1 Adolescent gynaecology
Pubertal Development and Primary Amenorrhoea
What is puberty and when does it occur?
Puberty is the physical, emotional and sexual transition from childhood to adulthood. It involves five changes: breast, pubic hair, axillary hair development, the growth spurt and the onset of menstruation. In girls pubertal development commences at around 8–9 years of age and lasts for 4–5 years. Precocious puberty is said to have occurred if pubertal development commences before then.1
What determines the onset of puberty?
The actual endocrine events that initiate puberty are unknown. It appears that puberty is held in check by higher central nervous system controls, but the restraint can be eliminated by injury or tumour growth, both of which can result in premature puberty. Gonadal steroids are produced as a result of increased gonadotrophin stimulation, and secondary sexual development follows a well-described pattern of changes.2
What is the sequence of events that occurs during puberty?
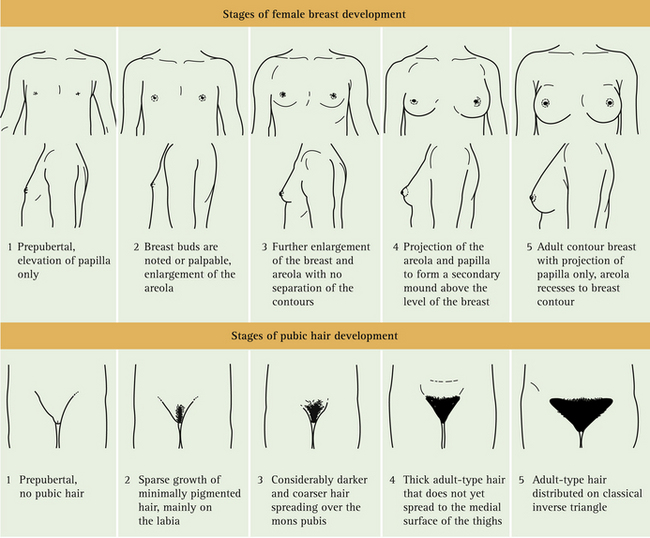
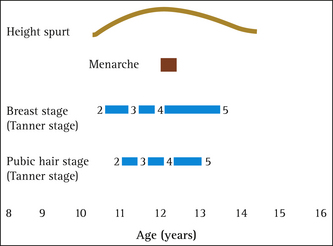
Usually there is a distinct chronological sequence to pubertal development. The first event to occur
is breast budding followed by sexual hair growth, the growth spurt and finally menarche. Tanner has described this sequence and in girls takes into account both breast and pubic hair development (Table 1.1).3 Axillary hair becomes evident approximately at Tanner’s stage 3, while the growth spurt occurs between Tanner’s stages 2 and 5, peaking at the onset of Tanner’s stage 4. Girls undergo this growth spurt on average two years earlier than boys and reach a peak growth velocity of 8 cm/year before the production of oestrogen eventually closes the epiphyses.4 Figure 1.1 shows the timing of pubertal events in graph form.
TABLE 1.1 Tanner’s stages of pubertal development
What is the average age of menarche?
Over the last century the average age of menarche has dropped by 3 years5 and now stands at 12.7 years.6 Factors contributing to this change include public health successes such as improved childhood nutrition and health status through reduction in childhood infections.7 While decreases in age at menarche until the mid-1960s resulted from ‘positive’ changes, such as better nutrition, it has been suggested that decreases since that time are related to ‘negative’ changes, such as overeating and decreased physical activity, and that these negative changes have brought about a disparity between physical and psychosocial maturity as well as a potential for increased rates of breast cancer later in life.8
What is a ‘normal’ adolescent menstrual pattern?
Most adolescent cycles range from approximately 20 to 45 days and last 2–7 days, even in the first gynaecological year. Cycles become more regular with increasing age and gynaecological age. By the third gynaecological year, 60–80% of cycles are 21–34 days long and a young woman’s ‘normal’ cycle length is established by approximately the fifth or sixth gynaecological year, or by age 19–20.9 It is important to note, however, that she may well have started some form of hormonal contraception by then and may never have had the opportunity to experience her ‘normal’ cycle.
When is a girl considered to have primary amenorrhoea?
Absence of periods is called primary amenorrhoea and should be investigated if there is a failure to establish menstruation by the age of 14 years in girls without signs of secondary sexual development, or by the age of 16 in the presence of normal secondary sexual characteristics.4 These age limits, while arbitrary, allow for variability in the normal rates of sexual maturation and the increasingly lower mean age of menarche.
