Abnormal Umbilical Cord
Anne Kennedy, MD
DIFFERENTIAL DIAGNOSIS
Common
Umbilical Cord Cyst
Allantoic Cyst with Patent Urachus
Omphalomesenteric Duct Cyst
Pseudocyst
Cystic Wharton Jelly
Omphalocele (Mimic)
Physiologic Gut Herniation (Mimic)
Less Common
Cord Knot
Short Cord
Abnormal Cord Coiling
Cord Hematoma
Cord Thrombosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Cord assessment is an important part of all OB scans
Look at abdominal cord insertion site
Look at placental cord insertion site
Evaluate cord structure
Are the vessels normal?
Is the cord length normal?
Is there an appropriate degree of “twist” to the vessels?
Helpful Clues for Common Diagnoses
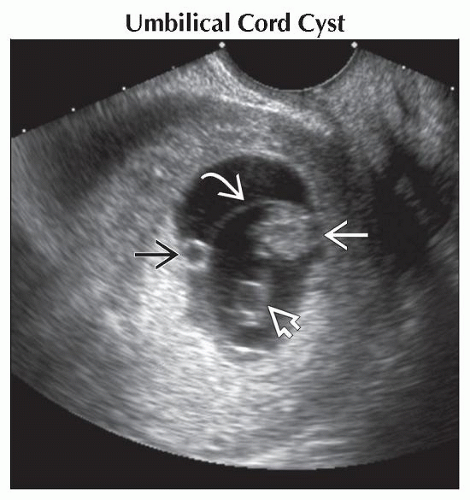
Umbilical Cord Cyst
Equally common at fetal & placental ends and in free loops of cord
May be paraxial (eccentric, do not displace vessels) or axial (centrally located and splay vessels)
Generally thin-walled, anechoic, often multiple
If echogenic content, consider intracystic hemorrhage, which may lead to cord compromise
May be true cysts (allantoic, omphalomesenteric duct cysts) or pseudocysts
Isolated cord cysts may spontaneously resolve with etiology never determined
Allantoic Cyst with Patent Urachus
Always near fetal insertion
May grow and compress cord
Allantoic cysts may be isolated or communicate with the urachus
Patent urachus: Cystic mass superior to, and communicating with, bladder
Obstructed bladder decompresses into urachus and base of cord
Omphalomesenteric Duct Cyst
2° to omphalomesenteric duct remnant
+ Abdominal wall anomalies
+ Intraabdominal mesenteric cysts
+ Other severe anomalies
Pseudocyst
Often associated with cystic Wharton jelly
May also be sequela of cord hematoma
Cystic Wharton Jelly
Mucoid degeneration of abnormal Wharton jelly
Innumerable small pseudocysts develop surrounding cord vessels
Likely to be associated with aneuploidy and syndromes
Omphalocele (Mimic)
Smooth mass protruding from central anterior abdominal wall with covering membrane
Umbilical cord inserts onto membrane, usually central but may be eccentric
Liver and small bowel most common contents (those with small bowel most likely to be confused with abnormal cord)
Physiologic Gut Herniation (Mimic)
Normal embryological developmental phenomenon
Bowel elongates, herniates into base of cord, rotates 270°, then returns to peritoneal cavity
Bowel returns to abdomen by 11.2 weeks
Should not extend more than 1 cm into base of cord
Never contains liver
Helpful Clues for Less Common Diagnoses
Cord Knot
True knot
Most common in monoamniotic twins
Rarely also seen in singletons
Risk factors include advanced maternal age, multiparity, long umbilical cords
May restrict flow → hypoxia, growth restriction
May occlude cord → fetal demise
Reported to lead to a 4-fold increase in fetal loss
False knot
Due to kinks in vessels, not a true knot
No known clinical significance
Short Cord
Average cord is 55 cm (range 35-80 cm)
Not possible to measure length prenatally, but short cord subjectively associated with fetus being “tethered”
Watch fetal movement in real time to assess for akinesia/arthrogryposis sequence
Associated with abruption/cord rupture
Abnormal Cord Coiling
Normal cord is helical, with up to 380 helices
Coiling is well established by 9 weeks and is thought to strengthen cord
Lack of normal coiling and length associated with fetal akinesia
Look at movements in real time
Assess joints for abnormal posture
Cord Hematoma
True cord hematoma is due to extravasation of blood into Wharton jelly surrounding cord vessels
Use Doppler to look for increased vascular resistance if large hematoma
May occur following invasive prenatal procedures
May also be seen adherent to cord secondary to intra-amniotic bleeding from any cause
Cord Thrombosis
Look for hypoechoic material distending vessels on grayscale images
Lack of flow on color or power Doppler
Venous thrombosis is a cause of sudden fetal demise
Most cases with surviving fetuses are reported as pathological finding after emergency delivery for distress in labor
Umbilical vein varix is a risk factor
May occur following invasive prenatal procedures, especially if large hematoma compresses vessels
May occur in association with large cord cysts, particularly at placental end of cord
Other Essential Information
Cord embryology
Early connecting stalk connects the embryo to the chorion
Allantois forms from caudal end of yolk sac
Cord formed from fusion of allantois and connecting stalk
Allantois functions as primitive bladder and early blood forming organ
Persistent segments of allantois are termed urachal remnants
Urachus serves as “pop-off valve” to decompress bladder if outlet obstruction
Allantois involutes to become median umbilical ligament
Multiple umbilical cord cysts associated with 7.6x increased risk of poor outcome
Straight cords with few or absent helices are associated with adverse fetal outcomes
Image Gallery
 Transvaginal ultrasound shows the yolk sac
 outside the amnion outside the amnion  that contains the embryo that contains the embryo  and developing cord. A cord cyst and developing cord. A cord cyst  is seen. This resolved spontaneously, and the infant was normal at birth. is seen. This resolved spontaneously, and the infant was normal at birth.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|