(6)
Department of Newborn Research, The Royal Women’s Hospital, 20 Flemington Rd, Parkville, VIC, 3052, Australia
Acute respiratory failure requiring assisted ventilation is one of the most common reasons for admission to the neonatal intensive care unit. Respiratory failure is the inability to maintain either normal delivery of oxygen to the tissues or normal removal of carbon dioxide from the tissues. It occurs when there is an imbalance between the respiratory workload and ventilatory strength and endurance. Definitions are somewhat arbitrary but suggested laboratory criteria for respiratory failure include two or more of the following: PaCO2 > 60 mmHg, PaO2 < 50 mmHg or O2 saturation <80 % with an FiO2 of 1.0 and pH < 7.25 (Wen et al. 2004).
Many have observed that neonates are not merely small adults. Infants have less respiratory reserve than older individuals, and respiratory failure is more common, not only during pulmonary illnesses but also any serious illness. Infants have narrow, compliant airways which are prone to collapse. Their chest wall is not ossified and has low muscle mass. It is very compliant, which in combination with a low functional residual capacity puts the infant at risk of airway collapse and atelectasis. The low recoil of the chest wall means that little pressure is required to expand the chest wall. In contrast to older subjects, the major force contributing to elastic recoil is surface tension at the air-liquid interface in the distal airways and alveoli. Surfactant deficiency, both primary and secondary, leads to decreased stability of the small terminal airways and alveoli and ultimately to collapse.
Assisted ventilation aims to (1) maintain adequate oxygenation, supporting gas exchange by improving alveolar ventilation, (2) restore or maintain functional residual capacity to prevent atelectasis or reopen areas of collapsed lung and (3) reduce the work of breathing in the presence of high airway resistance and/or reduced compliance. For neonates, the aim is to gently support the patient in order to allow time for the resolution of the underlying disorder without causing further injury through ventilation.
47.2 Pulmonary Pathologies in the Neonate Leading to Respiratory Failure
Louise S. Owen7 and Peter G. Davis7
(7)
Department of Newborn Research, The Royal Women’s Hospital, 20 Flemington Rd, Parkville, VIC, 3052, Australia
Educational Aims
To describe the pathology and physiology of RDS
To outline the risk factors associated with RDS
To describe the impact of delivery room and early management of RDS on outcome
To delineate the range of non-invasive and invasive modes of respiratory support available to treat RDS
To outline the importance of instituting a lung protective ventilatory strategy to reduce the risk of developing BPD
To outline the role of additional therapies in the treatment of RDS
To describe the complications and outcomes of RDS
47.2.1 Infant Respiratory Distress Syndrome
Respiratory distress syndrome (RDS) remains the most common reason for admission to neonatal intensive care and is associated with significant morbidity and mortality (Wen et al. 2004; Horbar et al. 2002). RDS develops due to immaturity of the surfactant synthesis systems, insufficiency of surfactant production and structural immaturity of the lungs.
47.2.1.1 Pathophysiology of RDS
47.2.1.1.1 Lung Development
Human lung development falls into distinct stages: the pseudoglandular stage from 5 to 17 weeks gestation, the canalicular stage from 16 to 26 weeks gestation, the saccular stage between 24 and 38 weeks and the alveolar stage from 36 weeks until 2 years. During the canalicular phase, there is ongoing branching of the respiratory bronchioles with thinning of the airway epithelium, so that by the end of this period there is some capability for gas exchange. During the saccular stage, the peripheral airways widen into saccules which then form the alveolar ducts, the precursor to alveoli. Infants born during this period do not have fully functioning terminal airways; there are fewer, thick-walled gas exchange units. The true alveolar stage does not start until 36 weeks gestation and continues postnatally until about 2 years of age. The development of fully functional alveoli is also dependent on development of the surrounding mesenchyme and the alveolar capillaries.
47.2.1.1.2 Transition
The transition from fetal life to newborn life involves multiple processes. The most important adaptation is the conversion of the lungs from a fluid-filled unit to air-filled spaces, capable of working as a gas exchange organ. In utero, the terminal airways are full of fluid secreted from the pulmonary epithelial cells. This fluid is an important determinant of lung growth. The volume of fluid is equivalent to functional residual capacity (FRC) post delivery. Following delivery, lung fluid is cleared. This process is slower and less efficient in preterm infants (Egan et al. 1984). The sequence of lung inflation, fluid clearance and rising pH controls the early fall in pulmonary vascular resistance and initial oxygenation. The action of the respiratory muscles overcomes the resistive properties of the airways to develop FRC and tidal volume (Sinha et al. 2008). Antenatal, perinatal and resuscitation events interact to affect the processes of lung fluid clearance, FRC development and maintenance of adequate tidal volume.
47.2.1.1.3 Physiology
RDS is characterised by stiff non-compliant lungs with low levels of surfactant. Premature lungs have insufficient alveolarisation, decreased functional surface area, increased distance from alveoli to adjacent capillaries and reduced surfactant synthesis and show less hysteresis than normal lungs. The terminal airways collapse at end of expiration due to high surface tension. Tidal volumes are small and the dead space is relatively large. Infants are able to increase their respiratory rate to compensate for the low tidal volume. This means they may be able to maintain their minute volume, but the work of breathing is doubled (Hjalmarson and Olsson 1974; McCann et al. 1987). Most infants have some surfactant at birth (Reynolds et al. 1968) but levels fall within a few hours as alveolar protein leak inhibits function (Ikegami et al. 1983). Without exogenous surfactant infants tire, minute volume falls and hypoxia and acidaemia follows. This further increases surfactant inhibition.
47.2.1.1.4 Histology
Hyaline membranes are the characteristic histological finding in RDS and have given the disease its alternative name of hyaline membrane disease. In immature, stiff, surfactant deficient lungs, alveolar epithelial cell death starts to occur in the first hour after birth. Dead cells detach from the basement membrane, denuded patches appear, and protein leak leads to interstitial oedema. Hyaline membranes form; they consist of plasma protein, fibrin, cellular debris, red blood cells, macrophages and proteinaceous exudate. The material lines or fills the air spaces inhibiting gas exchange. Most of the protein leak occurs over the first 24 h (Ikegami et al. 1992). During this time the hyaline membranes, which are initially patchy, become more confluent. Ischaemia exacerbates RDS with epithelial necrosis occurring in the terminal airways. Asphyxiated infants have more severe RDS (Linderkamp et al. 1978) and respond less well to surfactant treatment (Skelton and Jeffery 1996).
After 24 h, inflammatory cell numbers increase and macrophages start to ingest the membranous material. Epithelial regeneration commences after 48 h and surfactant production starts to increase. Microscopically, the surfactant deficient lung is characterised by collapsed air-spaces alternating with hyper-expanded areas, vascular congestion and hyaline membranes. The lungs remain non-compliant and atelectatic until surfactant reappears at 36–48 h (Kanto et al. 1976). Hyaline membranes are broken down by the seventh day but will persist for longer if the infant is receiving mechanical ventilation. Healing is hyperplastic with shedding of the bronchiolar epithelial cells. Proteinaceous material in the terminal airways induces scarring and fibrosis in the developing alveoli and ultimately can lead to bronchopulmonary dysplasia or chronic lung disease (CLD).
47.2.1.1.5 Clinical Picture
The diagnosis of RDS is made on the basis of the clinical picture and the chest x-ray which demonstrates decreased lung volumes and a bell-shaped chest. Uniform infiltrates described as a ‘ground glass’ appearance involve all lobes of the lungs. Air bronchograms are seen as the infiltrate outlines the larger airways that remain air filled. In severe cases, the infiltrates are such that the cardiac and diaphragmatic borders become indistinct giving a ‘white-out’ appearance. Infants increase their respiratory rate, take smaller volume breaths and use accessory muscles to assist with their increased work of breathing. This results in nasal flaring and rib, sternal and subcostal recession. Infants attempt to stop alveolar collapse at end expiration by closing the glottis, resulting in grunting. As the infant tires, cyanosis develops and the infant develops apnoeic episodes with desaturations. Infants with RDS have decreased urine output and commonly become oedematous. The differential diagnosis includes infection (particularly group B streptococcal infection), persistent pulmonary hypertension of the newborn, aspiration pneumonia, lung malformations and upper airway obstruction, transient tachypnoea of the newborn, meconium aspiration syndrome, air leak syndromes, pulmonary haemorrhage, asphyxia, congenital heart disease, primary neurological or neuromuscular disease and inborn errors of metabolism.
47.2.1.2 Lung Mechanics of RDS
47.2.1.2.1 FRC and Physiological Dead Space
The effects of RDS on lung function vary with gestational and postnatal age. Newborns with normal lungs quickly develop an FRC of about 30 mL/kg (McCann et al. 1987). FRC is the volume of gas remaining in the lungs at the end of normal expiration, preventing alveolar collapse and allowing the lung to operate at optimal efficiency. Less mature infants have lower lung volumes, including a lower FRC; however, tidal volume remains about the same at 4–6 mL/kg (Hislop et al. 1986). These effects proportionally increase the physiological dead space to 60–80 % of tidal volume, compared with 30–40 % of tidal volume in healthy lungs (Avery et al. 1981). To compensate for this increased dead space, infants with RDS increase their respiratory rates. For infants without RDS, a rise in respiratory rate can lead to gas trapping; however, in babies with RDS, an increased respiratory rate may be enough to help maintain necessary FRC and avoid end-expiratory alveolar collapse. Newborn FRC already approaches alveolar closing volume, so a reduction in FRC permits atelectasis to readily develop. Further loss of FRC occurs due to vascular congestion, interstitial oedema and proteinaceous exudates.
Infants with RDS try to preserve lung function by delaying contraction of the diaphragm to delay the loss of thoracic volume and keep the alveoli inflated (Davis and Bureau 1987). Infants also contract the laryngeal muscles to keep the upper airway closed until late expiration, and then when these muscles relax, the abdominal muscles contract. The explosive release of air sounds as a grunt. Grunting helps to delay air escape from the lung and maintains FRC. It has been demonstrated that when an endotracheal tube is inserted, the loss of these mechanisms result in a fall in arterial oxygenation (Harrison et al. 1968). Surfactant treatment helps to increase lung volumes, so that lower positive pressures are required for ventilation. Higher lung volumes are maintained even when positive pressure is reduced because FRC increases following surfactant treatment (Goldsmith et al. 1991). Most lung volume improvement is seen when exogenous surfactant containing surfactant proteins are used (Rider et al. 1993). As FRC improves oxygenation improves. This normally occurs as lung fluid clears (Engle et al. 1983) or following surfactant treatment (Edberg et al. 1990) or when using distending pressure, such as mechanical ventilation (Richardson and Jung 1978). In an infant with RDS, the FRC returns to normal by about day 7.
47.2.1.2.2 Time Constant, Compliance and Resistance
Infants with RDS have less compliant, more resistant lungs. This results in a short time constant, meaning that gas leaves the terminal airways more quickly than in normal lungs. Surfactant-deficient lungs, with high surface tension in the alveoli, exhibit collapse in expiration of the smaller alveoli. This leads to overdistension of the larger alveoli that have remained open. Compliance is reduced as fewer terminal air spaces are ventilated, and those that are open become overdistended. Alveolar instability affects compliance as the critical opening and closing pressures vary. This means that alveoli open and shut suddenly, smaller ones then stay closed and open alveoli overfill. There is increased resistance in the lungs due to reduced cross-sectional area of the patent airways to the distal lung units. During spontaneous breathing the activity of the respiratory muscles tries to overcome elastic resistance and inertia of the tissues by increasing the change in intrapleural pressure, resulting in distortion of the compliant chest wall. Pulmonary compliance improves more slowly, following surfactant administration, than the rapid improvement seen in FRC (Edberg et al. 1990). This is reflected by quick improvement in oxygenation, compared with the relatively slower fall in carbon dioxide. The reduced compliance slowly returns to normal around day 7.
47.2.1.2.3 Gas Exchange and Shunting
Arterial carbon dioxide levels rise in RDS due to alveolar underventilation from atelectasis and the proportional increase in dead space. Most hypoxia in RDS is due to right-to-left shunting. Small shunts exist across the foramen ovale (if right atrial pressure is higher than left atrial pressure) and the ductus arteriosus (which is often patent in infants with RDS for 48 h). These shunts only account for about 10 % of the shunt in RDS (Seppanen et al. 1994) and are more important in other lung pathologies such as persistent pulmonary hypertension. In RDS, the most important shunt is intrapulmonary, as capillary blood travels through unventilated, or hypoventilated, atelectatic areas of the lung. Pulmonary arterial pressure normally falls rapidly, to half of the in utero level, soon after birth, but in RDS it can remain high for the first week (Evans and Archer 1991). The pulmonary pressure is proportionately higher in infants with more severe RDS and can exacerbate the hypoxia seen in RDS.
47.2.1.3 Epidemiology of RDS
Risk of RDS varies with lung maturity, which is intrinsically related to gestational age. Lung maturity is altered by the use of antenatal steroids and by postnatal surfactant treatment. Premature infants have lower levels of surfactant, although in almost all infants, there is some surfactant present within a few hours of birth (Reynolds et al. 1968). If newborn infants are not given surfactant, then levels fall as protein leak and oedema increase and the infant tires. The resulting hypoxia and acidosis reduce surfactant synthesis, and the clinical condition deteriorates further.
47.2.1.3.1 Prevention of RDS
Ideally prevention of RDS would focus on avoiding preterm birth. Addressing social deprivation and reducing rates of genital tract infection and preterm rupture of the membranes, both of which increase preterm delivery, could reduce RDS rates. If preterm labour occurs, or maternal disease necessitates preterm delivery, pharmaceutical intervention such as tocolytics may prolong pregnancy for 48 h. This is sufficient time to administer steroid treatment and reduce the risk of RDS. Antibiotics for suspected infection, or for membrane rupture, reduces progression to preterm delivery (Gomez et al. 1995). Other factors which impact on RDS development include asphyxia and drug depression of the infant. Care in avoiding intra- and postpartum asphyxia and minimal use of maternally administered opiates, anaesthetics, benzodiazepines and magnesium sulphate may also reduce rates of RDS.
47.2.1.3.2 Antenatal Steroids
Synthetic steroids given antenatally as betamethasone or dexamethasone, to women at risk of preterm delivery, reduce rates of RDS (odds ratio (OR) 0.63, 95 % confidence interval (CI) 0.44, 0.82). Neonatal deaths are reduced (OR 0.6, 95 % CI 0.48, 0.75) (Crowley 1995) as are rates of germinal matrix/intraventricular haemorrhage and necrotising enterocolitis (Ward 1994). The widespread uptake of antenatal steroid use has had a dramatic impact on the epidemiology of RDS over the last 20 years. Steroids induce enzymes for surfactant synthesis, induce genes for synthesis of surfactant protein (Mendelson et al. 1993), improve the quality of the surfactant produced (Ueda et al. 1995; Lanteri et al. 1994), mature the lung tissue and increase the number of alveolar divisions (Lanteri et al. 1994). The optimal timing of steroid administration has been shown to be 24–168 h prior to delivery (Crowley 1995). Some benefit can be seen with doses given 4–24 h prior to delivery (Sen et al. 2002). There is limited evidence of benefit below 28 weeks gestation (Garite et al. 1992) or beyond 34 weeks gestation (Liggins and Howie 1972). Steroids appear to be safe in terms of effect on maternal pregnancy-induced hypertension (Lamont et al. 1983), prolonged rupture of the membranes (Crowley 1995) and maternal diabetes. No long-term adverse outcomes have been demonstrated in infants following a single course of antenatal steroids (Dessens et al. 2000).
Repeated courses of steroids continue to improve neonatal outcomes in terms of lung function but may be detrimental to fetal growth and brain function (Aghajafari et al. 2002). A randomised controlled trial (RCT) in Australia demonstrated that repeated doses of antenatal corticosteroids reduced neonatal morbidity, compared with a single course, without changing neurosensory disability or body size at age 2 (Crowther et al. 2007). Another RCT of repeated versus single-steroid courses found a non-statistically significant increased rate of cerebral palsy in the repeated course group (Wapner et al. 2007); this question warrants further study. A retrospective review of infants who received multiple courses of steroids, compared with infants who received no antenatal steroids, showed that repeated courses were associated with decreased head circumference, decreased body mass index and decreased salivary cortisol at age 6–10 years (Chen et al. 2008). A Cochrane review of multiple doses of antenatal steroids published in 2007 concluded that further long-term data were required (Crowther and Harding 2007), and a review of this topic published in mid-2009 concluded that concerns about brain growth following repeated courses of antenatal corticosteroid currently warranted restriction of use to a single course (Newnham and Jobe 2009).
47.2.1.4 Incidence of RDS
Prior to the use of antenatal steroids and surfactant, the incidence of RDS in newborns in Europe was 2–3 % (Hjalmarson 1981). In the mid-1980s in the USA, the incidence was reported as 1.72 % (Becerra et al. 1992). In the modern era with widespread use of antenatal steroids and surfactant, the figures quoted are less than 1 % (Rubaltelli et al. 1998). The incidence of RDS decreases with advancing gestational age, from more than 50 % in infants born at 28 weeks gestation to around 25 % in those born at 31 weeks gestation. This fall reflects the increase in endogenous surfactant production between these ages.
47.2.1.5 Risk Factors for RDS
47.2.1.5.1 Gestation
Risk factors for RDS have been well demonstrated, with prematurity being the most important. Incidence of RDS is inversely proportional to gestational age; the majority of infants born before 28 weeks gestation will have some degree of respiratory distress. RDS remains a significant problem until around 34 weeks of gestation (Lewis et al. 1996); by 35–36 weeks gestation, incidence falls to 2 % (Rubaltelli et al. 1998). Not only are preterm lungs less mature in terms of surfactant synthesis, but epithelial protein leak is worse in these infants, leading to increased surfactant inhibition. Preterm infants are more at risk of other factors that impact on the incidence of RDS such as asphyxia, hypoxia, cold and hypotension.
47.2.1.5.2 Maternal Factors
Infants of diabetic mothers are at higher risk of developing RDS as they have abnormal surfactant synthesis (Ojomo and Coustan 1990), and insulin delays the maturation of type 2 alveolar cells delaying surfactant production (Gross et al. 1980). Maternal hypertension and prolonged membrane rupture protect against RDS. Stress raises the fetal cortisol and induces lung maturation.
Maternal alcohol use (Ioffe and Chernick 1987), smoking (Lieberman et al. 1992) and opioid and cocaine abuse all reduce RDS in the infant. Heroin is known to mature surfactant systems, and animal models of antenatal cocaine use have shown that cocaine induces surfactant synthesis (Sosenko 1993).
Antenatal steroids protect against RDS (see section on Epidemiology of RDS).
47.2.1.5.3 Fetal Factors
Male infants are at higher risk of developing RDS and suffer a more severe course. Incidence in males is 1.7 times higher, and males are more likely to die from the condition (Farrell and Avery 1975). This gender difference appears to be related to the effects of androgens which delay the maturation of the lecithin-sphingomyelin ratio and delay production of phosphatidylcholine in surfactant (Torday 1992).
Race plays a part in risk of RDS with infants of black race relatively protected. Black infants have about a one-third lower incidence than Caucasians (Hulsey et al. 1993). This protection exists even in the most immature infants (Kavvadia et al. 1998). When looking at lecithin-sphingomyelin ratio to assess lung maturity, for the same ratio more Caucasian infants develop RDS than black infants (Richardson and Torday 1994). It is hypothesised that there may be allelic variation in surfactant proteins causing this disparity (Rishi et al. 1992).
Growth-restricted infants are more likely to develop RDS, and the disease is more severe, compared with normal weight infants of the same gestation. Growth restriction is not as strong a risk factor as gestation, so a preterm infant of similar weight to a growth-restricted older infant is more likely to develop RDS than a growth-restricted child (Piper et al. 1996).
In multiple pregnancies the second, or higher birth order infant, is at more risk of developing RDS, as are infants born following a rapid labour.
Genetic conditions resulting in surfactant protein deficiencies are a rare cause of RDS, e.g. autosomal recessive surfactant protein B deficiency. Partial protein deficiencies and polymorphisms of parts of the proteins have also been described (Cole et al. 2000; Makri et al. 2002). A family history of a sibling with RDS increases the risk for the subsequent infant.
47.2.1.5.4 Delivery Factors
Infants born by caesarean section (CS) are at higher risk of developing RDS. Infants born by CS after a period of time in labour have more surfactant in their airway than those born without labour (Callen et al. 1979). CS without labour is associated with more RDS and transient tachypnoea of the newborn (Annibale et al. 1995; Cohen and Carson 1985; Morrison et al. 1995). Risk of RDS following elective CS without labour continues to fall between 37 and 40 weeks of gestation.
Asphyxia results in reduced lung perfusion, and ischaemia causes capillary damage. Recovery and reperfusion cause protein leak from damaged capillaries, worsening RDS (Jefferies et al. 1984). The function of surfactant decreases with acidosis and low temperature; below 34 °C surfactant cannot spread, and therefore cold or acidotic infants are more likely to develop RDS (Gluck et al. 1972).
47.2.1.6 Stepwise Approach to Respiratory Support for RDS
Management of newborn infants who either have or are likely to develop RDS is twofold: firstly, there is the need to provide initial support for the respiratory distress, and second is the instigation of the optimal lung protective strategy to prevent development of BPD. BPD will affect up to 40 % of infants born before 29 weeks, presenting a significant healthcare burden (Patel and Greenough 2008). Every effort should be made to deliver preterm infants at high risk of RDS in centres with the appropriate skills and resources available to provide the best possible care (Sweet et al. 2007).
47.2.1.6.1 Delivery Room Management
Most very premature infants will need some form of respiratory support in the first few minutes of life. Most resuscitation guidelines are drawn up with term infants in mind and may not translate accurately to preterm infants at high risk of RDS and BPD. Until recently premature infants were routinely stabilised using 100 % oxygen; many were intubated and given surfactant as a standard procedure, regardless of their respiratory effort. We now know that 100 % oxygen is not the best choice of gas to use (Saugstad et al. 2008) and several studies are underway to determine the most appropriate initial oxygen concentration to use, as well as the best oxygen saturations to target (Castillo et al. 2008). Centile charts for normal oxygen saturations for preterm infants are now being developed (Dawson et al. 2009a). There are good theoretical, clinical and animal data for using positive end-expiratory pressure (PEEP) at delivery. Animal data have demonstrated that PEEP reduces alveolar-arterial oxygen gradient (Probyn et al. 2004), protects from lung injury (Jobe et al. 2002), preserves the surfactant pool (Michna et al. 1999), improves oxygenation and improves ventilation-perfusion matching (Schlessel et al. 1989; Finer et al. 2004). PEEP also accelerates formation of FRC (Siew et al. 2009) and protects the lungs by keeping the alveoli open (Nilsson et al. 1980). Using a resuscitation device that is able to give PEEP would seem advantageous but so far has not shown improved outcomes in terms of saturations at 5 min or need for endotracheal intubation (Dawson et al. 2009b). Use of CPAP to treat preterm infants has been shown to reduce rates of endotracheal intubation (Lindner et al. 1999; Lundstrom 2003; Stevens et al. 2007), but the disadvantage is that any surfactant treatment is delayed. PEEP or CPAP from the delivery room onward has been shown to be as good as initial ventilation and surfactant treatment, but not any better (Morley et al. 2008), and is discussed further in the CPAP section of this chapter. CPAP and sustained inflations can be used to help the infant establish FRC (te Pas et al. 2009a; te Pas and Walther 2007). It is important to carefully control any positive pressure support given in the delivery room to avoid damaging the lungs. Animal studies have shown that even a few large volume inflations can damage newborn lungs (Bjorklund et al. 1997; Dreyfuss and Saumon 1992; Hernandez et al. 1989) and currently the majority of respiratory support systems used in the delivery room do not allow the clinician to measure the delivered volume (Schmolzer et al. 2010). In the absence of respiratory function, monitoring the initial stabilisation and transfer from the delivery room to the neonatal intensive care unit (NICU) should be guided by oxygen saturations and chest movement. However, Tracy et al. suggest that this clinically determined ventilation commonly results in hypocarbia, hyperoxia or both (Tracy et al. 2004).
47.2.1.6.2 General Management
Infants with RDS should be nursed in a thermo-neutral environment, with cardiovascular and respiratory monitoring. Once initial examination is complete, infants should be handled as little as possible and nursed prone to maximise oxygenation and respiratory muscle coordination (Hand et al. 2007; Leipala et al. 2003; Wells et al. 2005). As RDS is clinically indistinguishable from sepsis, infants with ongoing respiratory symptoms should have intravenous access, blood sent for full blood count, a chest x-ray, septic markers and blood culture and should receive antibiotics.
Infants with significant increased work of breathing should not initially receive enteral feeds, but be managed with intravenous fluid titrated against urine output and plasma sodium. Very low birth weight infants who are likely to need ongoing respiratory support require early parental nutrition for optimal lung growth and recovery. Anaemia and coagulation abnormalities need to be carefully controlled; blood pressure should be maintained with crystalloid and if necessary with inotropic support. Arterial oxygen levels should be kept between 50 and 75 mmHg (7–10 kPa); ongoing clinical trials, such as BOOST2, aim to determine the optimal oxygen saturations for this group of infants. The European Consensus Guidelines on the Management of Neonatal RDS currently recommend that oxygen saturations, in infants receiving supplemental oxygen, should be kept below 95 % (Sweet et al. 2007). Hypocarbia must be avoided due to the effect on cerebral blood flow (Garland et al. 1995). A degree of permissive hypercarbia appears safe (Miller and Carlo 2007) and is associated with lower rates of BPD (Thome and Ambalavanan 2009).
47.2.1.6.3 Supplemental Oxygen
Infants with the mildest degree of RDS may need only supplemental oxygen and good general care. Supplemental oxygen may be delivered into the isolette, given directly as subnasal oxygen or delivered via a hood or head box. With increasing disease severity, oxygen requirements climb, work of breathing increases, the infant tires, carbon dioxide (PaCO2) levels rise and the pH falls. The infant may have desaturations or apnoeas at which point positive pressure support is required. The British Association of Perinatal Medicine (BAPM) suggests instigation of CPAP support if the inspired oxygen requirement reaches 40 %, if the pH falls below 7.25 or if the PaCO2 rises above 50 mmHg (6.7 kPa) (British Association of Perinatal Medicine T 2005).
47.2.1.6.4 Continuous Positive Airway Pressure
CPAP was first used in neonates in 1971 (Gregory et al. 1971) and has grown hugely in popularity, particularly over the last 15 years. It has been advocated as a gentler form of respiratory support (Jacobsen et al. 1993) and has been shown to have many physiological benefits. These include decreasing the likelihood of upper airway collapse and decreasing upper airway resistance by splinting and increasing the cross-sectional area of the pharynx (Miller et al. 1990). CPAP reduces obstructive apnoeas (Miller et al. 1985) and alters the shape of the diaphragm, improving lung compliance and decreasing lung resistance (Gaon et al. 1999). It allows larger tidal volumes for the same respiratory effort and conserves surfactant. CPAP has also been demonstrated to increase FRC (Richardson and Jung 1978; Richardson et al. 1980), stabilise the chest wall (Locke et al. 1991), improve lung volumes (Harris et al. 1976; Yu and Rolfe 1977) and improve oxygenation (Durand et al. 1983).
47.2.1.6.4.1 Generating CPAP Pressure
CPAP can be generated by a ventilator, by an underwater bubbling circuit and by variable flow drivers. There is little evidence to support one form of CPAP delivery over another, a conclusion reached by Cochrane review in 2008 (De Paoli et al. 2008). There are reports that CPAP from variable flow circuits may be superior to CPAP via a ventilator (Pandit et al. 2001; Huckstadt et al. 2003; Courtney et al. 2001) with increased tidal volume, improved thoraco-abdominal synchrony (Boumecid et al. 2007), more stable airway pressure and decreased work of breathing (Moa et al. 1988). However, other studies have not found any differences in respiratory rate, heart rate, blood pressure or comfort levels between the devices (Ahluwalia et al. 1998) nor any difference in rates of extubation failure (Stefanescu et al. 2003).
Studies that have compared ventilator generated CPAP with underwater bubbling CPAP have also seen mixed results. Animal studies showed improved airway patency, higher pH and improved oxygenation in bubble circuits compared with ventilator CPAP (Pillow et al. 2007), while another study described more stable pressure at the prong during ventilator CPAP (Kahn et al. 2007). There has been debate about whether bubble CPAP is superior to ventilator CPAP due to oscillations in the delivered pressure caused by the bubbling (Lee et al. 1998), but it appears that vigorous bubbling is no better than gentle bubbling (Morley et al. 2005) and the oscillations are dramatically attenuated on reaching the small airways (Kahn et al. 2007). One clinical study that attempted to compare ventilator with bubble CPAP found reduced minute volume, but also reduced respiratory rates in the bubble CPAP group with no difference in blood gases (Lee et al. 1998).
Studies have also compared variable flow CPAP with bubble CPAP. One group found that bubble CPAP was not as good as variable flow CPAP at improving work of breathing and thoraco-abdominal synchrony (Liptsen et al. 2005), and another group found infants treated with bubble CPAP had higher oxygen requirements and respiratory rates (Mazzella et al. 2001). A third, more recent study determined that bubble CPAP was equally as effective as variable flow in preventing extubation failure and was more effective in infants who had been ventilated for longer (Gupta et al. 2009). Clinically important outcomes of different CPAP devices require further evaluation in randomised trials.
47.2.1.6.4.2 Nasal Interface During CPAP
CPAP was originally described using either an endotracheal tube or various head chambers and masks. These were associated with severe side effects and are no longer used. Endotracheal CPAP has been shown to increase work of breathing (Kim 1989; Davis and Henderson-Smart 2001; LeSouef et al. 1984), and CPAP is now delivered via a variety of short and long, single and bi-nasal prongs, or by nasal mask.
Long nasopharyngeal tubes, passed through one nostril to sit above the epiglottis, are still used but have high intrinsic resistance, and therefore a significant amount of the distending pressure is lost along the tube, sometimes more than 4 cm H2O (De Paoli et al. 2002). Shorter single nasal prongs can be used but also have high resistance, and pressure is also lost via the contralateral nostril. Short bi-nasal prongs, of which there are several designs, provide a low resistance interface (De Paoli et al. 2002). Their use has been shown to prevent more re-intubations than single nasal or nasopharyngeal prongs (relative risk (RR) 0.59, 95 % CI 0.41, 0.85, number needed to treat (NNT) was 5) (De Paoli et al. 2008). Small nasal masks have also been developed, initially in the belief that they caused less trauma. There is minimal data regarding their use, efficacy or safety, and a recent study showed that mask CPAP caused as much nasal trauma as bi-nasal prongs (Yong et al. 2005), albeit at different sites. The use of nasal masks needs to be properly investigated.
47.2.1.6.4.3 Indications for CPAP: Delivery Room and Early CPAP
In much of the developed world, management of very preterm infants in the delivery room has included endotracheal intubation and early surfactant treatment. However, a series of observational studies suggested that preterm infants managed well with initial CPAP support, reducing intubation and BPD rates, without increasing mortality or morbidity (Jacobsen et al. 1993; De Klerk and De Klerk 2001; Kamper et al. 1993; Van Marter et al. 2000). Following these publications CPAP gained more credibility as a first-line treatment and was extensively used in very low birth weight infants (Finer et al. 2004; Ammari et al. 2005). Starting CPAP soon after birth not only avoids endotracheal intubation and its inherent risks (O’Donnell et al. 2006) but also delays any surfactant treatment (Stevens et al. 2007). RCTs and meta-analyses of premature infants managed with early CPAP compared with intubation and ventilation had failed to detect differences between groups (Han et al. 1987; Sandri et al. 2004; Subramaniam et al. 2005). One study did find lower rates of BPD in infants treated with early CPAP, but the group had also received a sustained inflation at stabilisation which may have affected the results (te Pas and Walther 2007).
The COIN trial randomised infants less than 28 weeks of gestation to either CPAP or intubation in the delivery room (Morley et al. 2008). This trial found that half of the infants in the CPAP group never required intubation. CPAP-treated infants had a significantly lower rate of death or BPD at 28 days, but not at 36 weeks corrected age. CPAP-treated infants also had a higher rate of pneumothorax, but no differences were found in any other adverse outcomes. From this large RCT, it would appear that CPAP is an acceptable alternative to intubation in the delivery room as many small babies who breathe spontaneously at birth were successfully treated without mechanical ventilation. It is possible that the higher pneumothorax rate in the CPAP group was due to surfactant deficiency. The challenge is not only to look at ways to support infants with CPAP but also to replace surfactant in a timely manner if necessary (Hascoet et al. 2008).
47.2.1.6.4.4 Indication for CPAP: Post-extubation
As lung protective strategies have evolved, premature infants are being extubated earlier. Premature infants will have ongoing lung disease (Fox et al. 1981), poor thoraco-abdominal wall co-ordination (Locke et al. 1991) and apnoea of prematurity (Kattwinkel et al. 1975). They can develop progressive atelectasis (Finer et al. 1979) and many do not manage without ventilation for long (Annibale et al. 1994; Davis and Henderson-Smart 2000; Higgins et al. 1991). Systematic review of nine trials randomising infants to CPAP or head box oxygen post-extubation showed reduced need for additional respiratory support in the CPAP group (RR 0.62 95 % CI 0.51, 0.76, with NNT 6) (Davis and Henderson-Smart 2003). No difference was seen in terms of BPD. In these studies many infants in the head box oxygen group were successfully ‘rescued’ with CPAP treatment, and as a result the review found no difference in re-intubation rates. Extubation to CPAP was only advantageous if CPAP pressures were at least 5 cm H2O. The review concluded that CPAP is beneficial post-extubation, but if resources are limited, there is no harm in restricting CPAP use after extubation to those infants who are unable to manage in head box oxygen alone. Current European guidelines recommend that preterm infants should be placed on CPAP following extubation (Sweet et al. 2007).
47.2.1.6.4.5 Optimal CPAP Pressure
Deciding optimal CPAP pressure with which to treat infants is difficult. Animal data suggests that alveolar-arterial gradient falls with increasing PEEP, up to 8 cm H2O (Probyn et al. 2004). Human data shows increasing FRC and tidal volume, with decreasing respiratory rate and thoraco-abdominal asynchrony, as PEEP increases from 0 to 8 cm H2O (Elgellab et al. 2001). Laboratory data demonstrated that different prong systems result in the loss of several centimetres of water pressure across the prongs (De Paoli et al. 2002), and other studies have shown that further pressure loss occurs between the prong and the pharynx (De Paoli et al. 2005). There is much to learn about optimal CPAP pressures, and it is unlikely that any single pressure will be appropriate for the duration of an infant’s illness. It would be more realistic to titrate CPAP pressure against severity of the lung disease at a given time (Davis et al. 2009).
47.2.1.6.4.6 CPAP Complications
Success of CPAP support is dependent on training and experience of both medical and nursing staff. Clinical skills in delivering CPAP support increase with time (Aly et al. 2004). The aim of CPAP is to pressurise the infants nasopharynx and lungs, but nasal prong fit is inexact and gas leak from the mouth and nose means that delivered pressure may be lower than intended (Kahn et al. 2007). Optimal prong size, position, angle and strapping all affect pressure delivery. Chin strapping may be used to reduce leak, but there is no evidence that this increases the delivered pressure. It can be difficult to achieve a therapeutic distending pressure in some infants, resulting in failure of CPAP treatment.
