Chapter 623 Abnormalities of the Optic Nerve
Optic Nerve Hypoplasia
Optic nerve hypoplasia is a principal feature of septo-optic dysplasia of de Morsier, a developmental disorder characterized by the association of anomalies of the midline structures of the brain with hypoplasia of the optic nerves, optic chiasm, and optic tracts; typically noted are agenesis of the septum pellucidum, partial or complete agenesis of the corpus callosum, and malformation of the fornix, with a large chiasmatic cistern. Patients can have hypothalamic abnormalities and endocrine defects ranging from panhypopituitarism to isolated deficiency of growth hormone, hypothyroidism, or diabetes insipidus. Neonatal hypoglycemia and seizures are important presenting signs in affected infants (Chapter 585).
Optic Nerve Coloboma
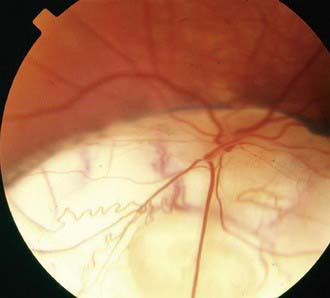
Optic nerve colobomas can be unilateral or bilateral. The visual acuity can range from normal to complete blindness. The coloboma develops secondary to incomplete closure of the embryonic fissure. The defect can produce a partial or total excavation of the optic disc (Fig. 623-1) Chorioretinal and iris colobomas can also occur. Optic nerve colobomas may be seen in a multitude of ocular and systemic abnormalities including the CHARGE association (coloboma, heart disease, atresia choanae, retarded growth and development and/or central nervous system anomalies, genetic anomalies and/or hypogonadism, ear anomalies and/or deafness).
 of involved eyes. Morning glory disc anomaly has been associated with basal encephalocele in patients with midfacial anomalies. Abnormalities of the carotid circulation can also be seen in patients with morning glory anomaly. Moyamoya disease is a well-described associated finding.
of involved eyes. Morning glory disc anomaly has been associated with basal encephalocele in patients with midfacial anomalies. Abnormalities of the carotid circulation can also be seen in patients with morning glory anomaly. Moyamoya disease is a well-described associated finding.


