage of physes to preserve future limb growth.
For cases of forearm or upper arm amputation, it is critical that the part be placed in an ice saline solution for transport and that cold perfusion with heparinized saline be considered when the part arrives to the replant center (Tamai 1982). Additionally, due to the possibility of reperfusion compartment syndrome, patients should undergo fasciotomies with consideration given to serial operative wound assessment to discern the viability of the muscles and skin (Kim et al. 2005). The limb should be revascularized as soon as possible to prevent muscle death and minimize the risk of subsequent infection (Saies et al. 1994; Taras et al. 1991).
As in cases of adult major limb replantation, consideration may be given to intraoperative arterial shunting with specifically designed catheters. This enables rapid reestablishment of arterial supply to the part. This is considered if the presurgical ischemia time is lengthy and the amputated part contains significant amounts of ischemia-sensitive muscle. The shunt is typically placed prior to skeletal fixation and arterial flow is reestablished. The surgeon may elect to shunt a large vein and minimize blood loss during this procedure. Shunt reperfusion is maintained for adequate duration to enable the surgeon to safely begin tourniquet-controlled replantation thereafter. The surgeon may lengthen the shunt reperfusion period if the previous ischemia time was lengthy.
During reperfusion of forearm or arm level amputations, the anesthesiologist should carefully monitor the patient’s hematocrit and administer blood as needed (Buncke et al. 2003). Due to the reperfusion of ischemic muscle, the venous return at first is dark and high in potassium due to muscle breakdown. Waikakul et al. showed that the risk for failed replantation is higher if the measured potassium is greater than 6.5 meq/dL from the venous return (Waikakul et al. 1998).
If the required shunt reperfusion period is lengthy and the anatomy permits, the surgeon may proceed with osseous fixation , tendon repair, and nerve repair with the shunt in place. When the perfusion period is deemed adequate, the shunt may be removed and arterial repair or reconstruction with grafts is then pursued rapidly.
Skeletal Fixation and Bone Shortening
For digits, bone shortening is an important technique to minimize tension on the anastomosis of arteries, veins, and nerves ; however, in children, one must not compromise the physis (Urbaniak 1984). Popular stabilization techniques for digits include intraosseous wires or Kirschner wires (Fig. 3).
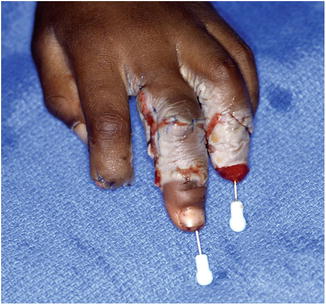
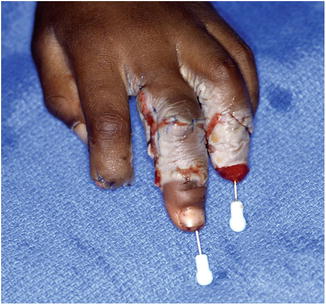
Fig. 3
Successful replantation of the long and ring fingers using longitudinal K-wires for fixation (Courtesy of Shriners Hospital for Children, Philadelphia, PA)
For fingertip amputations, Kirschner wires are often too large and should not be used in infants, toddlers, or young children. For these patients, small needles, such as a 25- or a 27-gauge, can be used for bone fixation . The needles may be inserted by hand, and not with a power drill. This minimizes the transfer of heat that is generated by the drill, which can lead to necrosis of the small bone fragment and thin surrounding tissues. In replantation performed at the distal fingertip, a single needle is sufficient, whereas more proximally two crossed needles will achieve fixation and prevent rotation (Dautel 2000; Dautel and Barbary 2007).
When the injury is at the wrist, forearm, or upper arm level, the radius, ulna, and humerus can be shortened up to 3 or 4 cm without significant functional problems. In long bones, rigid fixation with plates provides the best stability while again making sure not to injure the physis with shortening or fixation (Buncke et al. 2003).
Tendon Repair
Multiple tendon repair techniques have been described throughout the literature, and the technique employed is often dependent on surgeon preference and the zone of injury. Tendon repair within the flexor tendon sheath is performed with greater surgical precision to minimize adhesion formation. Increasing the number of strands across the repair site and the addition of an epitendinous stitch has been shown to improve the repair strength and tendon gliding within the sheath. Outside the flexor sheath, the tendons may be repaired with core sutures. Less precision needs to be dedicated to avoiding bulk of the repair site as it does not require passage through the sheath. Within flexor tendon zone 5, if the tendons are avulsed from the musculotendinous junction, primary tendon transfers should be considered (Kim et al. 2005). Buncke et al. preferred to repair the tendons with a double-opposing locking loop with or without an epitendinous stitch, although for extensor tendons, they recognized that if there is no length, a mattress repair is adequate (Buncke et al. 2003).