Gastric distension is a well-recognised side effect of CPAP although CPAP does not appear to increase the risk of necrotising enterocolitis (Aly et al. 2009) and may actually increase the speed of gastric emptying (Gounaris et al. 2004). Standard practice includes insertion of a gastric tube that is left open to air, with the aim of venting the stomach, although there is no evidence that this occurs. Nasal trauma has been reported in up to 20 % of infants receiving nasal CPAP (Robertson et al. 1996). Similar rates of injury between nasal prongs, masks and nasopharyngeal tubes have been reported (Yong et al. 2005; Buettiker et al. 2004). Duration of CPAP support has so far been shown to be the strongest risk factor for traumatic injury (Yong et al. 2005). Early RCTs of CPAP report increased rates of pneumothoraces (Ho et al. 2002) and recent trials have shown similar rates (Morley et al. 2008; Sandri et al. 2009). Several case reports exist of more unusual complications including pneumopericardium (Turkbay et al. 2007), pulmonary interstitial emphysema (Arioni et al. 2006) and ingested nasal tubes (Duran et al. 2005). There is some data to suggest that CPAP increases infection rates, possibly secondary to trauma to the nasal mucosa (Ronnestad et al. 2005).
47.2.1.6.5 INSURE Technique
Increasing numbers of preterm infants are managed with CPAP support from birth, but concerns remain about pneumothorax rates and the delay in any surfactant treatment required. Clinicians have become interested in a technique that incorporates a brief period of intubation, to administer surfactant, followed by rapid extubation to CPAP which may overcome these problems. The technique has become known as INSURE (intubation-surfactant-extubation), and several studies have tested this method against standard ventilation techniques (Blennow et al. 1999; Bohlin et al. 2007; Thomson 2002; Verder et al. 1999).
Systematic review has shown that in infants at high risk of early RDS, early prophylactic surfactant in the first 2 h of life is better than later selective surfactant use with respect to BPD, death and air leak (Soll and Morley 2001). It has also been reported that quick intubation for surfactant delivery was most efficacious when done early (Blennow et al. 1999; Bohlin et al. 2007) with improved oxygen, less mechanical ventilation and less BPD (Thomson 2002; Verder et al. 1999; Verder 2007).
Meta-analysis of six INSURE papers (Stevens et al. 2007) has shown reduction in BPD in the INSURE group, compared with traditional treatment of surfactant and ongoing ventilation (RR 0.51 95 % CI 0.26, 0.99). The review also found that INSURE-treated infants had less need for mechanical ventilation (RR 0.67, 95 % CI 0.57, 0.79) and fewer air leaks (RR 0.52, 95 % CI 0.28, 0.96) but had an increase in surfactant use. Stratified analysis, by oxygen requirement at study entry, found that a lower threshold of intervention, at an inspired oxygen below 45 %, resulted in lower rates of pneumothorax (RR 0.46, 95 % CI 0.23, 0.93) and less BPD (RR 0.43, 95 % CI 0.20, 0.92). Higher thresholds were associated with higher rates of patent ductus arteriosus (RR 2.15, 95 % CI 1.09, 4.13). Further studies comparing INSURE with ongoing ventilation, published since the meta-analysis, have added further weight to its findings (Rojas et al. 2009). The REVE trial also compared the INSURE technique with ongoing ventilation post-surfactant treatment, and the results suggest that the technique has most benefit for the youngest infants at 25–26 weeks gestation (Truffert et al. 2008).
The technique may not be risk-free; it still requires intubation which has inherent risks, and data suggest that INSURE results in a period of depressed brain activity (van de Berg et al. 2010). These studies have not answered the question of whether it is better to treat infants with the INSURE technique or to treat with CPAP alone and give rescue surfactant, via brief intubation, only if CPAP support is insufficient. One small Scandinavian study has addressed this question and found that the INSURE group had better oxygenation and reduced need for mechanical ventilation (Verder et al. 1994) compared with the CPAP and rescue surfactant group. The large multicentre CURPAP study also aimed to answer this question (Sandri et al. 2008), and the presented results show that there were no differences between groups in the need for mechanical ventilation, or for the combined outcome of death or BPD (Sandri et al. 2009). The implication for clinicians is that CPAP with rescue surfactant was no worse than prophylactic surfactant followed by CPAP support. There is a need to individualise initial CPAP support with early rescue surfactant based on clinical criteria. The Vermont-Oxford Network is now running a three-armed trial comparing traditional intubation, surfactant and ongoing ventilation with either INSURE or CPAP and rescue surfactant (Sinha et al. 2008).
47.2.1.6.6 High-Flow Humidified Nasal Cannula Oxygen Delivery
High-flow nasal cannulae deliver gas at 2–8 L/min into the nose, via small prongs which are loose fitting in the nostrils. The technique has evolved from subnasal oxygen treatment at low flows, less than 2 L/min, as clinicians have attempted to support more infants without using traditional CPAP. The use of humidified high-flow systems has increased rapidly over the last few years, particularly as it is felt that the system is easier to use (Shoemaker et al. 2007) and provides more patient comfort.
Traditional CPAP delivery has disadvantages using of tight-fitting head wraps, the need for careful positioning, compression of the nose and nasal trauma, and it is sometimes poorly tolerated by the infant. The use of small cannulae to generate positive pressure could reduce many of these issues; however, early equipment, developed from the original low-flow systems, were poorly heated and humidified. This limited their use due to risk of nasal mucosa injury, mucosal bleeding, thickened secretions and nosocomial infection (Kopelman and Holbert 2003; Woodhead et al. 2006). The development of heated humidified high-flow gas delivery via nasal cannulae (HHHFNC) may circumvent these issues. Such circuits are reported to decrease work of breathing and prevent re-intubation more effectively than high flow from a standard, non-heated, non-humidified nasal cannula (Woodhead et al. 2006).
Studies have shown that HHHFNC, at relatively low flows of 1–2 L/min, can generate a positive pressure in the airway of preterm infants (Sreenan et al. 2001); however, HHHFNC does not currently allow the measurement of delivered pressure, without a separate invasive process such as an oesophageal pressure probe. Some data exist suggesting that HHHFNC does not produce excessive distending pressures (Kubicka et al. 2008; Saslow et al. 2006) and that very high flows would be needed to generate significant positive pressure. Other data has demonstrated high and variable delivered pressures (Shoemaker et al. 2007; Campbell et al. 2006), and reports exist that demonstrate potentially hazardous pressures, especially in very small infants (Sreenan et al. 2001; Quinteros et al. 2009; Chang et al. 2005).
Specific gas flow to obtain a certain delivered pressure is unknown; the pressure generated in the pharynx will depend on leak at the nose (Lampland et al. 2009), which in turn depends on the size of the patients nostril, and the presence of any secretions sealing the nares. Some algorithms exist to guide flow selection, but they depend on a consistent level of leak being present, which is not necessarily the case in practice (Wilkinson et al. 2008). If the infant’s mouth is closed and the cannulae become functionally ‘sealed’ in the nares due to secretions or tight-fitting cannulae, then flow will continue to increase the nasopharyngeal pressure until an outlet is found. This could result in significant lung and gastrointestinal overdistention. A recent report describes development of subcutaneous scalp emphysema, pneumo-orbitis and pneumocephalus during HHHFNC use (Jasin et al. 2008). Not all HHHFNC systems contain a pressure-limiting safety valve to protect against inadvertent high pressure, but such a system should be incorporated into future designs (Lampland et al. 2009). One further concern with HHHFNC has been adequate humidification and heating of the circuit. Anecdotal reports exist of condensation in the tubing and cannulae during flows at the lower end of the range of ‘high flow’, resulting in water droplets coalescing to obstruct flow or enter the nares.
Initial studies with ‘high-flow’ systems showed disadvantages when compared with CPAP (Campbell et al. 2006); however, partial humidification and relatively low flows were used. More recent studies have found work of breathing and lung compliance were improved during HHHFNC compared with CPAP (Saslow et al. 2006); ventilator days were decreased without adverse effects such as air leak, intraventricular haemorrhage, nosocomial infection or BPD (Shoemaker et al. 2007); and frequency and severity of apnoea and bradycardia were reduced (Shoemaker et al. 2007; Woodhead et al. 2006; Sreenan et al. 2001; Holleman-Duray et al. 2007).
It is possible that the jet of gas delivered in HHHFNC may penetrate the nasal dead space very efficiently. As the nasal compartment contributes up to 50 % of the overall respiratory resistance (Hall et al. 2002), this effect could contribute to a reduced work of breathing compared with conventional CPAP prongs. The uptake of HHHFNC by numerous neonatal units has not been accompanied by obvious changes in neonatal outcome, but the technique has not been systematically studied. The American Association of Respiratory Care 2002 Clinical Practice Guideline (Myers 2002) states that flow for nasal cannula treatment in newborn infants should not exceed 2 L/min and acknowledges that even this flow may be excessive for the extremely low birth weight infant. There is a need for high-quality RCTs to delineate the range of delivered pressure for a given flow, for all sizes of preterm infants. Until the results of these trials are available, if an infant requires CPAP, then it can more safely be delivered with a standard device (Davis et al. 2009; So et al. 1992). A multicentre, prospective, randomised comparison of CPAP compared with HHHFNC in infants greater than 1,000 g and 28 weeks gestation, from birth or following extubation, is currently underway.
47.2.1.6.7 Non-invasive Ventilation: Nasal Intermittent Positive Pressure Ventilation (NIPPV)
NIPPV includes modes of non-invasive ventilation, characterised by CPAP augmented with mechanical inflations to a set pressure. The peak (PIP) and end-expiratory pressures, inflation rate and time can all be manipulated during NIPPV. Terminology used to describe NIPPV is varied, reflecting the different inflation strategies applied through the nasal interface. Terms include synchronised nasal intermittent positive pressure ventilation (SNIPPV) (Aghai et al. 2006; Bhandari et al. 2007; Kulkarni et al. 2006; Santin et al. 2004), nasopharyngeal-synchronised intermittent mandatory ventilation (NP-SIMV) (Friedlich et al. 1999), nasal synchronised intermittent mandatory ventilation (N-SIMV) (Kiciman et al. 1998), nasal synchronised intermittent positive pressure ventilation (nSIPPV) (Moretti et al. 1999), nasal intermittent mandatory ventilation (NIMV) (Kugelman et al. 2007) and non-invasive pressure support ventilation (NI-PSV) (Ali et al. 2007). Nasal bi-level positive airway pressure (N-BiPAP) (Migliori et al. 2005) is also used but may be more indicative of a technique using a narrow PIP-PEEP pressure difference, long inspiratory times and low rates, during which the infant continues to breathe undisturbed.
47.2.1.6.7.1 Evolution of NIPPV
NIPPV has emerged concurrently with the drive toward minimal ventilation and lung protective strategies of respiratory support. As many as half of very low birth weight infants ‘fail’ initial CPAP support (Finer et al. 2004; Morley et al. 2008), requiring intubation and ventilation, and around a third ‘fail’ extubation to CPAP (Annibale et al. 1994; Higgins et al. 1991; Davis and Henderson-Smart 2003). Efforts to manage more small infants without invasive ventilation prompted the investigation and use of NIPPV. Neonatal NIPPV uses nasal prongs or masks, with variable leak via the mouth and nose, and usually no trigger for synchronisation. A survey of neonatal units in the UK in 2006 (Owen et al. 2008) showed that 48 % of regional nurseries were using NIPPV.
The mechanism of action of NIPPV remains unclear. Hypotheses include pharyngeal dilation and increased pharyngeal pressure (Aghai et al. 2006; Santin et al. 2004; Friedlich et al. 1999; Moretti et al. 1999; Khalaf et al. 2001) increased sighs and improved respiratory drive (Lin et al. 1998), induction of Head’s paradoxical reflex (Ryan et al. 1989), increased mean airway pressure (Davis et al. 2001) increased alveolar recruitment (Khalaf et al. 2001; Courtney and Barrington 2007), increased functional residual capacity (FRC) and increased tidal and minute volume (Moretti et al. 1999). It is unclear whether mechanical inflations during NIPPV are transmitted to the chest. There is some evidence that NIPPV, compared with CPAP, improves arterial oxygen, carbon dioxide, respiratory rates and oxygen saturations (Moretti et al. 1999; Migliori et al. 2005), reduces thoraco-abdominal asynchrony (Kiciman et al. 1998) and decreases work of breathing (Aghai et al. 2006; Ali et al. 2007). NIPPV may increase tidal volumes and minute ventilation (Moretti et al. 1999), although this finding is not consistent (Aghai et al. 2006; Ali et al. 2007).
47.2.1.6.7.2 NIPPV Delivery
NIPPV may be generated by a ventilator or specialised CPAP driver and may be delivered by nasal or nasopharyngeal prongs or by nasal mask. No studies have compared efficacy of nasal interface for NIPPV delivery. Most NIPPV delivery systems do not allow the mechanical inflations to be synchronised with spontaneous inspiration. Abdominal pneumatic capsules have been used to attempt to synchronise inflations, but their efficacy during NIPPV has not been investigated.
We do not know the optimal inflation settings in terms of PIP, PEEP, inflation rate or time for NIPPV, and these values have varied widely in published studies. The 2006 UK survey noted that the settings used by clinicians were very variable (Owen et al. 2008). No studies have investigated weaning strategies for NIPPV.
47.2.1.6.7.3 Indications for NIPPV Use
Meta-analysis of three studies (Friedlich et al. 1999; Khalaf et al. 2001; Barrington et al. 2001) comparing NIPPV with CPAP following extubation found a significant risk reduction for extubation failure (RR 0.21, 95 % CI 0.1, 0.45, NNT 3) in the NIPPV group (Davis et al. 2001). Recent studies of NIPPV post-extubation have confirmed this finding (Khorana et al. 2008; Sai Sunil Kishore et al. 2009). Meta-analysis of two studies (Lin et al. 1998; Ryan et al. 1989) comparing NIPPV with CPAP for the treatment of apnoea showed no advantage of NIPPV over CPAP (Davis et al. 2001). Some studies have now investigated the use of NIPPV for the initial treatment of respiratory disease and found reduced rates of endotracheal intubation in the NIPPV groups (Kugelman et al. 2007; Bisceglia et al. 2007). There is emerging evidence that NIPPV, when compared with ventilation (Bhandari et al. 2007) or with CPAP (Kulkarni et al. 2006; Kugelman et al. 2007), has reduced rates of BPD. Retrospective review of NIPPV-treated infants, compared with ventilated infants, shows that the smallest babies had better outcomes with respect to BPD, death and neurodevelopmental outcome at 18–22 months (Bhandari et al. 2009). A large multicentre trial of NIPPV as a first-line treatment is now taking place (Kirpalani 2007).
47.2.1.6.7.4 NIPPV Complications
Complications similar to those seen in CPAP-treated infants are the most likely to occur, including trauma, laceration (Yong et al. 2005; Shanmugananda and Rawal 2007) and sepsis (Graham et al. 2006). Historically gastrointestinal perforations (Garland et al. 1985) and head moulding (Pape et al. 1976) were reported following NIPPV, but these have not been described in recent studies. Abdominal distension has been reported in one NIPPV study (Jackson et al. 2003), but it has also been suggested that the reduced work of breathing seen during NIPPV may reduce gastrointestinal complications (Aghai et al. 2006).
47.2.1.6.7.5 Future Directions for NIPPV
There is no evidence regarding the best device, interface, settings or weaning, nor whether synchronised NIPPV is more advantageous compared with non-synchronised NIPPV. These areas warrant further investigation to delineate how NIPPV is most beneficial (Owen et al. 2007).
47.2.1.6.8 Ventilation
Neonatal endotracheal intubation and ventilation emerged in the 1960s, and although many infants survived due to this intervention (Henderson-Smart et al. 2002), it quickly became apparent that ventilation had inherent risks: ventilator-induced lung injury (Dreyfuss and Saumon 1998), infection, development of BPD (Avery et al. 1987; Heimler et al. 1988; Pandya and Kotecha 2001) and upper airway problems. While there is now considerable debate about which preterm infants need mechanical ventilation, there have also been dramatic changes in the way neonatologists are able to deliver mechanical ventilation. The British Association of Perinatal Medicine (BAPM) suggests that infants have failed CPAP support and require ventilation if they have persistent or major apnoeas with bradycardia, become acidotic below pH 7.25 or require more than 60 % oxygen (British Association of Perinatal Medicine T 2005).
47.2.1.6.8.1 Conventional Ventilation
Early neonatal ventilation was time cycled, was pressure limited and was not synchronised with spontaneous respiratory effort (continuous mandatory ventilation (CMV), referred to as conventional ventilation). It was however demonstrated that CMV, at inflation rates similar to the infant’s own respiratory rate, could result in synchronous breathing (Greenough et al. 1983, 1987).
47.2.1.6.8.2 Triggered Ventilation
Technology now allows synchronisation of mechanical inflations with spontaneous inspiration. Success of this technique relies on the triggering device being highly sensitive, with minimal time delay. Several types of trigger have been devised, using changes in airway pressure, airway flow, transthoracic impedance and abdominal movement. Different triggers may work differently under varying respiratory conditions and movements (Kassim and Greenough 2006); flow triggers have been shown to be superior to pressure triggers (Dimitriou et al. 2001). Triggered ventilatory modes, when compared with conventional CMV, show reduced rates of air leak and shorter duration of ventilation, when started during the recovery phase of RDS (Greenough et al. 2008). They also achieve improved blood gases, more stable blood pressure and reduced work of breathing (Cleary et al. 1995). Triggered modes have not been shown to be advantageous over conventional CMV in terms of intraventricular haemorrhage (IVH), BPD or mortality (Greenough et al. 2008). Some triggered ventilation modes support all spontaneous inspirations (e.g. assist control (AC), synchronised intermittent positive pressure ventilation (SIPPV) or patient-triggered ventilation (PTV)). Other modes support only a set number of inspirations (e.g. synchronised intermittent mechanical ventilation (SIMV)), determined by the clinician. Small RCTs have suggested that supporting all inflations is superior to supporting a limited number and that low numbers of supported breaths, less than 20/min, actually increase work of breathing (Roze et al. 1995).