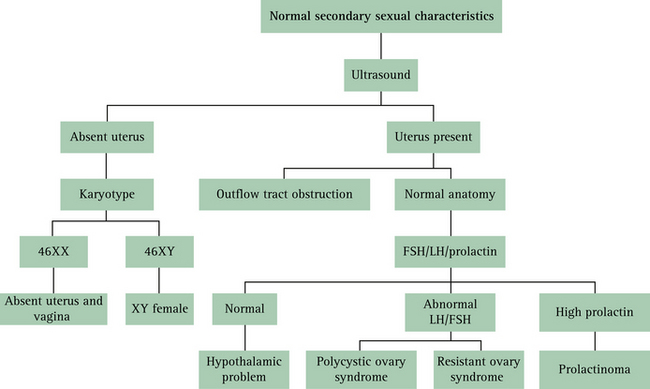
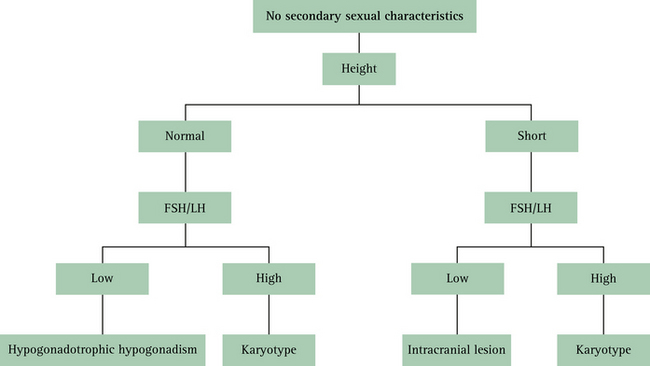
Primary amenorrhoea can be classified according to the presence or absence of secondary sexual characteristics. The onset of menstruation should usually occur within 2 years of the onset of breast development, pubic and axillary hair development and the growth spurt.10 Box 1.1 lists the possible causes of primary amenorrhoea when secondary sexual characteristics are present and Table 1.2 shows the causes of primary amenorrhoea when secondary sexual characteristics are absent. In this latter situation, classification is assisted by consideration of height.
BOX 1.1 Causes of primary amenorrhoea when secondary sexual characteristics are present
(Adapted from Edmonds54)
TABLE 1.2 Causes of primary amenorrhoea when secondary sexual characteristics are absent
| Normal stature | Short stature |
|---|---|
(Adapted from Edmonds54)
What history needs to be taken?
At the initial presentation, a history detailing the following issues needs to be taken:
What kind of investigative pathway should be followed?
If, when examining a young girl with primary amenorrhoea, normal secondary sexual characteristics are present but there is no family history of delayed menarche, the investigative pathway shown in Figure 1.2 should be followed. If, on the other hand, no secondary sexual characteristics are seen, GPs should assess height and follow the investigative pathway given in Figure 1.3 (p 6).
What common causes of primary amenorrhoea will a GP encounter?
From a general-practice or primary-care perspective, the most common cause of primary amenorrhoea is constitutional delay. This delay is caused by an immature pulsatile release of gonadotrophin-releasing hormone (GnRH), which eventually matures spontaneously. There is often a family history of delayed menarche or puberty in these girls.11 After constitutional delay, Turner’s syndrome and, more rarely, an absent vagina with a non-functioning uterus are the next most common causes of primary amenorrhoea seen in general practice.
Turner’s syndrome is caused by a chromosomal abnormality, whereby there is either complete absence or a partial abnormality of one of the two X chromosomes. The incidence of this syndrome is 1 in 2000 female births.12 The features of Turner’s syndrome are variable; they may include short stature, webbed neck, lymphoedema, a shield chest with widely spaced nipples, scoliosis, a wide carrying angle, coarctation of the aorta and streak ovaries.
Rokitansky-Kuster-Hauser syndrome is the name given to a condition where there is either partial or complete absence of the vagina, and a rudimentary uterus. It accounts for up to 15% of primary amenorrhoea cases.13 While ovarian development is normal, up to 40% of girls with this syndrome have associated renal tract abnormalities and 12% have skeletal abnormalities.14
Summary of key points
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree