Chapter 614 Abnormalities of Pupil and Iris
Aniridia
The term aniridia is a misnomer because iris tissue is usually present, although it is hypoplastic (Fig. 614-1). Two thirds of the cases are dominantly transmitted with a high degree of penetrance. The other 30% of cases are sporadic and are considered to be new mutations. The condition is bilateral in 98% of all patients, regardless of the means of transmission, and is found in approximately 1/50,000 persons.
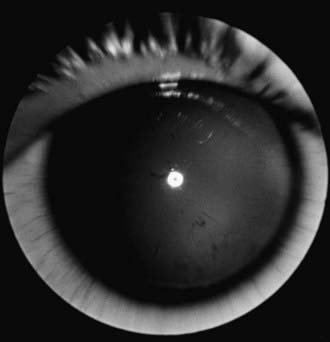
Figure 614-1 Aniridia with minimal iris tissue.
(From Nelson LB, Spaeth GL, Nowinski TS, et al: Aniridia: a review, Surv Ophthalmol 28:621–642, 1984.)
Aniridia is caused by a defect in the PAX6 gene on chromosome 11p13. The PAX6 gene is the master control gene for eye morphogenesis. Aniridia can be sporadic or familial. The familial form is autosomal dominant with complete penetrance but variable expressivity. Sporadic aniridia is associated with Wilms tumor in as many as 30% of cases (Chapter 493.1). The combination of aniridia and Wilms tumor represents a contiguous gene syndrome in which the adjacent PAX6 and Wilms tumor (WT1) genes are both deleted. Some deletions create the WAGR complex of Wilms tumor, aniridia, genitourinary malformations, and mental retardation. All children with sporadic aniridia should undergo chromosomal deletional analysis to exclude the possibility of Wilms tumor formation. Children who test positive for the deletion should undergo repeated abdominal ultrasonographic and clinical examinations. Wilms tumor has also been reported in patients with familial aniridia. Therefore, these patients should also undergo chromosomal analysis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


