Chapter 24
Alternative Regional Analgesic Techniques for Labor and Vaginal Delivery
David H. Chestnut MD
Neuraxial analgesic techniques are the most flexible analgesic techniques available for obstetric patients. The anesthesia provider may use an epidural or a spinal technique to provide effective analgesia during the first and/or second stage of labor. Subsequently, the epidural or spinal technique may be used to achieve anesthesia for either vaginal or cesarean delivery. Unfortunately, some maternal conditions (e.g., coagulopathy, hemorrhage) contraindicate the administration of neuraxial analgesia. Many parturients do not have access to neuraxial analgesia, and others do not want it. The purpose of this chapter is to discuss alternative regional analgesic techniques for labor and vaginal delivery.
Paracervical Block
During the first stage of labor, pain results primarily from dilation of the cervix and distention of the lower uterine segment and upper vagina. Pain impulses are transmitted from the upper vagina, cervix, and lower uterine segment by visceral afferent nerve fibers that join the sympathetic chain at L2 to L3 and enter the spinal cord at T10 to L1. Some obstetricians perform paracervical block to provide analgesia during the first stage of labor. The goal is to block transmission through the paracervical ganglion—also known as Frankenhäuser’s ganglion—which lies immediately lateral and posterior to the cervicouterine junction.
Paracervical block does not adversely affect the progress of labor. Further, it provides analgesia without the annoying sensory and motor blockade that may result from neuraxial analgesia. The paracervical technique does not block somatic sensory fibers from the lower vagina, vulva, and perineum. Thus, it does not relieve the pain caused by distention of these structures during the late first stage and second stage of labor. Contemporary experience suggests that paracervical block results in satisfactory analgesia during the first stage of labor in 50% to 75% of parturients. One study noted that paracervical block provided better analgesia in nulliparous women than in parous women, probably because paracervical block does not provide effective analgesia for the sudden and rapid descent of the presenting part that often occurs in parous women.1
In 1981, approximately 5% of laboring women in the United States received paracervical block,2 and 2% to 3% of parturients in the United States received paracervical block during labor in 2001.3 Paracervical block remains more popular in Scandinavian countries. Approximately 17% of Finnish parturients received paracervical block during labor in 2004-2005.4 In the United States, the decline in the popularity of paracervical block has resulted from both fear of fetal complications and the greater popularity of neuraxial analgesic techniques.
Jensen et al.5 randomly assigned 117 nulliparous women to receive either bupivacaine paracervical block or intramuscular meperidine 75 mg. Women in the paracervical block group had significantly better analgesia than women in the meperidine group at 20, 40, and 60 minutes. During the first 60 minutes, pain relief was complete or acceptable in 78% of the women in the paracervical block group but in only 31% of the women in the meperidine group. Two fetuses in the paracervical block group and one in the meperidine group had transient bradycardia. A total of 6 infants in the paracervical block group and 16 infants in the meperidine group (P < .05) had fetal/neonatal depression, which the investigators defined as an umbilical arterial blood pH of 7.15 or less and/or a 1-minute Apgar score of 7 or less.5 A 2012 Cochrane Review cited this study as evidence that paracervical block provides more effective analgesia during labor than intramuscular meperidine.6
In a recent study, Junttila et al.4 randomly assigned 122 parous women to receive either bupivacaine paracervical block or single-shot spinal bupivacaine with sufentanil. Single-injection spinal analgesia was superior to that provided by paracervical block (Figure 24-1), although paracervical block resulted in a pain score of 3 or less in 43% of the study subjects, and over half of the women in the paracervical block group indicated that they would be happy to receive this method of analgesia during labor in a future pregnancy. There was no difference between the two groups in the incidence of fetal heart rate (FHR) abnormalities, and there were no cases of fetal bradycardia in either group.4
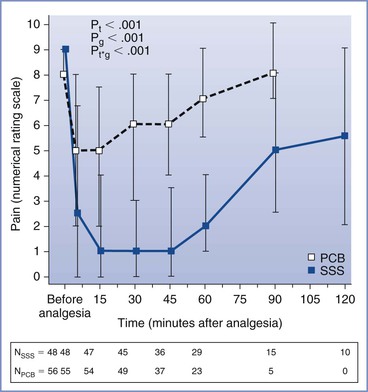
FIGURE 24-1 Pain scores over time before and after paracervical block (10 mL of 0.25% bupivacaine) or single-shot spinal (intrathecal) injection of bupivacaine 2.5 mg and sufentanil 2.5 µg. Data are median pain scores with the 25th and 75th percentiles. PCB, paracervical block; SSS, single-shot spinal analgesia; Pt, P-time; Pg, P-groups; Pt*g, P-time*group. N, number of parturients at the measurement time points. (From Junttilla EK, Karjalainen PK, Ohtonen PP, et al. A comparison of paracervical block with single-shot spinal for labour analgesia in multiparous women: a randomized controlled trial. Int J Obstet Anesth 2009; 18:15-21.)