47.2.1.6.8.3 Volume-Targeted Ventilation (VTV)
Until recently, it had not been possible to measure tidal and minute volumes in neonates, but as devices have been developed that can make these tiny measurements, volume-targeted neonatal ventilation has emerged. There is good animal and adult evidence to suggest that controlling tidal volume can reduce volutrauma, atelectotrauma and BPD in low birth weight infants (Van Marter et al. 2000). Volume-targeted ventilation allows gas exchange at lower peak inflation pressures in both the early and recovery phases of RDS (Cheema and Ahluwalia 2001). VTV shows more consistent tidal volume delivery, fewer very large breaths and less inflammatory cytokine response (Keszler 2005). Meta-analysis of volume-targeted ventilation, compared with pressure-limited ventilation, shows lower pneumothorax and IVH rates, but no definite effect on BPD or mortality rates (McCallion et al. 2005). Long-term follow-up of infants managed with VTV, compared with pressure-limited ventilation, showed no differences in mortality, respiratory illnesses or readmissions. The volume-targeted group had lower rates of inhaled steroid and bronchodilator use (Singh et al. 2009a).
47.2.1.6.8.4 Newer Modes of Conventional Ventilation
It is possible to synchronise the end of inspiration as well as the start, such that the infant is able to determine their own inspiratory time (sometimes called flow termination, e.g. pressure support ventilation, PSV, from the Dräger Babylog ventilator). Data evaluating this mode of support suggests that the technique is associated with lower rates of asynchrony (Dimitriou et al. 1998). Pressure support ventilation combined with volume-targeted ventilation has had mixed results; there appears to be reduced inflammation compared with pressure-limited ventilation (Lista et al. 2004), whereas another study found no benefit (Nafday et al. 2005). One study found infants on PSV with volume targeting required higher mean airway pressures than those managed with SIMV (Olsen et al. 2002).
Many other modes exist, such as pressure-regulated volume-controlled ventilation (PRVC from the Servo-i ventilator); this mode combines pressure and volume control. Tidal volume and maximum pressure are set, and the ventilator uses decelerating variable flow to achieve the target tidal volume. Two RCTs using PRVC in preterm infants have been published. One demonstrated reduced grade III and IV IVH in the PRVC group, compared with CMV. In a subgroup of infants less than 1,000 g, they demonstrated shorter duration of ventilation in the PRVC group (median of 11 vs. 19 days) (Piotrowski et al. 1997). The second trial found no differences when compared with SIMV (D’Angio et al. 2005).
Volume-assured pressure support ventilation (VAPS from the VIP Bird Gold ventilator) is another form of hybrid pressure and volume-controlled ventilation, where adjustment of pressure and inspiratory time occurs within each breath, to achieve the desired volume. No studies have evaluated this mode in infants with RDS.
Proportional-assist ventilation (PAV) allows even more patient control. The infant controls the timing, frequency and magnitude of inflations, and the waveform is tailored to compensate for changes in compliance and resistance. This method of support reduces work of breathing (Schulze et al. 1996) and may allow ventilation at lower mean airway pressures (Schulze et al. 1999) with less thoraco-abdominal asynchrony (Musante et al. 2001), but infants can have longer desaturations compared with PTV and require conventional back-up inflations for periods of apnoea (Schulze et al. 2007).
Neurally adjusted ventilatory assist (NAVA) uses the electrical activity of the diaphragm to control the ventilator (Sinderby et al. 1999), and electrodes are embedded onto a gastric tube positioned in the lower oesophagus. The electrical signal triggers ventilator inflation, drives inflation pressure proportional to the respiratory effort and ceases at end inspiration. One study examining seven low birth weight infants with this technique showed improved infant-ventilator interaction and lower respiratory rates during NAVA, when compared with conventional ventilation (Beck et al. 2009).
There have been many reviews of the evidence regarding respiratory management of infants with RDS published over the past decade (Sinha et al. 2008; Sweet et al. 2007; Hascoet et al. 2008; van Kaam and Rimensberger 2007; Ambalavanan and Carlo 2006; Bancalari and del Moral 2001; Claure and Bancalari 2008; Greenough and Sharma 2005; Hummler and Schulze 2009; Ramanathan 2008; Ramanathan and Sardesai 2008; Sinha and Donn 2008); however, scientific evidence does not necessarily translate into clinical practice. A survey carried out in 2006 in the UK showed that 73 % of neonatal units chose conventional non-synchronised ventilation (CMV) as the first line of support in preterm infants with RDS. Two per cent chose CPAP as first line, 2 % chose high-frequency ventilation and 5 % chose volume-targeted ventilation (Henderson-Smart et al. 2007), and only a quarter of NICUs were able to measure tidal volumes during ventilation.
47.2.1.6.9 High-Frequency Oscillatory Ventilation (HFOV)
Early animal work investigating HFOV demonstrated that there was more lung damage with the high magnitude pressure changes used in conventional ventilation than with the high mean airway pressure (MAP) used in HFOV (Hamilton et al. 1983). Animal data has shown less protein leak in RDS when using HFOV, compared with conventional ventilation (Niblett et al. 1989). Initial trials of HFOV used low lung volume strategies. This technique may be ideal for infants with established air leak syndromes, but when infants with RDS were studied, no pulmonary benefits were found with HFOV, and higher rates of IVH were seen (The HIFI Study Group 1989). Many of the infants enrolled in the early studies would not have had continuous carbon dioxide monitoring and may have had undetected hypocarbia contributing to the poor outcomes seen (The HIFI Study Group 1989; Greisen et al. 1987; Froese and Kinsella 2005). Further animal data demonstrated that optimising lung volume prolonged the effect of exogenous surfactant (Froese et al. 1993) and that when starting HFOV it was important to fully recruit the lung using a short period of higher airway pressure. A brief period of overdistension is less damaging than the persistent atelectasis seen in the low-volume approach (Bond and Froese 1993), and the open lung technique results in more even distribution of tidal volume and less alveolar overdistention (Frerichs et al. 2003). Froese et al. suggested that how the HFOV technique is applied is more important than the choice of mechanical device generating the oscillations (Froese and Kinsella 2005).
The next wave of clinical trials used high lung volume strategies, where clinicians reduced inspired oxygen before reducing the MAP. Acute and chronic pulmonary advantages of HFOV were then seen compared with conventional ventilation (Gerstmann et al. 1996). However, the results were not reproduced in later trials where all the infants received steroids, exogenous surfactant and early CPAP after delivery (Thome et al. 1999), all of which result in a more open lung ventilation technique in both groups. Improvements in conventional ventilation, increasing PEEP, decreasing tidal volume and synchronising inflations, have meant that the advantages of HFOV have been greatly reduced (Courtney et al. 2002). Now the pulmonary benefits of lower BPD rates and shorter duration of ventilation are only seen in infants with the most severe disease, who require high oxygen requirements (>60 %) post surfactant (Courtney et al. 2002). Routine HFOV for all RDS has not been shown to be beneficial and is now often reserved for the subset of infants with severe disease. The BAPM guidelines suggest conversion to HFOV, from conventional ventilation, for infants who have failed to respond to surfactant therapy and optimisation of conventional ventilation and who still have an oxygen requirement above 60 % and peak pressures above 30 cm H2O (British Association of Perinatal Medicine T 2005).
A Cochrane review has concluded that there is no clear evidence that prophylactic HFOV offers important advantages over conventional ventilation, in treating premature infants with RDS. There may be a small reduction in the rate of BPD, but the evidence is weak; future HFOV trials should focus on infants who are at the highest risk of BPD (Henderson-Smart et al. 2007). It is still to be determined whether a conventional ventilation strategy that aims to minimise volutrauma and atelectotrauma by using open lung ventilation, low tidal volumes and high PEEP is any different from HFOV (van Kaam and Rimensberger 2007).
There has been one study examining the application of high-frequency oscillations via nasal prongs showing improved PaCO2 and pH, compared with standard CPAP (Colaizy et al. 2008); further investigation of this method may be warranted.
47.2.1.6.10 High-Frequency Jet Ventilation (HFJV)
This mode of ventilation is a modification of HFOV that delivers very short inflation times of 0.02 s via a small bore injector cannula, in the frequency range of about 4–8 Hz. HFJV is not routinely used for infants with RDS. One study demonstrated that HFJV reduced rates of BPD in preterm infants, compared with conventional ventilation (Keszler et al. 1997), but a second study was stopped early due to higher rates of IVH seen in the HFJV group (Wiswell et al. 1996).
47.2.1.6.11 Extracorporeal Membrane Oxygenation (ECMO)
ECMO describes the use of modified cardiopulmonary bypass for patients with reversible lung disease, in whom maximal standard therapy has failed. It has become accepted for the treatment of several neonatal conditions, allowing time for lung healing. Catheter size and the need for systemic anticoagulation means that the technique is usually limited to infants greater than 2 kg in weight and more than 34 weeks gestation (Revenis et al. 1992). This excludes the majority of infants likely to have severe RDS. Infants at lower gestations have reduced survival (Hirschl et al. 1993) and a significantly increased risk of IVH (Hardart and Fackler 1999). IVH is four times more likely at 34 weeks gestation than at term (Neonatal ECMO Registry of the Extracorporeal Life Support Organisation 2004). Mature infants with life-threatening RDS show benefit from ECMO treatment with survival rates of more than 80 % (Bahrami and Van Meurs 2005).
47.2.1.6.12 Partial Liquid Ventilation (PLV)
PLV involves instilling perfluorocarbon into the lungs; perfluorocarbon is capable of gas transport, and during PLV the volume of liquid instilled replaces FRC. Conventional gas ventilation is applied in addition. PLV has been shown to reduce lung injury in animal models, but there is limited data in preterm infants with RDS (Ambalavanan and Carlo 2006). One non-randomised study showed a higher than expected rate of survival in infants with severe RDS, in whom conventional treatment was failing (Leach et al. 1996).
47.2.1.6.13 Weaning from Respiratory Support
Stepping down from mechanical ventilation is a topic of as much interest as escalation of support; however, there is very little research into the best practice of weaning. There is some evidence to suggest that the AC mode of ventilation is superior to SIMV modes for weaning (Dimitriou et al. 1995; Chan and Greenough 1994), as low SIMV rates can increase oxygen consumption and increase work of breathing (Roze et al. 1995). However, a survey of UK practice in 2006, more than a decade after this evidence was published, found that 73 % of neonatal units used SIMV mode for weaning infants from ventilation (Henderson-Smart et al. 2007). There have been several methods investigated to test whether an infant is ready for extubation, the key factors being an infant’s respiratory drive and their lung compliance.
Use of CPAP following extubation has been shown to be superior to head box oxygen, if the CPAP pressure is at least 5 cm H2O (Davis and Henderson-Smart 2003). In addition, use of NIPPV has been shown to prevent more extubation failures than CPAP alone (Davis et al. 2001). Weaning from NIPPV has not been studied, and weaning from CPAP has been the subject of very few studies. One study suggests decreasing CPAP support to pressures of 4–5 cm H2O and then stopping (Singh et al. 2006); this is the alternative to ‘cycling’ the infant through increasing periods of time off CPAP. The ‘cycling’ method has not been shown to have any significant advantages and prolongs the time the infant spends on CPAP support (Soe et al. 2006).
47.2.1.6.14 Summary of Respiratory Support
Currently the data are not conclusive to support or refute either starting with ventilation and weaning quickly or starting with minimal support and only escalating care if the infant is not managing. Ideal ventilation delivers consistent tidal and minute volumes, responds quickly to changing demands and allows the infant to breathe at the lowest pressures with the least work of breathing. Further RCTs comparing different modalities, for specific clinical conditions, are required before any single mode can be justified as being superior to another.
47.2.1.7 Rationale for Using Adjunctive Therapies During CPAP or Mechanical Ventilation for RDS
47.2.1.7.1 Exogenous Surfactant
The introduction of surfactant replacement in the late 1980s reduced mortality due to RDS but left NICUs with the burden of survivors with BPD, as survival increased, so did the rate of BPD (Hintz et al. 2005). Debate continues today about the need for surfactant administration, which surfactant to use, the most appropriate timing for surfactant delivery, the best dose and optimal mode of surfactant delivery, to treat RDS and prevent BPD. Surfactant has been shown to decrease rates of pneumothorax by 30–65 % and decrease mortality by up to 40 % (Halliday 2005).
47.2.1.7.1.1 Structure and Function of Surfactant
Surfactant is a complex system of phospholipids – mainly dipalmitoyl phosphatidylcholine, neutral lipids, proteins and glycoproteins. Surfactant is produced and assembled in type 2 pneumocytes from 22 weeks of gestation onwards, and the number of type 2 pneumocytes increases throughout gestation. Surfactant is stored in the lamellar bodies of the pneumocytes and is later extruded into the air spaces. A healthy term infant has about ten times the pool of surfactant compared with a premature baby with RDS (Adams et al. 1970; Jackson et al. 1986).
The main effect of surfactant is reduction of surface tension; phosphatidylcholine produces a monolayer that reduces surface tension by about two-thirds. Other phospholipids, along with surfactant proteins, further reduce surface tension to almost zero (Veldhuizen et al. 1998). Surface tension is responsible for approximately two-thirds of the elastic recoil forces of the lung, so by reducing surface tension, the surfactant prevents the air spaces from collapsing at end expiration. The lowered surface tension also allows re-expansion of the terminal airways with less force. Maximum lung volumes are increased and lung expansion is more uniform. Exogenous surfactants can mimic the effects of natural surfactant, but it takes up to ten times the quantity of exogenous surfactant to generate the same effects as endogenous surfactant (Seidner et al. 1988; Ikegami et al. 1989).
47.2.1.7.1.2 Surfactant Preparations
Improved outcomes are seen with animal-derived surfactants (Soll and Blanco 2001) or surfactants containing additional proteins or peptides, rather than phospholipids alone (Moya et al. 2005). Studies have shown more improvements in FRC and compliance when using porcine-derived surfactant (poractant alfa – CurosurfTM) compared with synthetic surfactant (colfosceril – ExosurfTM) (Stenson et al. 1994) and when using bovine-derived surfactants beractant (SurvantaTM) (Cotton et al. 1993) or calfactant (InfasurfTM) (Onrust et al. 1999) compared with colfosceril. Although few studies have directly compared different animal-derived surfactants, there is some data to suggest a quicker improvement in oxygenation with poractant alfa (Speer et al. 1995; Ramanathan et al. 2004). Newer artificial surfactants are now emerging which contain an artificial peptide (sinapultide) similar to surfactant protein B (lucinactant – SurfaxinTM). Early data suggest that this product may be as good as animal-derived compounds (Moya et al. 2005, 2007).
47.2.1.7.1.3 Timing of First Surfactant Dose
Using surfactant prior to the onset RDS can reduce ventilator-induced lung injury (Halliday 2006; Donn and Sinha 2006). Prophylactic versus selective rescue surfactant has been shown to be superior in terms of mortality (OR 0.61 95 % CI 0.28, 0.77), BPD or death (OR 0.85 95 % CI 0.76, 0.95) and pneumothorax(OR 0.54, 95 % CI 0.42, 0.84) (Soll and Morley 2001). However, there has not been shown to be a difference in mortality depending on whether the dose is given prior to mechanical ventilation or following stabilisation (Kendig et al. 1998); there is no definite answer as to how early, early treatment should be (Soll and Morley 2001; Yost and Soll 2000). Currently data would suggest that there is not much difference between early CPAP with prophylactic surfactant via brief intubation, early CPAP and selective rescue surfactant, intubation with prophylactic surfactant or rescue endotracheal intubation and rescue surfactant (Thomson 2002).
47.2.1.7.1.4 Dose of Surfactant
The dose of surfactant recommended by most manufacturers is 100 mg/kg. Smaller doses have been shown to be less effective (Konishi et al. 1988; Halliday et al. 1993), and larger doses may have a quicker effect but confer no ongoing advantages (Halliday et al. 1993). Manufacturers recommend repeat doses at 12 h, but if there is severe disease with extensive protein leak, much of the second dose may be inactivated. Early delivery of the second dose in infants with high ventilatory or oxygen requirements may be more advantageous (Figueras-Aloy et al. 2001). A Cochrane review looking at single versus multiple doses of surfactant described two papers using animal-derived surfactants showing that multiple doses resulted in fewer pneumothoraces (RR 0.51, 95 % CI 0.30, 0.88) and a trend towards lower mortality (RR 0.63, 95 % CI 0.39, 1.02). They also described one study, using synthetic surfactant, that showed lower rates of necrotising enterocolitis (NEC) following multiple doses (RR 0.20, 95 % CI 0.08, 0.51) and lower mortality (RR 0.56, 95 % CI 0.39, 0.81). The review concluded that if an infant has ongoing respiratory insufficiency, then repeated doses of surfactant are beneficial (Soll and Ozek 2009). Studies have found no benefit in delivery of more than two doses of surfactant (The OSIRIS Collaborative Group 1992).
