Chapter 420 Acyanotic Congenital Heart Disease
The Left-to-Right Shunt Lesions
420.1 Atrial Septal Defect
Atrial septal defects (ASDs) can occur in any portion of the atrial septum (secundum, primum, or sinus venosus), depending on which embryonic septal structure has failed to develop normally (Chapter 414). Less commonly, the atrial septum may be nearly absent, with the creation of a functional single atrium. Isolated secundum ASDs account for ≈7% of congenital heart defects. The majority of cases of ASD are sporadic; autosomal dominant inheritance does occur as part of the Holt-Oram syndrome (hypoplastic or absent radii, 1st-degree heart block, ASD) or in families with secundum ASD and heart block.
Beda RD, Gill EAJr. Patent foramen ovale: does it play a role in the pathophysiology of migraine headache? Cardiol Clin. 2005;23:91-96.
Benson DW, Silberbach GM, Kavanaugh-McHugh A, et al. Mutations in the cardiac transcription factor NKX2.5 affect diverse cardiac developmental pathways. J Clin Invest. 1999;104:1567-1573.
Jategaonkar S, Scholtz W, Schmidt H, et al. Percutaneous closure of atrial septal defects: echocardiographic and functional results in patients older than 60 years. Circ Cardiovasc Interv. 2009;2:85-89.
Kharouf R, Luxenberg DM, Khalid O, et al. Atrial septal defect: spectrum of care. Pediatr Cardiol. 2008;29:271-280.
Masura J, Gavora P, Podnar T. Long-term outcome of transcatheter secundum-type atrial septal defect closure using Amplatzer septal occluders. J Am Coll Cardiol. 2005;45:505-507.
Radzik D, Davignon A, van Doesburg N, et al. Predictive factors for spontaneous closure of atrial septal defects diagnosed in the first 3 months of life. J Am Coll Cardiol. 1993;22:851-853.
Riggs T, Sharp SE, Batton D, et al. Spontaneous closure of atrial septal defects in premature vs full term neonates. Pediatr Cardiol. 2000;21:129-134.
Swartz EN. Is transcatheter device occlusion as good as open heart surgery for closure of atrial septal defects? Arch Dis Child. 2004;89:687-688.
Yew G, Wilson NJ. Transcatheter atrial septal defect closure with the Amplatzer septal occluder: five-year follow-up. Catheter Cardiovasc Interv. 2005;64:193-196.
420.2 Ostium Secundum Defect
Pathophysiology
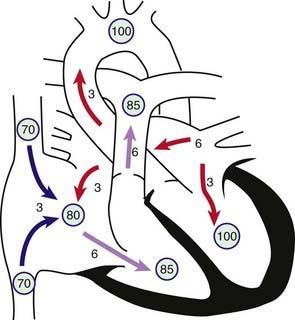
The degree of left-to-right shunting is dependent on the size of the defect, the relative compliance of the right and left ventricles, and the relative vascular resistance in the pulmonary and systemic circulations. In large defects, a considerable shunt of oxygenated blood flows from the left to the right atrium (Fig. 420-1). This blood is added to the usual venous return to the right atrium and is pumped by the right ventricle to the lungs. With large defects, the ratio of pulmonary to systemic blood flow (Qp : Qs) is usually between 2 : 1 and 4 : 1. The paucity of symptoms in infants with ASDs is related to the structure of the right ventricle in early life when its muscular wall is thick and less compliant, thus limiting the left-to-right shunt. As the infant becomes older and pulmonary vascular resistance drops, the right ventricular wall becomes thinner and the left-to-right shunt across the ASD increases. The increased blood flow through the right side of the heart results in enlargement of the right atrium and ventricle and dilatation of the pulmonary artery. The left atrium may also be enlarged, but the left ventricle and aorta are normal in size. Despite the large pulmonary blood flow, pulmonary arterial pressure is usually normal because of the absence of a high-pressure communication between the pulmonary and systemic circulations. Pulmonary vascular resistance remains low throughout childhood, although it may begin to increase in adulthood and may eventually result in reversal of the shunt and clinical cyanosis.
Diagnosis
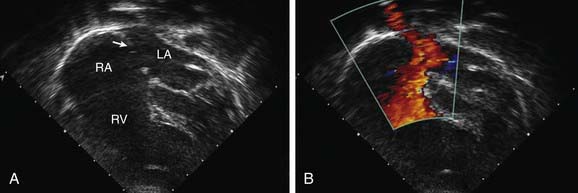
The echocardiogram shows findings characteristic of right ventricular volume overload, including an increased right ventricular end-diastolic dimension and flattening and abnormal motion of the ventricular septum (Fig. 420-2). A normal septum moves posteriorly during systole and anteriorly during diastole. With right ventricular overload and normal pulmonary vascular resistance, septal motion is either flattened or reversed—that is, anterior movement in systole. The location and size of the atrial defect are readily appreciated by two-dimensional scanning, with a characteristic brightening of the echo image seen at the edge of the defect (T-artifact). The shunt is confirmed by pulsed and color flow Doppler. The normal entry of all pulmonary veins into the left atrium should be confirmed.