Kangas-Saarela et al.7 compared neonatal neurobehavioral responses in 10 infants whose mothers received bupivacaine paracervical block with those in 12 infants whose mothers received no analgesia. The investigators performed paracervical block while each patient lay in a left lateral position, and they limited the depth of the injection into the vaginal mucosa to 3 mm or less. They observed no significant differences between groups in neurobehavioral responses at 3 hours, 1 day, 2 days, or 4 to 5 days after delivery. These investigators concluded that properly performed paracervical block does not adversely affect newborn infant behavior or neurologic function.7
Technique
Paracervical block is performed with the patient in a modified lithotomy position. The uterus should be displaced leftward during performance of the block; this displacement may be accomplished by placing a folded pillow beneath the patient’s right buttock. The physician uses a needle guide to define and limit the depth of the injection and to reduce the risk for vaginal or fetal injury. The physician introduces the needle and needle guide into the vagina with the left hand for the left side of the pelvis and with the right hand for the right side (Figure 24-2). The needle and needle guide are introduced into the left or right lateral vaginal fornix, near the cervix, at the 4-o’clock or the 8-o’clock position. The needle is advanced through the vaginal mucosa to a depth of 2 to 3 mm.8 The physician should aspirate before each injection of local anesthetic. A total of 5 to 10 mL of local anesthetic, without epinephrine, is injected on each side.9 Some obstetricians recommend giving incremental doses of local anesthetic on each side (e.g., 2.5 to 5 mL of local anesthetic between the 3-o’clock and 4-o’clock positions, followed by 2.5 to 5 mL between the 4-o’clock and 5-o’clock positions).8,10,11
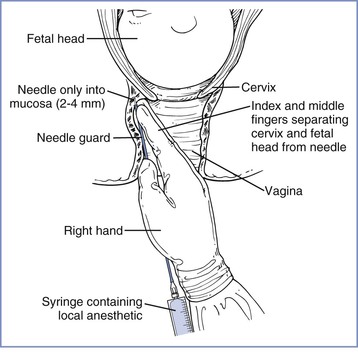
FIGURE 24-2 Technique of paracervical block. Notice the position of the hand and fingers in relation to the cervix and fetal head. No undue pressure is applied at the vaginal fornix by the fingers or the needle guide, and the needle is inserted to a shallow depth. (Redrawn from Abouleish E. Pain Control in Obstetrics. New York, JB Lippincott, 1977:344.)
After injecting the local anesthetic in either the left or right lateral vaginal fornix, the physician should wait 5 to 10 minutes and observe the FHR before injecting the local anesthetic on the other side.11 Some obstetricians do not endorse this recommendation. Van Dorsten et al.12 randomly assigned 42 healthy parturients at term to either of two methods of paracervical block. The study group experienced a 10-minute interval between injections of local anesthetic on the left and right sides of the vagina. The control group had almost simultaneous injections on the left and right sides. No cases of fetal bradycardia occurred in either group. The investigators concluded that patient selection and lateral positioning after the block have a more important role in the prevention of post–paracervical block fetal bradycardia than spacing the injections of local anesthetic. However, because they studied only 42 patients and had no cases of fetal bradycardia in either group, they could not exclude the possibility that incremental injection might reduce the incidence of fetal bradycardia in a larger series of patients.
Choice of Local Anesthetic
The physician should administer small volumes of a dilute solution of local anesthetic. There is no reason to inject more than 10 mL of local anesthetic on each side. Further, there is no indication for the use of concentrated solutions, such as 2% lidocaine, 0.5% bupivacaine, or 3% 2-chloroprocaine. Nieminen and Puolakka13 observed that paracervical block with 10 mL of 0.125% bupivacaine (5 mL on each side) provided analgesia similar to that provided by 10 mL of 0.25% bupivacaine.
The choice of local anesthetic is controversial. The North American manufacturers of bupivacaine have stated that bupivacaine is contraindicated for the performance of paracervical block. In contrast, many European obstetricians—especially those in Finland—have expressed a preference for bupivacaine for this procedure. Bupivacaine has greater cardiotoxicity than other local anesthetic agents, and some investigators have suggested that its use leads to a higher incidence of fetal bradycardia or adverse outcome than use of other local anesthetics for paracervical block. In a review of 50 cases of perinatal death associated with paracervical block, Teramo14 found that the local anesthetic was bupivacaine in at least 29 of the 50 cases.
Palomäki et al.15 hypothesized that levobupivacaine might result in a lower incidence of post–paracervical block fetal bradycardia than racemic bupivacaine. In a randomized double-blind study of 397 laboring women, paracervical block was performed with 10 mL of either 0.25% levobupivacaine or 0.25% racemic bupivacaine. The incidence of transient FHR abnormalities was 10.4% in the levobupivacaine group and 12.8% in the racemic bupivacaine group, and that of fetal bradycardia was 2.6% in the levobupivacaine group and 3.8% in the racemic bupivacaine group (P = NS).
Some physicians have suggested that 2-chloroprocaine is the local anesthetic of choice for paracervical block. Published studies suggest but do not prove that post–paracervical block fetal bradycardia occurs less frequently with 2-chloroprocaine than with amide local anesthetics.10,16–18 Weiss et al.16 performed a double-blind study in which 60 patients were randomly assigned to receive 20 mL of either 2% 2-chloroprocaine or 1% lidocaine for paracervical block. Bradycardia occurred in 1 of the 29 fetuses in the 2-chloroprocaine group, compared with 5 of 31 fetuses in the lidocaine group (P = .14). LeFevre18 retrospectively observed that fetal bradycardia occurred after 2 (6%) of 33 paracervical blocks performed with 2-chloroprocaine versus 44 (12%) of 361 paracervical blocks performed with mepivacaine (P = .29).
2-Chloroprocaine undergoes rapid enzymatic hydrolysis. Thus it has the shortest intravascular half-life among the local anesthetics used clinically. This rapid metabolism seems advantageous in the event of unintentional intravascular or fetal injection. Philipson et al.17 performed paracervical block with 10 mL of 1% 2-chloroprocaine in 16 healthy parturients. At delivery, only trace concentrations of 2-chloroprocaine were detected in one (6%) of the maternal blood samples and four (25%) of the umbilical cord venous blood samples. The investigators concluded17:
In all of the studies of paracervical block with 2-chloroprocaine, there were no cases in which the abnormal fetal heart rate patterns were associated with depressed neonates. This is in contrast to the studies with amide local anesthetics and may be explained by the rapid enzymatic inactivation of 2-chloroprocaine.
Some obstetricians dislike 2-chloroprocaine because of its relatively short duration of action. However, in one study the mean duration of analgesia was 40 minutes after paracervical administration of either 2-chloroprocaine or lidocaine.16 A 2012 Cochrane Review concluded that the choice of local anesthetic agent did not affect maternal satisfaction with pain relief after paracervical block.6
Maternal Complications
Maternal complications of paracervical block are uncommon but may be serious (Box 24-1).19–22 Systemic local anesthetic toxicity may result from direct intravascular injection or rapid systemic absorption of the local anesthetic. Postpartum neuropathy may follow direct sacral plexus trauma, or it may result from hematoma formation. Retropsoal and subgluteal abscesses are rare but may result in maternal morbidity or mortality.21,22
Fetal Complications
In some cases, fetal injury results from direct injection of local anesthetic into the fetal scalp during paracervical block.23 Fetal scalp injection of 10 or 20 mL of local anesthetic undoubtedly causes systemic local anesthetic toxicity, which may result in fetal death. Fetal scalp injection seems more likely to occur when the obstetrician performs paracervical block in the presence of advanced (i.e., > 8 cm) cervical dilation.
Bradycardia is the most common fetal complication. Fetal bradycardia typically develops within 2 to 10 minutes after the injection of local anesthetic. Most cases resolve within 5 to 10 minutes, but some cases of bradycardia persist for as long as 30 minutes. Published studies have noted an incidence of bradycardia that varies between 0% and 70%.4,11,18,24–31 These figures represent extremes on either side of the true incidence of this complication. Some studies have overstated the problem by defining bradycardia as a baseline FHR of less than 120 bpm. (A baseline FHR of 110 bpm does not necessarily indicate fetal compromise.) Experienced obstetricians clearly do not encounter clinically significant fetal bradycardia after 70% of their paracervical blocks. It is equally clear that the incidence of clinically significant fetal bradycardia is not zero, and it is difficult to teach this technique without placing some fetuses at risk.
Shnider et al.26 reported that fetal bradycardia occurred after 24% of 845 paracervical blocks administered to 705 patients with either 1% mepivacaine, 1% lidocaine, or 1% propitocaine (prilocaine). Neonatal depression occurred significantly more often in infants who had FHR changes after paracervical block than in a control group or in a group of infants with no FHR changes after paracervical block. In contrast, Carlsson et al.27 performed 523 paracervical blocks with 0.125% or 0.25% bupivacaine in 469 women. Of the total, nine (1.9%) fetuses had bradycardia, but at delivery all nine of the newborns had a 5-minute Apgar score of 9 or 10.
Goins28 observed fetal bradycardia in 24 (13%) of 182 patients who received paracervical block with 20 mL of 1% mepivacaine. He compared neonatal outcome for these patients with neonatal outcome for 343 patients who received other analgesic/anesthetic techniques. There was a slightly higher incidence of low Apgar scores at 1 minute and 5 minutes in the paracervical block group, but the difference was not statistically significant. LeFevre18 observed fetal bradycardia after 46 (11%) of 408 paracervical blocks. Fetal bradycardia was more common in those patients with a nonreassuring FHR tracing before the performance of paracervical block.
In a review of four randomized controlled trials published between 1975 and 2000, Rosen30 estimated that the incidence of post–paracervical block fetal bradycardia is 15%. More recently, Volmanen et al.31 reviewed four studies of paracervical block that had adequate sample size (n > 200), used the superficial injection technique, and administered 0.125% or 0.25% bupivacaine. Among the 1361 patients in these four studies, the incidence of fetal bradycardia was 2.2%. The observed episodes of fetal bradycardia were transient and did not require emergency cesarean delivery.31
Etiology of Fetal Bradycardia
The etiology of fetal bradycardia after paracervical block is unclear. Investigators have offered at least four theories that might explain the etiology of fetal bradycardia, as discussed here.
Reflex Bradycardia.
Manipulation of the fetal head, the uterus, or the uterine blood vessels during performance of the block may cause reflex fetal bradycardia.25
Direct Fetal Central Nervous System and Myocardial Depression.
The performance of paracervical block results in the injection of large volumes of local anesthetic close to the uteroplacental circulation. Local anesthetic rapidly crosses the placenta32 and may cause fetal central nervous system (CNS) depression, myocardial depression, and/or umbilical vasoconstriction. Puolakka et al.33 observed that the most common abnormality after paracervical block was the disappearance of FHR accelerations. They speculated that FHR changes result from rapid transplacental passage of local anesthetic into the fetal circulation, followed by a direct toxic effect of the local anesthetic on the FHR regulatory centers.
Some investigators have suggested that fetal bradycardia results from a direct toxic effect of the local anesthetic on the fetal heart.34,35 Shnider et al.34 reported that in four cases of fetal bradycardia, mepivacaine concentrations in fetal scalp blood were higher than peak concentrations in maternal arterial blood. Asling et al.35 made similar observations in six of seven cases of fetal bradycardia. They suggested that local anesthetic reaches the fetus by a more direct route than maternal systemic absorption, and they speculated that high fetal concentrations of local anesthetic result from local anesthetic diffusion across the uterine arteries. This would lead to local anesthetic concentrations in intervillous blood that are higher than concentrations in maternal brachial arterial blood. High fetal concentrations would then occur from the passive diffusion of local anesthetic across the placenta.
High fetal concentrations of local anesthetic also may result from fetal acidosis and ion trapping.36,37 Local anesthetics are weak bases, and if acidosis develops in a fetus, increasing amounts of local anesthetic will cross the placenta regardless of the site of maternal injection. It is also possible that the obstetrician may directly inject local anesthetic into uterine blood vessels.
Most studies have noted that local anesthetic concentrations in the fetus are consistently lower than those in the mother after paracervical block.9 Further, fetal bradycardia has not consistently occurred in documented cases of fetal local anesthetic toxicity. Freeman et al.38 injected 300 mg of mepivacaine directly into the scalp of two anencephalic fetuses. The QRS complex widened, the PR interval lengthened, and both fetuses died, but fetal bradycardia did not occur before fetal death. In contrast, the investigators observed no widening of the QRS complex or lengthening of the PR interval in normal fetuses demonstrating bradycardia after paracervical block. Rather, the fetal electrocardiogram (ECG) changes were consistent with sinoatrial node suppression with a wandering atrial pacemaker. The investigators concluded that a mechanism other than direct fetal myocardial depression is responsible for fetal bradycardia after paracervical block.
Increased Uterine Activity.
Increased uterine activity results in decreased uteroplacental perfusion. Fishburne et al.39 noted that direct uterine arterial injection of bupivacaine consistently caused a significant increase in uterine tone in gravid ewes. Uterine arterial injection of 2-chloroprocaine did not affect myometrial tone, whereas injection of lidocaine had an intermediate effect.
Myometrial injection of a local anesthetic also may cause greater uterine activity. Morishima et al.40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


