Acute Abdomen in Infants and Children
Eva Ilse Rubio, MD
DIFFERENTIAL DIAGNOSIS
Common
Appendicitis
Inguinal Hernia
Midgut Volvulus
Intussusception
Adhesions
Crohn Disease
Less Common
Ovarian Torsion
Pelvic Inflammatory Disease
Ectopic Pregnancy
Meckel Diverticulum
Nonaccidental Trauma/Child Abuse
Henoch-Schönlein Purpura
Foreign Body Ingestion
Rare but Important
Gastric Volvulus
Wandering Spleen
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Gender
Bilious emesis vs. nonbilious emesis
Presence or absence of bowel obstruction
If bowel obstruction, proximal or distal
Skin: Rash or bruising
Helpful Clues for Common Diagnoses
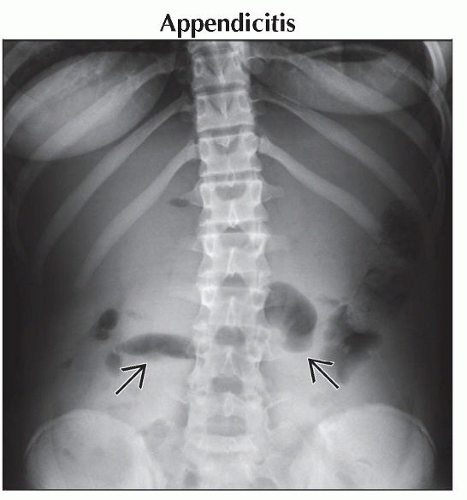
Appendicitis
Fever, leukocytosis, anorexia are expected but none are universal
Radiograph
Findings range from right lower quadrant air-fluid levels to frank small bowel obstruction
Useful for excluding free air
US
Noncompressible tubular structure > 7 mm in diameter
In children, may obviate CT and avoid radiation
Pitfall: Must see entire length of appendix to exclude tip appendicitis
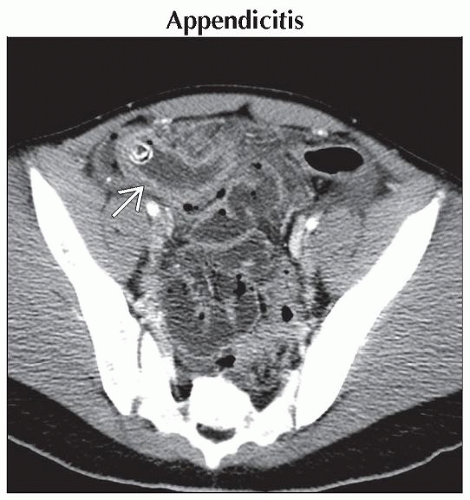
CT
Hyperemic walls, inflammatory stranding in fat
Inguinal Hernia
Radiograph may demonstrate loops of bowel in scrotal sac
US: Peristalsing bowel within scrotal sac
Midgut Volvulus
With midgut malrotation
Typical presentation in neonate with bilious emesis but may present at any age
Usually a proximal obstruction
Without midgut malrotation
Lead points include adhesions, Meckel diverticulum, or other abdominal lesions
Proximal or distal obstruction
Intussusception
Radiographs (notoriously unreliable) may suggest intussusception with rounded soft tissue density
US sensitive and specific for ileocolic intussusception
Bowel and mesenteric fat trapped within colon create “doughnut” sign if seen in transverse plane
Adhesions
Presents as partial, complete, or intermittent bowel obstruction
Adhesions not seen but transition point from dilated to collapsed bowel may be identified on CT
Crohn Disease
Marked bowel wall thickening, often with skip areas
Perirectal inflammation/abscess easily missed on imaging
Helpful Clues for Less Common Diagnoses
Ovarian Torsion
US: Torsed ovary is generally large, heterogeneous, predominantly hypoechoic
Pitfall: Blood flow on US may confound diagnosis due to intermittent torsion or multiplicity of blood supply to ovaries
Obvious size/volume discrepancy between ovaries is virtually always present
In postmenarchal patient, torsed ovarian volume often > 20 mL
In premenarchal patient, ovarian volumes markedly discrepant, but torsed ovarian volume may be < 20 mL
Consider underlying ovarian mass or cyst
Pelvic Inflammatory Disease
Ectopic Pregnancy
Look for extrauterine gestational sac
If ruptured, appears as complex cystic/solid mass with echogenic peritoneal fluid
Meckel Diverticulum
May present as bleeding, intussusception, or bowel obstruction
CT: Small bowel obstruction, inflammatory changes around bowel loops, hyperemic tubular structure
Nonaccidental Trauma/Child Abuse
Abdomen CT obtained when laboratory values are abnormal (liver, pancreatic enzymes, CK-MB)
Abdomen CT: Duodenal hematoma, jejunal perforation, liver laceration, pancreatic laceration, pericardial effusion
Scrutinize images for fractures
Rectal prolapse is uncommon but known presentation
Henoch-Schönlein Purpura
Small vessel vasculitis
Acute abdominal findings may precede rash, arthralgia, hematuria
CT findings may prompt clinical consideration
Marked bowel wall thickening predominantly in jejunum and ileum, with skip areas
Intussusception, ascites
Mesenteric lymphadenopathy and vascular engorgement
Foreign Body Ingestion
May cause perforation, erosion, obstruction
Multiple magnets retain attraction to each other, cause pressure erosion, perforation
Helpful Clues for Rare Diagnoses
Gastric Volvulus
Radiograph: Large spherical gastric bubble
Fluoroscopic upper gastrointestinal (UGI) study considered definitive
Mesenteroaxial gastric volvulus
Stomach folds and twists
Higher association with vascular compromise and obstruction in children
Pylorus near/above gastroesophageal junction
May be associated with congenital diaphragmatic or abdominal abnormalities
Organoaxial gastric volvulus
Stomach flips upside down
Lower likelihood of vascular compromise or acute obstruction in children
Greater curvature above lesser curvature; downward pointing pylorus
Mixed mesenteroaxial/organoaxial
Wandering Spleen
Spleen absent from usual position in left upper quadrant due to lax or absent splenic ligaments
Risk of torsion of long vascular pedicle
Higher risk of injury in minor accidents when not protected by thoracic cage
Image Gallery
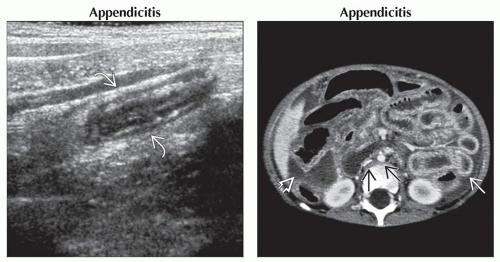 (Left) Longitudinal ultrasound shows an elongated dilated noncompressible tubular structure
 in the right lower quadrant. (Right) Axial CECT shows diffuse severe bowel wall thickening in the right lower quadrant. (Right) Axial CECT shows diffuse severe bowel wall thickening  , free fluid , free fluid  , flattened IVC, and small caliber aorta , flattened IVC, and small caliber aorta  in a 3 year old with perforated appendicitis who presented in septic shock with abdominal compartment syndrome. The patient survived after multiple abdominal washouts. in a 3 year old with perforated appendicitis who presented in septic shock with abdominal compartment syndrome. The patient survived after multiple abdominal washouts.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|