Treatment
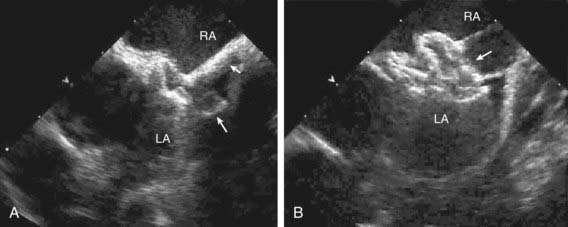
Surgical or transcatheter device closure is advised for all symptomatic patients and also for asymptomatic patients with a Qp : Qs ratio of at least 2 : 1 or those with right ventricular enlargement. The timing for elective closure is usually after the 1st yr and before entry into school. Closure carried out at open heart surgery is associated with a mortality rate of <1%. Repair is preferred during early childhood because surgical mortality and morbidity are significantly greater in adulthood; the long-term risk of arrhythmia is also greater after ASD repair in adults. For most patients, the procedure of choice is percutaneous catheter device closure using an atrial septal occlusion device, implanted transvenously in the cardiac catheterization laboratory (Fig. 420-3). The results are excellent and patients are discharged the following day. With the latest generation of devices, the incidence of serious complications such as device erosion is 0.1% and can be decreased by identifying high-risk patients such as those with a deficient rim of septum around the device. Echocardiography can usually determine whether a patient is a good candidate for device closure. In patients with small secundum ASDs and minimal left-to-right shunts without right ventricular enlargement, the consensus is that closure is not required. It is unclear at present whether the persistence of a small ASD into adulthood increases the risk for stroke enough to warrant prophylactic closure of all these defects.
420.4 Partial Anomalous Pulmonary Venous Return
One or several pulmonary veins may return anomalously to the superior or inferior vena cava, the right atrium, or the coronary sinus and produce a left-to-right shunt of oxygenated blood. Partial anomalous pulmonary venous return usually involves some or all of the veins from only one lung, more often the right one. When an associated ASD is present, it is generally of the sinus venosus type, although can be of the secundum type (Chapter 420.3). When an ASD is detected by echocardiography, one must always search for associated partial anomalous pulmonary venous return. The history, physical signs, and electrocardiographic and roentgenographic findings are indistinguishable from those of an isolated ostium secundum ASD. Occasionally, an anomalous vein draining into the inferior vena cava is visible on chest radiography as a crescentic shadow of vascular density along the right border of the cardiac silhouette (scimitar syndrome); in these cases, an ASD is not usually present, but pulmonary sequestration and anomalous arterial supply to that lobe are common findings. Total anomalous pulmonary venous return is a cyanotic lesion and is discussed in Chapter 425.7. Echocardiography generally confirms the diagnosis. MRI and CT are also useful if there is a question regarding pulmonary venous drainage or in cases of scimitar syndrome. If cardiac catheterization is performed, the presence of anomalous pulmonary veins is demonstrated by selective pulmonary arteriography and anomalous pulmonary arterial supply to the right lung is demonstrated by descending aortography.
420.5 Atrioventricular Septal Defects (Ostium Primum and Atrioventricular Canal or Endocardial Cushion Defects)
Transitional varieties of these defects also occur and include ostium primum defects with clefts in the anterior mitral and septal tricuspid valve leaflets and small ventricular septal defects, and, less commonly, ostium primum defects with normal AV valves. In some patients, the atrial septum is intact, but an inlet VSD is similar to that found in the full AV septal defect. Sometimes AV septal defects are associated with varying degrees of hypoplasia of one of the ventricles, known as either left- or right-dominant AVSD. If the affected ventricular chamber is too small to establish a two ventricle circulation, then surgical palliation, aiming for an eventual Fontan procedure, is performed (Chapters 424.4 and 425.10).
Pathophysiology
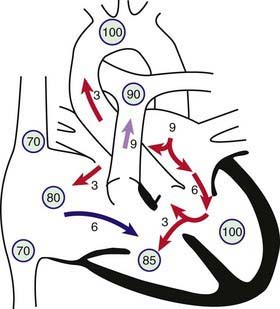
In complete AV septal defects, the left-to-right shunt occurs at both the atrial and ventricular levels (Fig. 420-4). Additional shunting may occur directly from the left ventricle to the right atrium because of absence of the AV septum. Pulmonary hypertension and an early tendency to increase pulmonary vascular resistance are common. AV valvular insufficiency increases the volume load on one or both ventricles. If the defect is large enough, some right-to-left shunting may also occur at both the atrial and ventricular levels and lead to mild arterial desaturation. With time, progressive pulmonary vascular disease increases the right-to-left shunt so that clinical cyanosis develops (Eisenmenger physiology, Chapter 427.2).