Chapter 661 Acne
Acne Vulgaris
Acne, particularly the comedonal form, occurs in 80% of adolescents.
Pathogenesis
The primary pathogenetic alterations in acne are (1) abnormal keratinization of the follicular epithelium, resulting in impaction of keratinized cells within the follicular lumen; (2) increased sebaceous gland production of sebum; (3) proliferation of Propionibacterium acnes within the follicle; and (4) inflammation. Comedonal acne (Fig. 661-1), particularly of the central face, is frequently the first sign of pubertal maturation. At puberty, the sebaceus gland enlarges and sebum production increases in response to the increased activities of androgens of primarily adrenal origin. Most patients with acne do not have endocrine abnormalities. Hyperresponsiveness of the sebocyte to androgens is likely involved in determining the severity of acne in a given individual. Sebocytes and follicular keratinocytes contain 5α-reductase and 3β- and 17β-hydroxyl-steroid dehydrogenase, which are capable of metabolizing androgens. A significant number of women with acne (25-50%), particularly those with relatively mild papulopustular acne, note that their acne flares about 1 wk before menstruation.
Clinical Manifestations
Acne vulgaris is characterized by 4 basic types of lesions: open and closed comedones, papules, pustules (Fig. 661-2), and nodulocystic lesions (Fig. 661-3 and Table 661-1). One or more types of lesions may predominate. In its mildest form, which is often seen early in adolescence, lesions are limited to comedones on the central area of the face. Lesions may also involve the chest, upper back, and deltoid areas. A predominance of lesions on the forehead, particularly closed comedones, is often attributable to prolonged use of greasy hair preparations (pomade acne) (Fig. 661-4). Marked involvement on the trunk is most often seen in males. Lesions often heal with temporary postinflammatory erythema and hyperpigmentation. Pitted, atrophic, or hypertrophic scars may be interspersed, depending on the severity, depth, and chronicity of the process. Diagnosis of acne is rarely difficult, although flat warts, folliculitis, and other types of acne may be confused with acne vulgaris.
Table 661-1 CLASSIFICATION OF ACNE
| SEVERITY | DESCRIPTION |
|---|---|
| Mild | Comedones (noninflammatory lesions) are the main lesions. Papules and pustules may be present but are small and few in number (generally < 10). |
| Moderate | Moderate numbers of papules and pustules (10-40) and comedones (10-40) are present. Mild disease of the trunk may also be present. |
| Moderately severe | Numerous papules and pustules are present (40-100), usually with many comedones (40-100) and occasional larger, deeper nodular inflamed lesions (up to 5). Widespread affected areas usually involve the face, chest, and back. |
| Severe | Nodulocystic acne and acne conglobata with many large, painful nodular or pustular lesions are present, along with many smaller papules, pustules, and comedones. |
From James WD: Clinical practice: acne, N Engl J Med 352:1463–1472, 2005.
Treatment
No evidence shows that early treatment, with the exception of isotretinoin, alters the course of acne. Acne can be controlled and severe scarring prevented by judicious maintenance therapy that is continued until the disease process has abated spontaneously. Therapy must be individualized and aimed at preventing microcomedone formation through reduction of follicular hyperkeratosis, sebum production, the P. acnes population in follicular orifices, and free fatty acid production. Initial control takes at least 6-8 wk, depending on the severity of the acne (Table 661-2 and Fig 661-5). It is also important to address the potentially severe emotional impact of acne on adolescents.
Table 661-2 TYPICAL TREATMENT REGIMENS FOR ACNE
COMEDONAL ACNE
MILD PAPULOPUSTULAR ACNE
SEVERE PAPULOPUSTULAR OR NODULAR ACNE
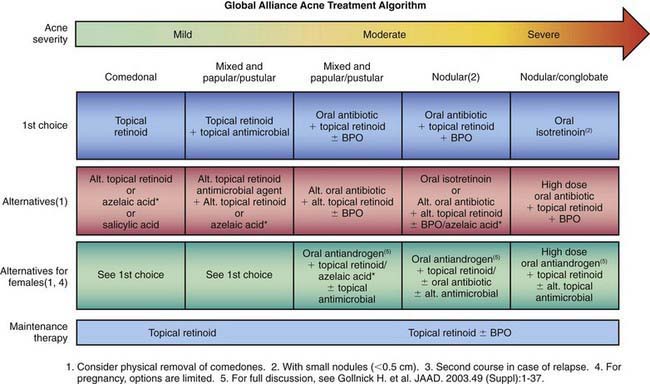
Figure 661-5 Acne treatment algorithm, BPO, benzoyl peroxide.
(From Thiboutot D, Gollnick H; Global Alliance to Improve Acne, et al: New insights into the management of acne: an update from the global alliance to improve outcomes in acne, J Am Acad Dermatol 60:S1–S50, 2009.)