Arterial Repair
In the setting of a sharp laceration or penetrating injury, identification of vessel ends is often accomplished near the traumatic wound. However, following avulsion-type injuries, damage of a long vessel segment may frequently be encountered and require vein grafting for repair even after bone shortening (Michalko and Bentz 2002; Cheng et al. 1998).
For fingertip injuries, evaluation of the proximal stump and the distal part should be done under a microscope in order to identify possible vessels for anastomosis. If the distal vessel is collapsed, one can milk the fingertip pulp and refill the vessels for aid in identification. Exposure of the proximal vessels is performed with midaxial or volar zigzag incisions (Tsai et al. 1989). Vessels are repaired under the microscope with 9-0, 10-0, or 11-0 monofilament (Dautel 2000; Dautel and Barbary 2007).
Venous Repair
Identifying suitable dorsal veins for anastomosis is technically challenging. By starting with the arterial anastomosis, subsequent venous engorgement can aid in the identification of dorsal veins. If possible, at least two veins should be repaired with studies showing that this technique will reduce venous congestion and bleeding and improve replant survival (Michalko and Bentz 2002; Cheng et al. 1998; Kim et al. 2005). Hattori et al. published a case series of 64 finger replants, where venous anastomosis was possible 84 % of the time, and reported an overall survival rate of 86 %. They concluded that the most critical factor in survival of the replant was the venous anastomosis (Hattori et al. 2003). Venous repair in very distal fingertip amputations is difficult due to the lack of dorsal veins. Tsai et al. advocate performing a venous anastomosis using a volar vein within the pulp (Tsai et al. 1989). In the absence of identifiable volar or dorsal veins, fingertip replantation may require using postoperative controlled bleeding to maintain digit viability until small venous pathways are developed (Dautel 2000; Dautel and Barbary 2007).
Nerve Repair
An important aspect of the functional outcome of digital replantation is the recovery of sensation. Excellent recovery of sensation has been demonstrated in replantation of pediatric digits, further supporting attempted replantation of all pediatric amputations when feasible. For fingertip injuries, identification of neural elements and repair can be technically challenging and sometimes impossible. However, great sensory recovery can be expected even without a nerve repair. Dautel evaluated recovery of sensation in eight pediatric patients with fingertip replantations where fingertip level nerve repair was not performed. Good return of sensation was found in this group despite the lack of nerve repair with an average 2-point discrimination of 4.6 mm at final follow-up (Dautel 2000; Dautel and Barbary 2007). Faivre et al. also found that there is adjacent and spontaneous neurotization after replantation of fingertips distal to the DIP joint in children (Faivre et al. 2003).
For more proximal injuries, primary nerve coaptation should be performed using an 8-0 or 9-0 microsuture. If excessive tension or a gap exists, nerve grafting should be performed. Typical sites of donor nerves are the posterior interosseous nerve, medial antebrachial cutaneous nerve, or digital nerve from adjacent non-salvageable digits (Kim et al. 2005). Other microsurgeons have successfully utilized the lateral femoral cutaneous nerve, superficial peroneal nerve from the dorsum of the foot, and the sural nerve for nerve grafts (Faivre et al. 2003; Buntic et al. 2002). While autograft remains the gold standard for nerve reconstruction, nerve conduits and nerve allograft have proven effective for reconstructing peripheral digital nerve deficits up to 30 mm while avoiding donor site morbidity (Taras et al. 2013; Lohmeyer et al. 2013) (Table 3).
Table 3
Surgical Steps for Pediatric Replantation
Begin preparation of amputated part prior to induction of anesthesia |
Identify amputated part neurovascular structures via bilateral midaxial approach |
Perform osseous shortening of amputated part preserving physis |
Place Kirschner wires in amputated bone perched at osteosynthesis site |
Place locking core suture in FDP tendon of amputated part |
Remove nail |
Identify proximal neurovascular structures via bilateral midaxial approach |
Fixate amputated bony structures to proximal bone with Kirschner wires |
Perform a 4-strand core suture repair of the FDP tendon only |
Repair extensor tendon with a figure-of-eight stitch |
Repair nerve using operating microscope |
Repair at least 2 dorsal veins using operating microscope if tourniquet time allows
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|