47.2.1.7.1.5 Mode of Surfactant Delivery
Almost all surfactant is given directly into the endotracheal tube as a bolus. There has not been shown to be any benefit in performing physical manoeuvres aiming to direct surfactant into different areas of the lungs (Zola et al. 1993). In the modern era of minimal ventilation, there is considerable interest in a technique of surfactant delivery that does not require intubation. Endotracheal intubation has inherent risks; it frequently takes longer than the recommended time to perform (O’Donnell et al. 2006) and is often not successful at the first attempt (Leone et al. 2005). There are reports of success using alternative delivery techniques. One group has reported using surfactant delivered via a small endotracheal catheter, under direct vision, and showed that the process was well tolerated and first attempt at administration was successful in 80 % (Kribs et al. 2008). This method is now the subject of a randomised controlled trial. Two groups have published studies of aerosolised surfactant delivery, which appears feasible and safe (Berggren et al. 2000; Jorch et al. 1997) but requires further study (Mazela et al. 2007), as animal data have suggested that drug distribution in the lungs may be very variable (Lewis et al. 1991). A recent report of aerosolised lucinactant (AerosurfTM) also appears feasible and safe (Finer et al. 2006). Another group has delivered surfactant via laryngeal masks (Trevisanuto et al. 2005); this is also now the subject of an RCT. Kattwinkel et al. used surfactant instilled into the pharynx prior to delivery of the body and reported that the method was simple and safe and warrants a randomised trial (Kattwinkel et al. 2004).
47.2.1.7.1.6 Adverse Events During Surfactant Delivery
Surfactant delivery is not without adverse effects. Infants can have transient hypoxia and bradycardia (Liechty et al. 1991) along with flattening of the EEG (electroencephalogram) (Hellstrom-Westas et al. 1992). A recent report demonstrated that the endotracheal tube is frequently obstructed following surfactant administration and infants exhibit increased ventilatory requirements for up to an hour following surfactant delivery (Wheeler et al. 2009).
47.2.1.7.1.7 Nonresponders to Surfactant
Lack of response to surfactant treatment may indicate persistent pulmonary hypertension, patent ductus arteriosus (PDA), air leak, shock, congenital infection or asphyxia (Wirbelauer and Speer 2009). In the absence of these confounding conditions, failure of response confers a worse prognosis (Skelton and Jeffery 1996; Kuint et al. 1994).
47.2.1.7.1.8 Surfactant Conclusion
Surfactant improves outcomes for small ventilated infants, but many of the trials investigating surfactant use were done in the pre-steroid era and general anaesthetic was routinely used for caesarean sections. The results, therefore, may not be so applicable to today’s population of preterm babies. In some infants who have received antenatal steroids, who are not affected by anaesthetic agents and who are supported with early CPAP, it is not clear whether exogenous surfactant is needed at all.
47.2.1.7.2 Inhaled Nitric Oxide
Nitric oxide is a potent pulmonary vasodilator and has been shown to have profound effects on gas exchange (Gaston et al. 1994). Its use improves ventilation-perfusion mismatching, allowing improved oxygenation and reduced ventilation. Inhaled nitric oxide has been shown to be beneficial in term infants with respiratory disease, but the results are less clear, and more variable, in infants below 34 weeks gestation (Van Meurs et al. 2005; Schreiber et al. 2003; Lindwall et al. 2005). There may be some short-term benefits, but no long-term advantages have been demonstrated in premature infants (Subhedar et al. 1997). Prophylactic low dose nitric oxide in preterm infants does not reduce the risk of developing BPD (Mercier et al. 2009). Concerns remain regarding the effects of the drug on the developing brain and possible risk of intracranial bleeding (Van Meurs et al. 2005).
47.2.1.7.3 Antibiotics
It is impossible to differentiate between RDS and severe postnatal, or congenital, infection. Blood cultures and antibiotic treatment, with a penicillin and an aminoglycoside, for 48 h until blood cultures are shown to be negative, are standard therapy for infants with presumed RDS.
47.2.1.7.4 Methylxanthines
Methylxanthines have proven benefit in treating apnoea of prematurity. A recent large RCT has shown improved survival without neurodevelopmental disability (Schmidt et al. 2007), reduced rates of BPD and shorter duration of respiratory support (Schmidt et al. 2006a) in infants treated with caffeine. These benefits would suggest that preterm infants with RDS, who may or may not develop apnoea of prematurity, could benefit from treatment with methylxanthines.
47.2.1.7.5 Heliox
Heliox is a gas mixture in which the nitrogen has been replaced with helium. This mixture decreases pulmonary resistance and resistive work of breathing. It is hypothesised that this might improve lung function and reduce energy expenditure in infants with severe lung disease. Early observational data show that mechanical ventilation with heliox mixture does reduce resistive work of breathing and ventilatory requirements, as well as improving gas exchange in ventilated preterm infants (Migliori et al. 2009). Other reports suggest it may be useful in the treatment of pulmonary interstitial emphysema (Phatak et al. 2008). Heliox treatment, combined with CPAP, for extremely low birth weight infants is currently being studied as part of a randomised trial.
47.2.1.7.6 Diuretics
Frusemide (furosemide) increases resorption of lung fluid and produces short-term improvements in lung function. However, the early use of diuretics in preterm infants can increase the risk of patent ductus arteriosus as frusemide stimulates production of prostaglandin E2. Repeated use of diuretics in premature infants increases the risk of ototoxicity and aminoglycoside ototoxicity (Hey Ee 2003), as well as the possibility of inducing hypovolaemia and low systemic blood pressure. Systematic review of diuretics for RDS shows no benefit on mortality, BPD, duration of mechanical ventilation, duration of oxygen treatment or length of hospital stay (Brion and Soll 2001). The trials included in the Cochrane review were completed before generalised use of antenatal steroids or surfactant replacement, but to date there is no evidence in favour of routine use of diuretic treatment in RDS (Wiswell et al. 2007). The use of diuretics should be reserved for oliguric infants with fluid retention and deteriorating lung function.
47.2.1.7.7 Analgesia, Sedation and Neuromuscular Paralysis
Opioids have regularly been used to provide analgesia and sedation for ventilated infants with RDS. Recent systematic review found no significant benefits in terms of mortality, duration of mechanical ventilation or neurodevelopmental outcomes to warrant routine use of opioids in this population (Bellu et al. 2005). Adverse effects of morphine, such as delaying achievement of full enteral feeds, need to be considered when considering opioid treatment (Menon et al. 2008). Midazolam is also commonly used for sedation of ventilated newborns, but again systematic review found no advantages when compared with either placebo or morphine. Midazolam use increased rates of adverse events including hypotension, death, longer duration of hospital stay, and more IVH and periventricular leukomalacia. The authors concluded that routine use of midazolam for sedation should not be recommended (Ng et al. 2003). Neuromuscular paralysing agents are sometimes used to abolish spontaneous breathing patterns in infants with asynchronous respiratory effort. Cochrane review has shown that agents such as pancuronium have the potential to decrease air leak and IVH in such infants. Uncertainty regarding the long-term pulmonary and neurological effects of paralysing agents means that routine usage is not currently recommended (Cools and Offringa 2005).
47.2.1.8 Classical Complications of RDS
The single most important complication of RDS, in terms of morbidity, treatment and cost, is bronchopulmonary dysplasia (BPD). BPD can occur even in the presence of only mild respiratory disease (Bancalari and del Moral 2001) and will affect up to 40 % of infants born before 29 weeks gestation (Patel and Greenough 2008). The use of antenatal steroids, surfactant and newer ventilatory techniques has not significantly reduced the incidence of BPD (Van Marter et al. 2001; Lemons et al. 2001).
Air leak syndromes including pulmonary interstitial emphysema, pneumothorax and pneumomediastinum used to be high in infants with RDS, but following the introduction of exogenous surfactant, the use of triggered ventilation techniques and shorter inflation times, these complication rates have fallen to about 5 % in infants ventilated for RDS (Rennie 2005).
Other major complications include PDA, intraventricular haemorrhage and renal failure. The incidence of symptomatic PDA increases with the fluid overload seen in infants with RDS (Bell et al. 1980); this in turn increases the risk of significant pulmonary haemorrhage. There has been considerable debate in the literature regarding the use of prophylactic indomethacin for very low birth weight babies with RDS, as indomethacin has been shown to reduce PDA and possibly reduce severe IVH (Fowlie 1996; Fowlie and Davis 2003). Long-term follow-up of infants who received prophylactic indomethacin has not demonstrated any beneficial effect on mortality or neurodevelopment (Fowlie and Davis 2003). Infants with RDS require close control of PaCO2, blood pressure and coagulation, to minimise the risk of developing IVH and acute tubular necrosis.
47.2.1.9 Short- and Long-Term Outcome of RDS
Long-term complications following RDS may develop as a result of oxygen toxicity, ventilator-induced lung and airway injuries, or from periods of hypoxia. The major complication of RDS remains chronic lung disease, bronchopulmonary dysplasia (BPD).
47.2.1.9.1 Survival
Overall mortality from RDS is between 5 and 10 % and is rare in infants of birth weight greater than 1,500 g (Rennie 2005). Death from RDS occurs most frequently between days 2 and 7 of life. Infants who receive prolonged ventilation from birth have lower survival rates and higher rates of impairment (Gaillard et al. 2001; Walsh et al. 2005).
47.2.1.9.2 Bronchopulmonary Dysplasia: Chronic Lung Disease
The definition of BPD has evolved over recent years from the original description of oxygen dependency at 28 days with corresponding x-ray changes (Northway et al. 1967). It has now been shown that oxygen dependence at 36 weeks corrected gestational age correlates better with long-term morbidity (Shennan et al. 1988). Infants born below 32 weeks gestation are assessed at 36 weeks corrected age, or at hospital discharge, whichever is sooner, and BPD is classified as mild, moderate or severe. Infants who need supplemental oxygen at 28 days of age, but who are in air at 36 weeks corrected age, have mild disease. Infants requiring up to 30 % oxygen at 36 weeks corrected age have moderate disease, and infants requiring more than 30 % oxygen, or positive pressure support, have severe disease. Infants born after 32 weeks gestational age are assessed by the same criteria at 56 days of age, or at hospital discharge, whichever is sooner (Jobe and Bancalari 2001).
It is difficult to predict infants who will go on to develop BPD from the appearance of the initial x-rays as the findings depend upon the amount of fetal lung fluid present and the phase of respiratory cycle in which the x-ray was taken. Positive pressure support and early surfactant use improve the x-ray appearance so early images are a poor guide to outcome (Kanto et al. 1978). The incidence of BPD in very low birth weight infants ranges from 15 to 50 %; quoted incidence varies as the proportion of extremely low birth weight babies in different studies varies (Sinha and Donn 2006). The oxygen saturation target, and ventilation strategy of individual neonatal units, influences the number of infants receiving supplemental oxygen and therefore the quoted rates of BPD. Numbers of infants with BPD have increased over recent years, and this may reflect the increased survival of very low birth weight infants. Many factors affect the risk of developing BPD: the degree of prematurity, the severity of the disease, oxygen toxicity, effects of ventilator-induced lung injury (barotrauma, volutrauma, atelectasis, shear trauma and biotrauma), PDA and the presence or absence of air leak. Infants who develop BPD commonly have exacerbations of their lung disease in childhood, requiring readmission to paediatric wards both in the first year (Mutch et al. 1986) and throughout childhood (McCormick et al. 1993). These infants are at risk of serious decompensation should they contract bronchiolitis, and regimens exist for respiratory syncytial virus prophylaxis to specific groups of children with BPD.
47.2.1.9.3 Neurological Outcome
Although most infants with RDS have normal neurological outcomes, those who require prolonged ventilation and develop BPD have more neurological sequelae than those with mild disease not requiring ventilation (Anderson and Doyle 2006). One follow-up study showed that infants with RDS who required prolonged continuous ventilation, for at least 28 days, were more likely to die or have abnormal neurological outcome, than those requiring less ventilation. The study also showed that very low birth weight infants with major cranial ultrasound abnormalities who had prolonged ventilation, all either died or had abnormal neurodevelopmental outcome (Thomas et al. 2003).
47.2.1.10 Conclusions
RDS remains a major problem for extremely low birth weight infants. How these infants are managed in the first few minutes of life may determine their long-term outcome. BPD is a major cause of severe neonatal morbidity (Ehrenkranz et al. 2005) and mechanical ventilation is a prime risk factor (Jobe and Bancalari 2001). How to use CPAP and surfactant to the infant’s best advantage, while avoiding lung injury, still needs to be determined. Optimal devices and settings for CPAP and NIPPV delivery need to be researched. On the horizon are developments such as nebulised surfactant, non-invasive ventilation, high-flow nasal cannula treatment, interactive modes of mechanical ventilation and the use of heliox. These treatments have the potential for improved management and outcome in the population of preterm infants at highest risk of RDS and are all the subject of ongoing trials.
Essentials to Remember
Respiratory distress syndrome (RDS) is the most common reason for admission to a neonatal intensive care unit.
In RDS the lungs are non-compliant and atelectatic with high surface tension and small airways collapse.
On CXR diffuse infiltrates have the appearance of ground glass which outlines larger air-filled bronchioles.
Risk of developing RDS varies with lung maturity which is related to gestational age and the use of antenatal steroids.
Mortality from RDS is 5–10 %, and antenatal steroids and surfactant replacement reduce mortality rates.
Management of RDS involves supporting respiration using a minimally invasive lung protective strategy, to reduce the risk of developing BPD.
Use of PEEP at delivery, judicious use of supplemental oxygen, early CPAP with or without prophylactic surfactant and restriction of invasive mechanical ventilation all play a role in reducing the risk of developing BPD.
BPD will affect up to 40 % of infants born before 29 weeks. Newer ventilatory techniques have not significantly reduced the incidence of BPD.
Numbers of infants with BPD have increased over recent years, and this may reflect the increased survival of very low birth weight infants with RDS.
Further research is required to define the optimal modes of respiratory support in RDS, to avoid lung injury.
47.2.2 Neonatal Pneumonia
Peter G. Davis8 and Louise S. Owen8
(8)
Department of Newborn Research, The Royal Women’s Hospital, 20 Flemington Rd, Parkville, VIC, 3052, Australia
Educational Aims
To define neonatal pneumonia and its classification
To describe the histopathology and common causative organisms
To outline why neonates are susceptible to pneumonia and define subgroups at highest risk
To describe appropriate therapy including antibiotics and respiratory support
To describe outcomes following neonatal pneumonia
Pneumonia may be defined as inflammation of the lung with consolidation. The term is usually used to indicate infection of the lung parenchyma resulting in obliteration of alveolar air spaces by purulent exudate. The lungs are a common site of infection in the newborn. Infection may be viral or bacterial in origin and may be acquired before birth, during delivery or in the early postnatal period. The clinical manifestations are often subtle and non-specific. Systemic signs may precede signs of respiratory distress and x-rays and blood tests have limited predictive value. It is important, therefore, to consider the diagnosis and treat early, as pneumonia is an important cause of mortality and morbidity in this age group.
47.2.2.1 Pathophysiology
47.2.2.1.1 Host Defences of the Newborn
The host defences in the lung of the newborn infant are less well developed than those of older children and adults. Polymorphonuclear neutrophils have reduced phagocytic and microbicidal activities as well as diminished capacity for chemotaxis and adhesion (Hill 1987). Natural killer cells, while normal in number, have reduced cytolytic activity against target cells. Circulating complement levels are reduced to around 50 % of levels seen in older children. Transmission of maternal IgG antibodies across the placenta confers a degree of immune protection. However, the neonate is poorly protected against organisms that predominantly evoke IgA or IgM antibodies. Importantly, preterm infants miss out on the placental transfer of antibodies which mostly occurs late in the third trimester of pregnancy.
As a result of impaired host defences, infections are more common and cause greater disruption of normal lung structure and function in both term and preterm neonates.
47.2.2.1.2 Pathology
Bacterial infections commonly give rise to inflammation of the pleura, infiltration and destruction of the bronchopulmonary tissue and exudate containing leukocytes and fibrin within the alveoli and small airways (Davies and Aherne 1962). An interstitial pattern with infiltration of mononuclear cells and lymphocytes is more typically seen in viral pneumonia.
Damage to the lungs occurs due to direct injury by the invading microorganisms and indirectly as a result of inappropriate or excessive responses by the host defence system. Direct injury is mediated by microbial enzymes, proteins and toxins that disrupt host cell membranes and metabolism. For example, group B streptococcal (GBS) pneumonia is characterised by exudative pulmonary oedema and alveolar haemorrhage. The organism appears to injure lung microvascular endothelial cells via a pore-forming hemolysin (Gibson et al. 1999). Inflammation attracts phagocytes which release substances that may help defend the body against the invading organisms but may result in poorly regulated cascades which damage host tissues.
Injury leads to an increased airway smooth muscle tone, mucous secretion and debris within the airways. In turn, this causes increased airway resistance, partial or total airway obstruction and atelectasis or air trapping. Surfactant inactivation by proteinacious exudate exacerbates the impairment of lung function. Gas exchange is impaired by increased barriers to alveolar diffusion, intrapulmonary shunting and ventilation-perfusion mismatch. An increased metabolic demand of the lungs and other tissues to which the infection may have spread exacerbates these problems.
Some bacterial infections are associated with typical pathological features. Staphylococcus aureus and Klebsiella pneumoniae cause extensive tissue damage and may lead to abscess formation and empyema.
47.2.2.2 Lung Mechanics
Neonatal pneumonia causes impaired lung mechanics through a variety of pathways. Respiratory drive is frequently reduced, leading to retention of carbon dioxide and culminating in apnoeic episodes requiring respiratory support. Hypoxaemia from hypoventilation is relatively easily overcome by increasing the inspired oxygen concentration.
Inflammation and infection involving the distal air spaces decreases ventilation to the affected areas. If perfusion of these areas is maintained, ventilation-perfusion mismatch occurs. When alveoli are completely filled with exudate, there may be no ventilation and extreme ventilation-perfusion inequality results. Hypoxaemia is the consequence of such an intrapulmonary shunt, and the low PaO2 is not overcome by administering high oxygen concentrations.
Pneumonia causes leakage of proteins from the intravascular and interstitial spaces into the alveoli. Fibrin, fibrinogen and albumin inhibit surfactant function, leading to a further reduction in functional residual capacity, decreased pulmonary compliance and increased work of breathing.
47.2.2.3 Epidemiology
47.2.2.3.1 Early Onset Pneumonia
Early onset pneumonia presents within the first 3 days of life. Transplacentally acquired pneumonia is a relatively rare form of early onset pneumonia. It includes those pneumonias caused by rubella virus, cytomegalovirus, Treponema pallidum and Listeria monocytogenes. Many of these infants are stillborn or die in the first days of life.
More commonly it is due to aspiration of infected amniotic fluid before or at the time of delivery. In developed countries, group B streptococcus (GBS) is the most common bacterial pathogen, but gram-negative organisms such as E. coli are also prevalent. In contrast, E. coli is the main organism in developing countries. Blood cultures are frequently positive when these organisms are involved. Listeria species, herpes simplex virus, candida, enterovirus and adenovirus have also been reported.
Initial treatment with a penicillin (penicillin G or ampicillin) and an aminoglycoside (gentamicin) is appropriate pending blood cultures. Acyclovir should be started if herpes simplex virus pneumonia is suspected. As the clinical and radiological signs of pneumonia are not specific, treatment of all cases of respiratory distress with appropriate antibiotics is the safest option.
47.2.2.3.2 Late-Onset Pneumonia
Late-onset pneumonia, beyond the first 72 h of life, may be caused by the same organisms, but Staphylococcus aureus, coagulase-negative Staphylococci and gram-negative bacilli are most common. Blood cultures are frequently negative in late-onset pneumonia.
Choice of antibiotics is governed by the resistance profiles of the setting. Where drug-resistant staphylococci are prevalent, the combination of vancomycin and gentamicin provides suitable cover.
47.2.2.3.3 Factors Associated with Increased Risk
Race and economic factors are associated with risk of early neonatal pneumonia. A study conducted in the 1960s showed that black infants who died in the first 48 h of life had an incidence of pneumonia of 27.7 %, compared with 11.3 % of white infants. The difference was consistent across all weight groups (Fujikura and Froehlich 1967). Similar differences were found by Naeye et al. in a series of consecutive autopsies of newborn and stillborn infants. Black infants had significantly higher rates of pneumonia (37 %) than Puerto Rican (22 %) or white infants (20 %). They also found that babies from families with the lowest income had significantly higher rates of pneumonia than infants from higher income families (Naeye et al. 1971).
Late-onset bacterial pneumonia may occur in nursery epidemics as a result of an infected health care worker or contaminated equipment. Viral epidemics have also been reported. Respiratory syncytial virus and influenza virus are amongst the causative organisms, and direct contact and droplets are the most common modes of spread.
47.2.2.4 Incidence
The reported rates of neonatal pneumonia vary widely depending on site, definition and method of ascertainment. However, it is well established that pneumonia is an important cause of mortality and morbidity in developing countries (Duke 2005). Between 750,000 and 1.2 million neonatal deaths are thought to be due to pneumonia which equates to 10 % of global child mortality (Nissen 2007). A field study in rural India found a mortality rates for pneumonia in the first month of life of 29 per 1,000 live births (Bang et al. 1993). The incidence is much lower in developed countries. Webber et al. prospectively studied neonatal pneumonia in single tertiary unit in Oxford (Webber et al. 1990). Over a 41-month period, they diagnosed 35 cases of early onset pneumonia amongst 19,569 live-born infants (1.79 per 1,000). Group B streptococcus was the predominant organism (69 %). Late-onset pneumonia occurred in 39 infants, the overwhelming majority of whom were preterm (92 %) and ventilated (87 %). Sinha et al. conducted a retrospective cohort study of neonatal infections using data from a large health maintenance organisation. In this US setting although infection was common during the first 30 days of life, pneumonia was uncommon compared to other infections. They reported rates of pneumonia of 4 per 1,000 during a nursery stay, 0.3 per 1,000 at paediatric office visits and 0.1 per 1,000 at emergency department visits (Sinha et al. 2003).
47.2.2.5 Risk Factors
47.2.2.5.1 Early Onset Pneumonia
Ascending infection from the maternal genital tract is the most common mode of acquisition of early onset pneumonia. Therefore, prolonged rupture of the membranes, variously defined as beyond 18 or 24 h duration, is an important risk factor for neonatal pneumonia. Signs of maternal infection, e.g. maternal fever and uterine tenderness, may give early warning of an infant at risk. Frequent pelvic examinations during labour are also considered a risk factor. Persistent fetal tachycardia is a relatively specific sign of infection, and its presence on CTG during labour should be communicated to those responsible for postnatal care of the infant.
Vaginal and rectal carriage of GBS occurs in 10–20 % of pregnant women. Infants at highest risk for GBS are those whose mothers carry the organism but have little or no circulating anti-GBS immunoglobulin. Approximately 1 % of infants born to carrier mothers become infected. Early onset GBS disease affects 1.8 per 1,000 live births.
Infected dairy products are considered the most important reservoir for transmission of Listeria monocytogenes. Women with HIV are more susceptible to infection with this organism.
47.2.2.5.2 Late-Onset Pneumonia
Late-onset pneumonia is strongly associated with assisted ventilation, and the risk is substantially higher for preterm infants. Rates vary according to the stringency of definition. Colonisation of the endotracheal tube is common, but using strict criteria, including positive blood culture of a respiratory pathogen, the rate of late-onset pneumonia in infants ventilated for more than 24 h in the Oxford study was 10 % (Webber et al. 1990). In a single-centre cohort study of ventilated infants of birth weight <2,000 g in St. Louis, the overall rate of ventilator-associated pneumonia was 11 %. Diagnosis was based on focal infiltrates on chest x-ray in combination with antibiotic usage for 1 week. The rate was substantially higher (28 %) in infants <28 weeks gestation (Apisarnthanarak et al. 2003). Using a less strict definition, Halliday et al. reported a pneumonia rate of 35 % in preterm infants ventilated during a randomised trial of surfactant therapy (Halliday et al. 1984). Other risk factors for late-onset pneumonia include neurological impairments leading to aspiration and congenital abnormalities of the lung and airways, e.g. tracheo-oesophageal fistula and cystic adenomatoid malformations. Preventable factors such as poor hand washing (Harbarth et al. 1999) are important in both developed and developing countries.
47.2.2.6 Stepwise Approach to Respiratory Support
47.2.2.6.1 Basic Principles
Successful treatment of neonatal pneumonia depends on consideration of the diagnosis in the differential diagnosis of any unwell newborn infant and early commencement of appropriate antibiotic therapy. The goals of treatment are to eradicate the infection and provide adequate respiratory support to allow intact survival of the infant.
There is less evidence to guide clinicians regarding the ventilation of infants with pneumonia compared with RDS. However, the hierarchy of respiratory support is similar to that for RDS. Requirements should be titrated against an infant’s needs. Regular clinical assessment, in addition to continuous cardiorespiratory and oxygen saturation monitoring, allows the clinician to gauge the infant’s progress and intervene appropriately.
47.2.2.6.2 Non-invasive Support
Active infants with respiratory distress whose breathing is regular may only require supplemental oxygen to maintain normal oxygen saturations. Additional support may be required to manage an infant with inadequate respiratory drive or severe lung disease. Sepsis in general and pneumonia in particular are often associated with apnoeic pauses. These occur in term infants but are more common in preterm infants. If apnoeic infants require frequent stimulation, i.e. more often than once per hour, or bag and mask ventilation, then additional support is required. Nasal CPAP may be useful as it reduces the work of breathing and leads to more regular respirations.
47.2.2.6.3 Invasive Support
Infants with severe respiratory distress, particularly when associated with respiratory acidosis, require intubation and ventilation. Regular assessment of blood gases is essential to avoid the dangers of excessive ventilation, i.e. hypocarbia and volutrauma as well as underventilation and worsening respiratory acidosis.
47.2.2.6.3.1 PEEP and Tidal Volume
There are no randomised trials comparing different modes of ventilation for infants with pneumonia. Given the paucity of human data, some animal data may usefully inform clinical practice. Using an adult rat model of pseudomonas pneumonia, Lin et al. showed that the choice of ventilator parameters is potentially important in determining the outcome of pneumonia (Lin et al. 2003). They compared an injurious mode of ventilation, zero PEEP and high tidal volumes with a lung protective strategy, standard PEEP and moderate tidal volume. Rats undergoing the injurious strategy had increased rates of bacteraemia and higher serum levels of inflammatory cytokines. In a series of experiments using a newborn piglet model of group B streptococcal pneumonia, van Kaam and Lachmann demonstrated the importance of PEEP and atelectasis. The use of (1) surfactant prophylaxis and (2) a strategy of peak and end-expiratory pressures designed to avoid atelectasis each independently resulted in attenuated bacterial growth and translocation into the blood stream (van Kaam et al. 2004). In a similar study, this group compared three different PEEP levels after surfactant lavage and group B streptococcus inoculation. The lowest PEEP group had the worst lung function and the highest mortality. The highest PEEP group had higher rates of translocation of bacteria into the bloodstream than the optimum PEEP group (Lachmann et al. 2007). The implications for clinicians are that care should be exercised in choice of ventilator settings and overdistension and atelectasis should be avoided.
47.2.2.6.3.2 High-Frequency Oscillatory Ventilation and Nitric Oxide
There are no trials which definitively identify the role of high-frequency oscillatory ventilation in the management of neonatal pneumonia. Typically this form of support is reserved for the sickest infants, i.e. those with the most difficulties with oxygenation and carbon dioxide retention. Donn and Sinha appropriately caution clinicians using high-frequency ventilation for infants with sepsis as this modality may exacerbate an already compromised cardiac output (Donn and Sinha 2003). Judicious use of volume replacement and inotropes may be required when this form of ventilation is used in infants with severe respiratory failure and hemodynamic compromise. When pulmonary hypertension is a feature, typically in group B streptococcal pneumonia, the combination of high-frequency ventilation and nitric oxide may be appropriate. Kinsella and Abman suggest that for pulmonary hypertension where diffuse parenchymal disease and underinflation are features, e.g. neonatal pneumonia, recruitment of air spaces using high-frequency oscillatory ventilation enhances delivery and effectiveness of inhaled nitric oxide (Kinsella and Abman 1998).
47.2.2.6.3.3 Exogenous Surfactant Therapy
Natural surfactants contain host defence factors. Surfactant proteins A and D modulate the inflammatory response to infection and assist in phagocytosis and killing of invading organisms (Jobe 2000). Herting et al. showed that exogenous surfactant reduced bacterial growth and improved lung compliance in a rabbit model of GBS pneumonia (Herting et al. 1997). In a retrospective study of 118 infants with culture proven GBS pneumonia, Herting et al. showed that surfactant therapy improved gas exchange in about 75 % of infants. The response was slower and smaller in magnitude than that of infants with hyaline membrane disease. In the absence of randomised trials on the topic, surfactant therapy for neonatal pneumonia may be considered a potentially useful therapy for infants requiring endotracheal intubation and ventilation.
47.2.2.7 Short- and Long-Term Outcomes
Duke reported case fatality rates for neonatal pneumonia of between 8 and 48 % in a variety of community- and hospital-based studies (Duke 2005). The highest rates were seen in early onset disease. The studies predominantly were from India, the exception being the Oxford study of Webber et al. which reported a mortality rate of 14 % (Webber et al. 1990). Duke noted the risk factors for death included the presence of hypoxaemia, low birth weight and absence of tachypnoea (Duke 2005).
In developed countries outcomes are generally good. However, increased mortality is associated with preterm birth, pre-existing chronic lung disease or immune deficiencies. Residual pulmonary anomalies including pneumatocoele are relatively common, particularly with staphylococcal pneumonia. These sequelae are also seen in association with Streptococcus pneumoniae, Streptococcus pyogenes and Haemophilus influenzae and may persist for many months. However, long-term prognosis for complete recovery is excellent (Huxtable et al. 1964).
47.2.2.8 Conclusions
Worldwide, neonatal pneumonia is an important cause of morbidity and mortality. The symptoms and signs are non-specific; therefore, the diagnosis should be suspected in any infant with respiratory distress. Infants treated early with appropriate antibiotics have a good prognosis. Respiratory support should be matched to the infant’s requirements, aiming to allow treatment and resolution of the infection without causing additional ventilator-induced damage.
Essentials to Remember
Neonates are susceptible to pneumonia because many of the components of the host defence system are not fully developed.
Infections can be of early onset (first 3 days of life) or late (beyond the first 3 days).
Early infections are most commonly due to group B streptococcus and gram-negative bacteria. Initial treatment with a penicillin and an aminoglycoside is appropriate.
Late infections are most commonly due to staphylococci and gram-negative bacilli. Antibiotic therapy should be guided by local resistance patterns; where resistant staphylococci are prevalent, vancomycin and an aminoglycoside provide suitable cover.
Prolonged rupture of membranes, signs of maternal infection and persistent fetal tachycardia may provide early warning of the risk of early onset pneumonia.
The combination of assisted ventilation and prematurity increases the risk of late-onset infection.
The level of respiratory support should be titrated against the infant’s requirements: supplemental oxygen, nasal CPAP and conventional and high-frequency ventilation via an endotracheal tube may be required.
Outcomes following neonatal pneumonia in developed countries are generally good. Risks of death increase with associated disorders and prematurity.
47.2.3 Meconium Aspiration Syndrome
Peter A. Dargaville9
(9)
Department of Paediatrics, Royal Hobart Hospital and University of Tasmania, Hobart, TAS, Australia
Educational Aims
This chapter aims to give an understanding of:
The pathophysiology of MAS, in particular the causes of hypoxaemia and poor lung compliance
The epidemiology of the condition
The conventional and alternative means of respiratory support for MAS, including a stepwise approach to respiratory support, and the rationale for use of adjunctive therapies
The complications and outcome of MAS
47.2.3.1 Introduction
Meconium aspiration syndrome (MAS) is a complex respiratory disease of the term and near-term neonate that continues to place a considerable burden on neonatal intensive care resources worldwide. MAS is a disease in evolution, with both the incidence and severity directly linked to improvements in antenatal and peripartum care. In the developed world, largely as a result of a more aggressive management of post-maturity, fetal growth restriction, placental dysfunction and intrapartum fetal distress, MAS has become uncommon but will never be eradicated completely. The outcome for afflicted infants has also improved substantially. In newly industrialised and developing countries, MAS remains a prominent cause of neonatal respiratory failure in the term infant, with a high risk of mortality.
MAS has features that make it stand alone amongst neonatal respiratory diseases – the unique combination of atelectasis, airflow obstruction and lung inflammation, the high risk of coexistent pulmonary hypertension and the fact of these occurring in a term infant with a mature lung structurally and biochemically. For all these reasons, management of MAS, and in particular the ventilatory management of MAS, has been a difficult challenge for neonatologists down the years.
In this chapter, MAS is defined as respiratory distress occurring soon after delivery in a meconium-stained infant that is not otherwise explicable and is associated with a typical radiographic appearance (Wiswell and Henley 1992).
47.2.3.2 Pathophysiology
Lung dysfunction in MAS is a variable interplay of several pathophysiological disturbances, chief amongst which are airway obstruction, epithelial injury, alveolar oedema, surfactant inhibition and pulmonary hypertension. Figure 47.1 shows a schematic of the pathogenesis of MAS, indicating the antecedents to these events, the critical one being entry of meconium into the lung (Dargaville and Mills 2005).
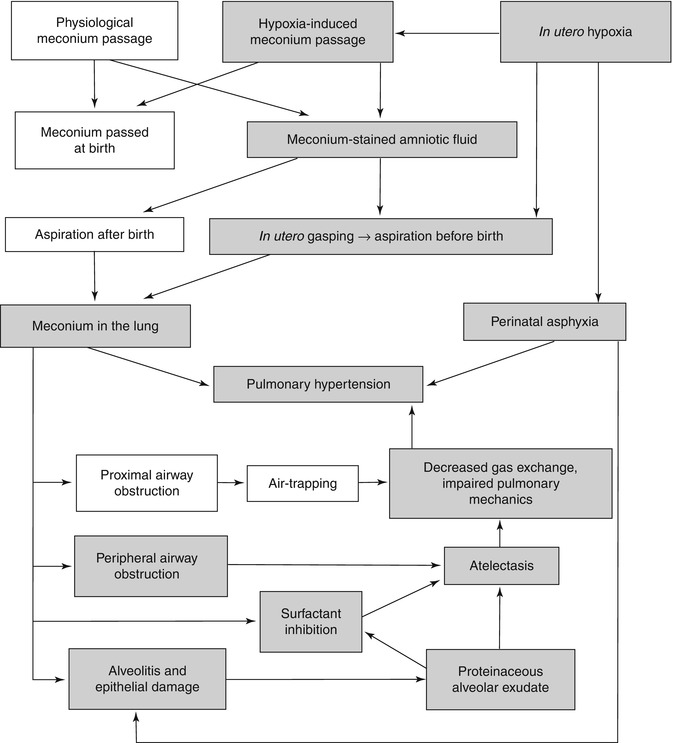
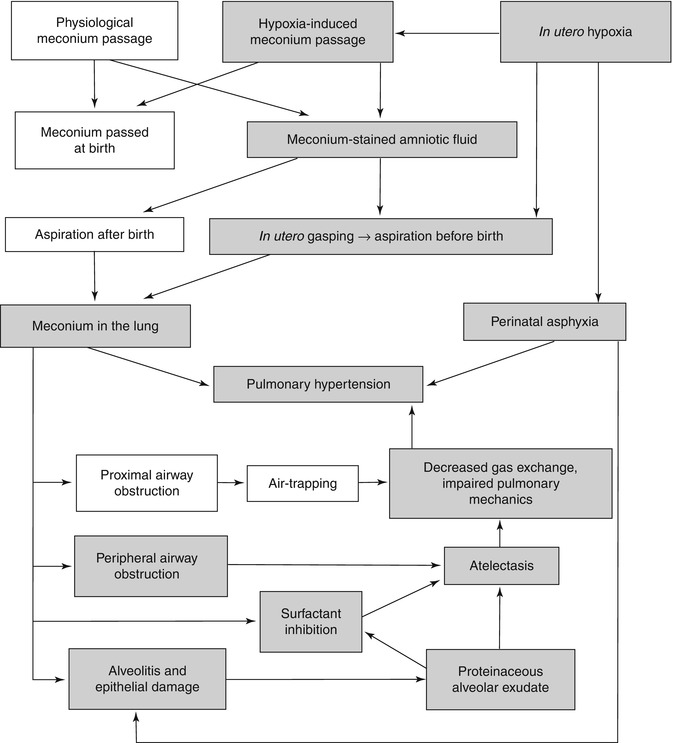
Fig. 47.1
Pathogenesis of meconium aspiration syndrome. Shaded boxes denote usual elements, and no shading denotes occasional elements (From Dargaville and Mills (2005); with permission)
Meconium is the viscid pigmented secretion of the fetal intestinal tract, which accumulates in the colon and distal small intestine in a layered fashion from the 12th week of fetal gestation. It is a noxious substance when inhaled, producing one of the worst forms of aspiration pneumonitis encountered in humans. Meconium has many adverse biophysical properties, including high tenacity (stickiness) (Rubin et al. 1996), extremely high surface tension (215 mN/m) (Rubin et al. 1996) and potent inhibition of surfactant function (Moses et al. 1991; Sun et al. 1993; Herting et al. 2001). Meconium is also directly toxic to the pulmonary epithelium, causing haemorrhagic alveolitis, and is chemotactic to neutrophils, activates complement and is possibly vasoactive (Oelberg et al. 1990; Dargaville et al. 2001; de Beaufort et al. 1998; Castellheim et al. 2005; Holcberg et al. 1999). These adverse properties of meconium are reflected in the sequence of pathophysiological disturbances known to occur in MAS (Fig. 47.1).
The pathogenesis of MAS after aspiration of meconium has been studied in animals with naturally occurring MAS (Shaffer et al. 1984), animal models of MAS induced using human meconium (Castellheim et al. 2005; Tyler et al. 1978; Tran et al. 1980; Davey et al. 1993; Wiswell et al. 1994; Gooding et al. 1971; Jones et al. 1996; Cayabyab et al. 2007) and in human infants with the disease (Dargaville et al. 2001; Dimitriou and Greenough 1995; Yeh et al. 1982). Once inhaled, meconium migrates distally down the tracheobronchial tree, obstructing airways of progressively smaller diameter (Tyler et al. 1978; Tran et al. 1980; Davey et al. 1993). In some instances there appears to be a considerable component of ‘ball-valve’ obstruction, with high resistance to airflow in expiration, and thus resultant gas trapping distal to the obstruction (Tran et al. 1980). If global in distribution, high functional residual capacity may result, although only in a small proportion of infants with MAS is there measurably high FRC (Dimitriou and Greenough 1995; Yeh et al. 1982), and even then only transiently (Yeh et al. 1982). For most infants with MAS, obstruction of the airways with meconium leads to downstream atelectasis (Fig. 47.2) (Wiswell et al. 1994). The juxtaposition of atelectatic and normally aerated lung units is reflected in the patchy opacification typically noted on chest x-ray in MAS (Fig. 47.3) (Yeh et al. 1979).
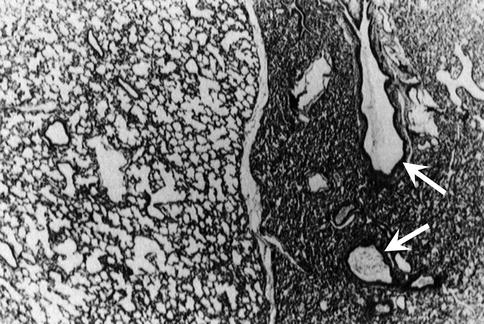
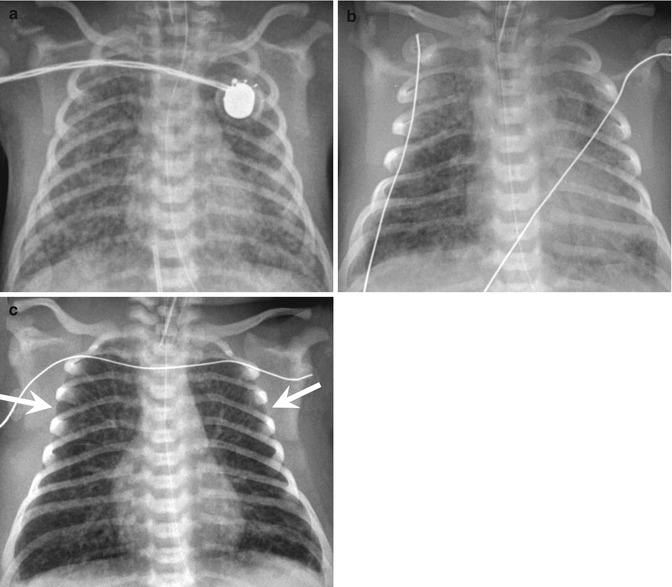
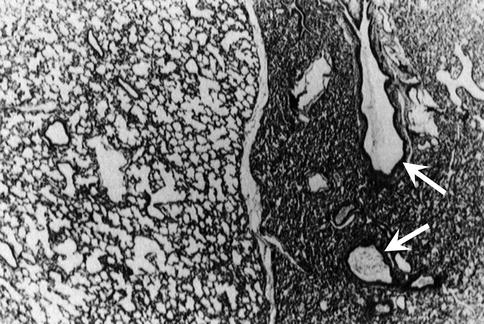
Fig. 47.2
Histological appearance of MAS. Section of lung from a piglet with experimental MAS, showing an area of normal lung expansion on the left, side by side with an area of atelectasis on the right. Meconium plugs are identified in the bronchi within the atelectatic region (arrows) (From Wiswell et al. (1994); with permission)
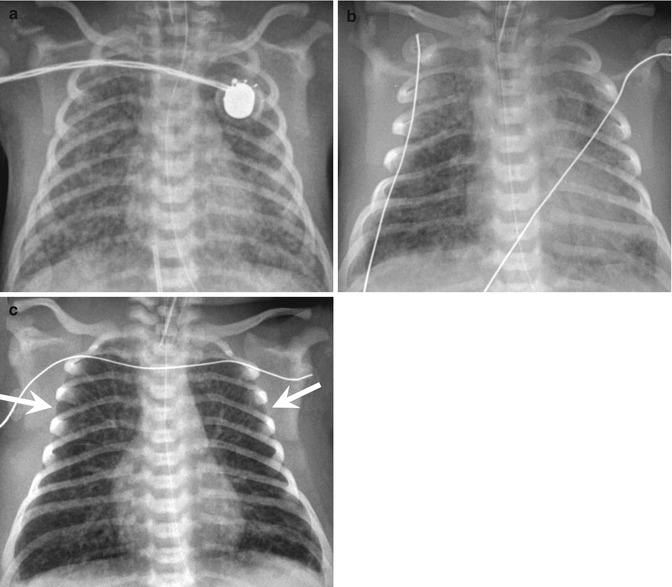
Fig. 47.3
Chest x-ray appearances in ventilated infants with MAS. Panel (a): Typical appearance of MAS showing ‘fluffy’ opacification widespread throughout the lung fields. Panel (b): Marked atelectasis in an infant with profound hypoxaemia. Panel (c): Hyperinflation and gas trapping, with a narrow cardiac waist, flattened diaphragms and intercostal bulging of the lung (arrows)
Experimentally, meconium instilled into the trachea reaches the alveoli within a few hours (Davey et al. 1993; Gooding et al. 1971), and the combination of haemorrhagic alveolitis and surfactant inhibition that follows potentiates the regional atelectasis. Meconium is toxic to the alveolar epithelium (Oelberg et al. 1990; Higgins et al. 1996), causing disruption of the alveolocapillary barrier and an exudative oedema not unlike that seen in acute respiratory distress syndrome. The underlying lung interstitium shows inflammatory cell infiltrate (Tyler et al. 1978; Davey et al. 1993), and there is a cytokine release in part related to complement activation (Castellheim et al. 2005; Jones et al. 1996; Cayabyab et al. 2007). The alveolar oedema potentiates the local atelectasis, causing variable degrees of ventilation-perfusion mismatch, or, worse still, intrapulmonary shunt. Moreover, meconium causes a potent dose-dependent inhibition of surfactant function (Moses et al. 1991; Sun et al. 1993; Herting et al. 2001), and, along with fibrinogen and haemoglobin in the exudate (Fuchimukai et al. 1987; Holm and Notter 1987), impairs the capacity of endogenous surfactant to reduce surface tension. Stability of alveoli at end expiration is thus compromised (Possmayer 2004), as is the capacity to clear oedema fluid from the air spaces (Carlton et al. 1995). The global consequence of these alveolar disturbances is a reduction in lung compliance (see below).
MAS is frequently accompanied by PPHN (Abu-Osba 1991), with many factors contributing to its development, including low pO2 and pH, coexistent intrauterine asphyxia and possibly vasoactive substances in the meconium itself (Wiswell and Bent 1993).
The most prominent and consistent physiological disturbances of pulmonary function in MAS are hypoxaemia and decreased compliance. Some degree of hypoxaemia is universal in symptomatic MAS, contributed to by many of the above-mentioned noxious effects of meconium. Disturbances of oxygenation in MAS may relate to atelectasis, overdistension, pulmonary hypertension or a combination of these. A challenging aspect of the management of MAS is to discern which mechanism of hypoxaemia is the predominant one in any given infant at any given time.
47.2.3.3 Lung Mechanics and Functional Residual Capacity
In naturally occurring MAS in animals (Shaffer et al. 1984) and humans (Cayabyab et al. 2007; Yeh et al. 1982; Brudno et al. 1990; Beeram and Dhanireddy 1992; Kugelman et al. 1995; Szymankiewicz et al. 2004), as well as in animal models of MAS (Tran et al. 1980; Davey et al. 1993), lung or respiratory system compliance is significantly impaired. Some studies in experimental animals have indicated that decreased compliance may be related to hyperinflation secondary to ‘ball-valve’ airway obstruction (Tran et al. 1980). In human infants, poor compliance has been noted with low and high FRC, although the only study reporting measurement of both indices simultaneously has been in non-ventilated infants with MAS of mild to moderate severity (Yeh et al. 1982). This study also demonstrated that most infants with MAS have FRC values in the normal range, with a subgroup showing high lung volumes, in particular, on the second day of life. Undoubtedly, in infants with more severe MAS requiring ventilation, there is the potential for overdistension of relatively unaffected lung regions which, due to their relatively long time constant, may empty incompletely during the ventilator expiratory cycle, especially at fast ventilator rates (Ramsden and Reynolds 1987). Respiratory resistance has also been noted to be increased in some studies, but variations in the technique of measurement make interpretation of these results difficult (ATS-ERS Pediatrics Assembly 1993).
47.2.3.4 Epidemiology
In most cases, MAS has its origin in two prenatal events. The first of these is in utero passage of meconium, and the second is an exaggeration of the normal pattern of fetal respiration (Duenhoelter and Pritchard 1977), to the point where the normal net efflux of fluid from the fetal lung is reversed and meconium gains entry into the lung in an amniotic fluid vehicle. Inhalation of meconium or meconium-stained fluid may also occur as an immediate postnatal event with the first breaths of extrauterine life. The lack of impact of oropharyngeal suction performed prior to the first breath on the risk and severity of subsequent MAS (Vain et al. 2004) suggests that postnatal inhalation of meconium is considerably less important as a cause of MAS, and that most cases are of prenatal origin.
Passage of meconium in utero is frequent (~10–15 %) (Wiswell and Bent 1993), with the most important determinant under normal circumstances being gestational age. Meconium passage occurs in 4 % of infants <38 weeks, 13 % at 39–40 weeks and 25–50 % of infants beyond 42 weeks (Ostrea and Naqvi 1982; Eden et al. 1987) and appears in many post-mature infants to be a physiological event not preceded by in utero compromise. On the other hand, in some instances prenatal meconium passage is clearly linked to fetal distress, with meconium-stained amniotic fluid more likely to occur where there is low fetal pH and/or low Apgar scores (Wiswell and Bent 1993).
The likelihood of MAS developing in the presence of meconium-stained amniotic fluid is also affected by the presence of fetal compromise. Low Apgar score is a very strong predictor of MAS amongst meconium-stained infants, with the odds ratio for MAS in the presence of a 5 min Apgar score <7 being as much as 21 (Wiswell et al. 2000). Risk of MAS is also higher when the liquor is heavily meconium-stained (Wiswell and Bent 1993; Wiswell et al. 2000).
47.2.3.5 Incidence
In the past few decades, there appears to have been a reduction in the incidence of MAS in many centres, at least in the developed world (Wiswell et al. 1990; Sriram et al. 2003; Yoder et al. 2002; Dargaville and Copnell 2006). The incidence of MAS requiring intubation and mechanical ventilation is now 0.4–0.6 per 1,000 live births (Dargaville and Copnell 2006; Gouyon et al. 2008). Incidence of MAS remains high outside the developed world, with hospital-based studies suggesting an incidence of MAS requiring intubation of 1.4–7 per 1,000 live births (Bhat and Rao 2008; Velaphi and Van Kwawegen 2008).
47.2.3.6 Risk Factors
Amongst all live births, several risk factors for MAS have been identified, with the presence of fetal compromise overshadowing all others. Compared to infants with a 5 min Apgar score of 7 or above, those with a score below 7 had an odds ratio of 52 for the development of MAS requiring intubation (Dargaville and Copnell 2006). Other important risk factors for MAS include advanced gestation (Yoder et al. 2002; Dargaville and Copnell 2006), black or indigenous or Islander ethnicity (Sriram et al. 2003; Dargaville and Copnell 2006; Urbaniak et al. 1996), Caesarean delivery (Dargaville and Copnell 2006; Hernandez et al. 1993) and home birth (Dargaville and Copnell 2006).
47.2.3.7 Stepwise Approach to Respiratory Support
As noted in the sections above, MAS is a disease of many elements, which coalesce into a problematic respiratory syndrome that can be difficult to treat. An approach to respiratory support is set out below.
47.2.3.7.1 Oxygen Therapy
Supplemental oxygen administration is the foundation upon which treatment for MAS is built and, in many less severe cases, will be the only therapy required (Singh et al. 2009b). Some ventilated infants with MAS require high inspired oxygen concentration for long periods, with few apparent adverse effects. Infants persistently requiring an FiO2 >0.8 should, however, have measures taken to improve oxygenation (see Table 47.1).
Table 47.1
Approach to hypoxaemia in MAS
If there is marked global or regional atelectasis, with extensive radiological opacification, consider: |
Increasing PEEP to improve end-expiratory lung volume |
Increasing PIP to recruit atelectatic lung units |
Increasing inspiratory time to facilitate the recruiting effect of PIP |
Use of HFOV with sufficient distending pressure to recruit atelectatic lung units |
Use of HFJV with sufficient PEEP to maintain FRC and conventional breath PIP to recruit atelectatic lung units |
Exogenous surfactant |
Lung lavage |
If there is obvious gas trapping, with global or regional hyperlucency radiologically, along with distortion of normal anatomy (flattened diaphragms, narrow cardiac waist), consider: |
Decreasing PEEP (but may lose recruitment of areas prone to atelectasis) |
Decreasing inspiratory time and increasing expiratory time |
Use of HFJV with low PEEP, low frequency (240–360 bpm) and minimal CMV breaths |
Use of HFOV with relatively low P AW and low frequency (5–6 Hz) |
If there is pulmonary hypertension, with a pre- and post-ductal SpO2 difference and/or evidence of increased right ventricular pressure, consider: |
Correction of potentiating factors – hypoglycaemia, hypocalcaemia, hypomagnesaemia, polycythaemia, hypothermia and pain |
Bolstering systemic blood pressure to reduce right-to-left ductal shunt – volume expansion and pressor agents |
Improving right ventricular function – inotrope infusion |
Selective pulmonary vasodilators – inhaled nitric oxide |
Moment by moment titration of oxygen concentration (or flow) in infants with MAS should be according to SpO2 level, with a pre-ductal reading to be preferred and the SpO2 target range being higher (e.g. 94–98 %) than that used in preterm infants. In ventilated infants, oxygen therapy should also be monitored by regular blood gas sampling from an intra-arterial line, preferably in a pre-ductal position in the right radial artery. Suggested target pO2 range is 60–100 mmHg (pre-ductal). Where there is considerable PPHN, titration of FiO2 using post-ductal pO2 values is not advisable.
47.2.3.7.2 Continuous Positive Airway Pressure (CPAP)
Of all infants requiring mechanical respiratory support because of MAS, approximately 10–20 % are treated with CPAP only (Wiswell et al. 2000; Dargaville and Copnell 2006; Singh et al. 2009b). Additionally, around one-quarter of infants requiring intubation with MAS receive CPAP before and/or after their period of ventilation (Dargaville and Copnell 2006). CPAP for such infants can be effectively delivered by bi-nasal prongs or a single nasal prong, typically with a CPAP pressure of 5–8 cm H2O. Tolerance of the CPAP device may be limited given the relative maturity of infants with MAS, and on occasions the associated discomfort will exacerbate pulmonary hypertension to the point where intubation becomes necessary.
47.2.3.7.3 Intubation
Approximately one-third of all infants with a diagnosis of MAS require intubation and mechanical ventilation (Wiswell and Bent 1993; Cleary and Wiswell 1998). This proportion varies according to how assiduously non-ventilated cases are identified in published series and also depends on ventilation practices of individual units. Indications for intubation of infants with MAS include (a) high oxygen requirement (FiO2 > 0.8), (b) respiratory acidosis, with arterial pH persistently less than 7.25, (c) pulmonary hypertension and (d) circulatory compromise, with poor systemic blood pressure and perfusion (Goldsmith 2008). Except in emergency circumstances, intubation of infants with MAS should be performed with premedication. Significant endotracheal tube leak is a major barrier to effective ventilation in infants with MAS, and in most cases a size 3.5 mm internal diameter endotracheal tube will be required. Once intubated, tolerance of the endotracheal tube will require ongoing sedation with infusions of an opiate (e.g. morphine or fentanyl) (Aranda et al. 2005), possibly supplemented with a benzodiazepine. Additionally, continuation of muscle relaxant drugs is often helpful during the stabilisation period after intubation, particularly in infants with coexistent pulmonary hypertension.
47.2.3.7.4 Conventional Mechanical Ventilation
Despite more than four decades of mechanical ventilation for infants with MAS, the ventilatory management of the condition remains in the realm of ‘art’ rather than ‘science’, with very few clinical trials upon which to base definitive recommendations. Physiological principles and published experience of ventilation in MAS do, however, allow some guiding principles to be put forward for conventional ventilation strategy.
47.2.3.7.4.1 Choosing a Mode of Ventilation
Ventilation mode and the value of patient triggering have been incompletely studied in MAS. Two randomised trials of patient-triggered ventilation have included infants with MAS. One of these found no advantage of synchronised intermittent mandatory ventilation (SIMV) over IMV in 15 infants with MAS (Chen et al. 1997). Another study found, in a group of 93 infants >2 kg birth weight (including an unspecified number with MAS), that use of SIMV was associated with a shorter duration of ventilation compared with IMV (Bernstein et al. 1996). Despite the relative paucity of evidence in favour, it seems logical to use a synchronised mode of ventilation in any spontaneously breathing ventilated infant with MAS. Trigger sensitivity should be set somewhat higher than for a preterm infant and should take into account the possibility of autocycling if there is a tube leak (Bernstein et al. 1995). There have been no clinical trials in patients with MAS comparing SIMV and synchronised intermittent positive pressure ventilation (SIPPV), also known as assist control. Given the propensity for gas trapping in MAS, there is some concern that using SIPPV may lead to high levels of inadvertent positive end-expiratory pressure (PEEP) with resultant hyperinflation. For this reason SIMV may be the most appropriate mode of ventilation in MAS.
47.2.3.7.4.2 Selection of Positive End-Expiratory Pressure
For any newborn respiratory disease, but particularly MAS, application of PEEP must balance the competing interests of overcoming atelectasis while avoiding overdistension. Early observations of the effect of PEEP suggested the greatest benefit with PEEP settings between 4 and 7 cm H2O, with higher PEEP settings (8–14 cm H2O) giving minimal oxygenation benefit (Fox et al. 1975). No more recent clinical studies exist to guide PEEP selection in MAS; physiological principles dictate that if atelectasis predominates (Fig. 47.3b), PEEP should be increased up to 10 cm H2O, whereas for regional or global hyperinflation (Fig. 47.3c), a lower PEEP (3–4 cm H2O) may be necessary (Goldsmith 2008). For infants with severe atelectasis, PEEP settings above 10 cm H2O are likely to increase the risk of pneumothorax (Probyn et al. 2004), and modes of high-frequency ventilation are to be preferred if available.
47.2.3.7.4.3 Selection of Inspiratory Time
As with PEEP, setting inspiratory time in MAS must take into account the balance between atelectasis and overdistension. Term infants have generally longer time constants than their preterm counterparts (Wood 2003) and thus require a longer inspiratory time (around 0.5 s) to allow near-full equilibration of lung volume change in response to the applied peak pressure. Even longer inspiratory times may be useful for lung recruitment during inspiration if atelectasis is prominent.
47.2.3.7.4.4 Selection of Peak Inspiratory Pressure (or Tidal Volume)
Given the reduced compliance, the peak inspiratory pressure (PIP) required to generate sufficient tidal volume in MAS are often high (30 cm H2O or more). Such pressures may well contribute to a secondary ventilator-induced lung injury in ventilated infants with MAS. Suggested target tidal volume is 5–6 mL/kg. If using a ‘volume guarantee’ mode, the peak pressure limit should be set at or near 30 cm H2O to allow the ventilator to scale up the PIP when needed to reach the tidal volume target. If PIP is persistently higher than 30 cm H2O, high-frequency ventilation should be considered, if available.
47.2.3.7.4.5 Selection of Ventilator Rate
Especially if there is gas trapping and expiratory airflow limitation, optimal conventional ventilation in MAS requires the use of a relatively low ventilator rate (<50) and hence longer expiratory time. This will help to avoid inadvertent PEEP. The resultant minute ventilation must be sufficient to produce adequate CO2 clearance. An acceptable arterial pCO2 range is 40–60 mmHg and pH 7.3–7.4, which is achievable in most infants even when there is significant parenchymal disease combined with PPHN (Gupta et al. 2002). Hyperventilation-induced alkalosis, which anecdotally appeared to reduce the need for extracorporeal membrane oxygenation (ECMO) in infants with PPHN (Walsh-Sukys et al. 2000), is no longer practised, in part due to the risk of sensorineural hearing loss (Hendricks-Munoz and Walton 1988).
47.2.3.7.5 High-Frequency Oscillatory Ventilation
Despite the dearth of clinical trial evidence suggesting a benefit (Henderson-Smart et al. 2009), high-frequency oscillatory ventilation (HFOV) has become an important means of providing respiratory support for infants with severe MAS failing conventional ventilation. Published series from large neonatal databases suggest that 20–30 % of all infants requiring intubation and ventilation with MAS are treated with high-frequency ventilation (Dargaville and Copnell 2006; Singh et al. 2009b; Tingay et al. 2007), with most of these receiving HFOV rather than high-frequency jet ventilation (HFJV). Indications for transitioning to HFOV include ongoing hypoxaemia and/or high FiO2 and, less commonly, respiratory acidosis. In infants with significant atelectasis, adequate lung recruitment may require the application of a mean airway pressure (P AW) considerably higher than on conventional ventilation (up to 25 cm H2O in some cases), with a stepwise recruitment manoeuvre likely to be the most effective (Pellicano et al. 2009). Once oxygenation has improved, P AW should then be reduced; most infants with MAS requiring HFOV can be stabilised using a P AW around 16–20 cm H2O, with gradual weaning in the days thereafter (Dargaville et al. 2007). Infants with prominent gas trapping may tolerate the recruitment process poorly, with reductions in oxygenation and systemic blood pressure and the potential for exacerbation of pulmonary hypertension. Recruitment manoeuvres of some form can still be advantageous in this group, with the benefit becoming apparent when the P AW is reduced.
Choice of oscillatory frequency is critically important in MAS, with experimental studies and clinical experience indicating that frequency should not be higher than 10 Hz and preferably should be set at 8 or even 6 Hz. In experimental models of MAS, high oscillatory frequency (15 Hz) is associated with worsening of gas trapping (Hachey et al. 1998). HFOV can also lend a clinical advantage in infants with significant coexisting PPHN, as the response to inhaled nitric oxide (iNO) is better when delivered on HFOV compared to conventional ventilation (Kinsella et al. 1997). Early reports suggested that up to half of infants with MAS treated with HFOV did not respond adequately and went on to receive ECMO (Carter et al. 1990; Paranka et al. 1995). More recent experience would suggest that only around 5 % of infants treated with HFOV and iNO fail to respond and transition to ECMO (Wiswell et al. 1990).
47.2.3.7.6 High-Frequency Jet Ventilation
The combination of atelectasis and gas trapping that can occur in MAS may be better managed with HFJV than HFOV, with the former technique offering the possibility of ventilation at a lower P AW (Keszler et al. 1986). A number of laboratory investigations have shown HFJV either alone or in combination with surfactant therapy, to be beneficial in animal models of MAS (Keszler et al. 1986; Wiswell et al. 1992, 1994). Clinical studies including infants with MAS appear to confirm the benefit of HFJV compared with conventional ventilation, both in terms of improvement in oxygenation and in avoidance of ECMO (Davis et al. 1992; Engle et al. 1997). Additionally, some infants with MAS failing on HFOV with hypoxaemia and/or respiratory acidosis do show improvements after transition to HFJV using a low frequency (240–360 bpm) and a low conventional ventilator rate (Dargaville (2010), unpublished observations).
47.2.3.8 Rationale for Using Adjunctive Therapies
47.2.3.8.1 Bolus Surfactant Therapy
The pathophysiology of MAS includes inhibition of surfactant in the air spaces, both by meconium and by exuded plasma proteins (Moses et al. 1991; Sun et al. 1993; Herting et al. 2001; Fuchimukai et al. 1987). Preliminary reports of the use of exogenous surfactant given as bolus therapy to ventilated infants with MAS were promising (Auten et al. 1991; Khammash et al. 1993), although it was identified that around 40 % of cases did not respond (Halliday et al. 1996). Four randomised controlled trials of bolus surfactant therapy have been conducted (Findlay et al. 1996; Lotze et al. 1998; Chinese Collaborative Study Group for Neonatal Respiratory Diseases 2005; Maturana et al. 2005), which when analysed together show a benefit in terms of reduction in need for ECMO, but not duration of ventilation or other pulmonary outcomes (El Shahed et al. 2007). In the developed world, bolus surfactant therapy is currently used in 30–50 % of ventilated infants with MAS (Dargaville and Copnell 2006; Singh et al. 2009b). Bolus surfactant therapy should be used judiciously in MAS, choosing infants with severe disease, and treating early, and if necessary, repeatedly (Dargaville and Mills 2005).
47.2.3.8.2 Lavage Therapy
Lung lavage using dilute surfactant is an emerging treatment for MAS that offers the potential of interrupting the pathogenesis of the disease by removal of meconium from the air spaces (Dargaville and Mills 2005). Laboratory studies and preliminary clinical evaluations have indicated that lavage therapy may improve oxygenation and shorten duration of ventilation in MAS (Cochrane et al. 1998; Wiswell et al. 2002; Dargaville et al. 2003). A recent randomised controlled trial of large volume lavage using dilute surfactant in infants with severe MAS noted no effect on duration of respiratory support or other pulmonary outcomes, but did find a higher rate of ECMO-free survival in the treated group (Dargaville et al. 2011). A further clinical trial would be necessary to more precisely define the effect on survival.
47.2.3.8.3 Corticosteroid Therapy
Steroid therapy has been investigated in MAS for more than three decades, with a number of small clinical trials being conducted, none of which have given a definitive result. One recent trial suggested that dexamethasone therapy could dampen the inflammatory response in MAS, as indicated by levels of tumour necrosis factor-α (Tripathi et al. 2007). In the absence of further trials, steroid therapy cannot be recommended as routine therapy in MAS.
47.2.3.8.4 Inhaled Nitric Oxide
Large randomised controlled trials have demonstrated the effectiveness of iNO in term infants with pulmonary hypertension, with a reduction in need for ECMO, and in the composite outcome of death or requirement for ECMO (Finer and Barrington 2006). Each trial included a large subgroup with MAS; overall more than 640 infants with MAS have been enrolled in iNO trials, although few have reported the outcome for MAS separately. The potential value of delivering iNO during HFOV has been highlighted in one trial, in which the proportion of nonresponders was lowest when the two therapies were combined (Kinsella et al. 1997). Currently around 20–30 % of all ventilated infants with MAS receive iNO (Dargaville and Copnell 2006; Singh et al. 2009b), and around 40–60 % show a sustained response (Gupta et al. 2002; Kinsella et al. 1997).
The approach to an infant with MAS and coexistent PPHN should initially focus on optimising the ventilatory management and, in particular, overcoming atelectasis if this is prominent radiologically. The severity of PPHN should be assessed clinically and by echocardiogram if available. If moderate to severe PPHN persists after appropriate ventilatory manoeuvres and the pO2 remains at less than 80–100 mmHg in FiO2 1.0 (Kinsella et al. 1997; Wessel et al. 1997), iNO should commence at a dose of 10–20 ppm. Higher doses do not appear to result in better oxygenation (Guthrie et al. 2004).
47.2.3.8.5 Extracorporeal Membrane Oxygenation
Infants with severe MAS have been treated with ECMO since 1976, and MAS has been the leading diagnosis amongst neonates referred for this therapy (Short 2008). With the advent of newer therapies, the number of infants with MAS treated with EMCO has decreased (Fliman et al. 2006), but survival with ECMO treatment for MAS has remained high (around 95 %) (Short 2008). The usual indication for commencing ECMO is intractable hypoxaemia despite optimisation of the patient’s condition with available therapies (including high-frequency ventilation and iNO and bolus surfactant therapy). Degree of hypoxaemia in this setting has generally been quantified using oxygenation index (OI), where OI = P AW × FiO2 × 100 / PaO2. An OI persistently above 40 despite aggressive standard management has been, and remains, an indication for treatment with ECMO where available (UK Collaborative ECMO Trial Group 1996).
47.2.3.9 Classical Complications
47.2.3.9.1 Air Leak
Pneumothorax is a feared complication of MAS which potentiates lung atelectasis and PPHN and compounds the difficulties with management. Around 10 % of all ventilated infants with MAS are reported to have this complication (Wiswell et al. 1990; Dargaville and Copnell 2006). Pneumothorax is associated with an increase in the risk of mortality (Dargaville and Copnell 2006; Lin et al. 2004), in part related to the severity of the associated lung disease, but also to the destabilising influence of the air leak itself. Clinicians should remain attuned to the possibility of pneumothorax in ventilated infants, particularly those prone to gas trapping, and should employ ventilatory strategies to avoid regional and global overdistension wherever possible. Effective treatment requires that air be evacuated from the pleural space immediately once the condition is diagnosed, and then in most instances, an intercostal drainage tube is required to control ongoing air leak.
Other air leak syndromes, including pneumomediastinum and pulmonary interstitial emphysema, are occasionally seen in MAS. Pneumopericardium and pneumoperitoneum are rare. Pneumomediastinum usually requires no treatment unless under significant tension (Masuda et al. 1984). Pulmonary interstitial emphysema in the setting of MAS at times results in the formation of multiple large cysts and can be extremely difficult to treat. The condition is best managed either with HFJV (see Table 47.1) or HFOV at low frequency (5–6 Hz).
47.2.3.9.2 Pulmonary Haemorrhage
Pulmonary haemorrhage (or, more correctly, haemorrhagic pulmonary oedema) occurs in a small proportion of infants with MAS and can occasionally cause severe destabilisation and hypoxaemia (Berger et al. 2000). Transient application of a high airway pressure is usually necessary to drive this oedema fluid back into the interstitium of the lung. This is best achieved using high-frequency ventilation, with P AW above 30 cm H2O sometimes required to re-recruit flooded alveoli.
47.2.3.9.3 Chronic Lung Disease
Cases of severe MAS succumbing after a long period of ventilation can have severe distortion of normal lung architecture on post-mortem examination (Chou et al. 1993). Refinements in ventilatory and adjunctive care now mean that fewer infants have long-standing severe chronic lung disease after MAS. Nevertheless, approximately 5–7 % of ventilated infants with MAS remain in oxygen for more than 4 weeks (Dargaville and Copnell 2006; Singh et al. 2009b), and 5 % go home in oxygen (Dargaville and Copnell 2006). A subset of infants who have had MAS in the newborn period will have wheezing and repeated hospitalisations in the first year of life and have demonstrable abnormalities on respiratory function testing (Yuksel et al. 1993). These abnormalities would be expected to largely resolve later in the first decade (see below).
47.2.3.9.4 Comorbidities
Seizures occur in around 10 % of all ventilated infants with MAS, most usually in the context of a coexistent hypoxic-ischaemic encephalopathy (Singh et al. 2009b; Cleary and Wiswell 1998). Circulatory insufficiency is common, and the majority of infants who have severe MAS and coexistent PPHN are treated with inotrope infusions (Dargaville et al. 2011). Multi-organ failure develops in a small proportion of such infants.
47.2.3.10 Short- and Long-Term Outcome
47.2.3.10.1 Mortality
Mortality related to MAS has decreased significantly, with population-based studies suggesting a mortality of 1–2 per 100,000 live births (Sriram et al. 2003; Dargaville and Copnell 2006; Nolent et al. 2004). The case fatality rate in ventilated infants with MAS varies widely in published series (0–37 %) (Cleary and Wiswell 1998) and is influenced by availability of alternative means of ventilation, adjunctive therapies including nitric oxide and ECMO. Approximately one-quarter to one-third of all deaths in ventilated infants with a diagnosis of MAS are directly attributable to the pulmonary disease, with the remainder in large part caused by hypoxic-ischaemic encephalopathy (Dargaville and Copnell 2006; Singh et al. 2009b; Nolent et al. 2004).
47.2.3.10.2 Duration of Ventilation, Oxygen and Hospitalisation
Considering all intubated infants with MAS, median duration of ventilation is 3 days (mean 4.8 days) (Dargaville and Copnell 2006). Infants with more severe disease, requiring at least one of HFV, iNO or bolus surfactant, are ventilated for a median of 5 days (Dargaville and Copnell 2006). Median duration of oxygen therapy and length of hospital stay currently stand at 7 and 17 days, respectively (Dargaville and Copnell 2006).
47.2.3.10.3 Long-Term Outcome
Respiratory compromise after hospital discharge is common in infants who were ventilated with MAS. Up to half of infants will be symptomatic with wheezing and coughing in the first year of life (Yuksel et al. 1993). Older children may exhibit evidence of airway obstruction, hyperinflation and airway hyperreactivity, but appear to have normal aerobic capacity (Swaminathan et al. 1989).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


