Chapter 422 Acyanotic Congenital Heart Disease
Regurgitant Lesions
422.1 Pulmonary Valvular Insufficiency and Congenital Absence of the Pulmonary Valve
Congenital absence of the pulmonary valve is usually associated with a ventricular septal defect, often in the context of tetralogy of Fallot (Chapter 424.1). In many of these neonates, the pulmonary arteries become widely dilated and compress the bronchi, with subsequent recurrent episodes of wheezing, pulmonary collapse, and pneumonitis. The presence and degree of cyanosis are variable. Florid pulmonary valvular incompetence may not be well tolerated, and death may occur from a combination of bronchial compression, hypoxemia, and heart failure. Correction involves plication of the massively dilated pulmonary arteries, closure of the ventricular septal defect, and placement of a homograft across the right ventricular outflow tract.
McDonnell BE, Raff GW, Gaynor JW, et al. Outcome after repair of tetralogy of Fallot with absent pulmonary valve. Ann Thorac Surg. 1999;67:1391-1395.
Pinsky WW. Absent pulmonary valve syndrome. In: Garson A, Bricker JT, Fisher DJ, et al, editors. The science and practice of pediatric cardiology. Baltimore: Williams & Wilkins; 1998:1413-1419.
422.2 Congenital Mitral Insufficiency
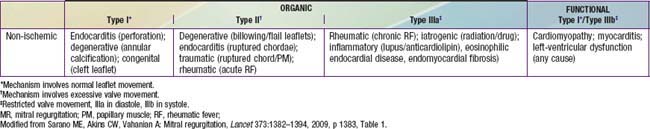
Congenital mitral insufficiency is rare as an isolated lesion and is more often associated with other anomalies. It is most commonly encountered in combination with an atrioventricular septal defect, either an ostium primum defect, or a complete AV septal defect (Chapter 420.5). Mitral insufficiency is also seen in patients with dilated cardiomyopathy (Chapter 433.1) as their left ventricular function deteriorates, secondary to dilatation of the valve ring. Mitral insufficiency may also be encountered in conjunction with coarctation of the aorta, ventricular septal defect, corrected transposition of the great vessels, anomalous origin of the left coronary artery from the pulmonary artery, or Marfan syndrome. In the absence of other congenital heart disease, endocarditis or rheumatic fever should be suspected in a patient with isolated severe mitral insufficiency (Table 422-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree