Inadequate cervical dilation or fetal descent:
Protracted labor—slow progress
Arrested labor—no progress
Inadequate expulsive effort—ineffective pushing
Fetopelvic disproportion:
Excessive fetal size
Inadequate pelvic capacity
Malpresentation or position of the fetus
Ruptured membranes without labor
 Dystocia Descriptors
Dystocia Descriptors
Abnormalities that are shown in Table 23-1 often interact in concert to produce dysfunctional labor. Commonly used expressions today such as cephalopelvic disproportion and failure to progress are used to describe ineffective labors. Of these, cephalopelvic disproportion is a term that came into use before the 20th century to describe obstructed labor resulting from disparity between the fetal head size and maternal pelvis. But the term originated at a time when the main indication for cesarean delivery was overt pelvic contracture due to rickets (Olah, 1994). Such absolute disproportion is now rare, and most cases result from malposition of the fetal head within the pelvis (asynclitism) or from ineffective uterine contractions. True disproportion is a tenuous diagnosis because two thirds or more of women undergoing cesarean delivery for this reason subsequently deliver even larger newborns vaginally. A second phrase, failure to progress in either spontaneous or stimulated labor, has become an increasingly popular description of ineffectual labor. This term reflects lack of progressive cervical dilatation or lack of fetal descent. Neither of these two expressions is specific. Terms presented in Table 23-2 and their diagnostic criteria more precisely describe abnormal labor.
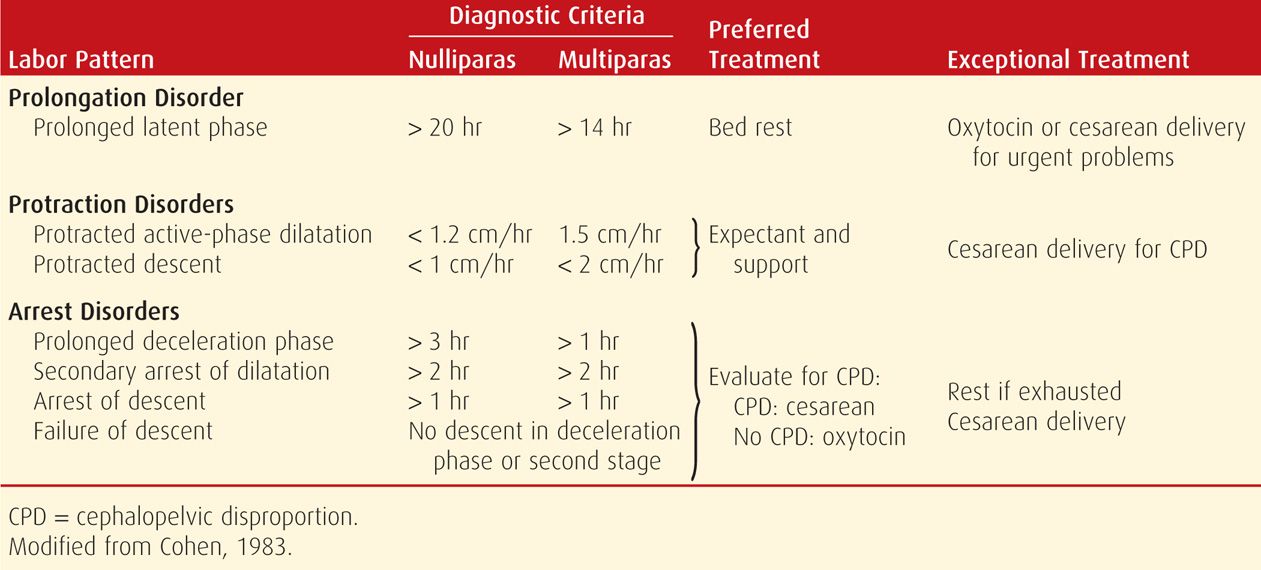
TABLE 23-2. Abnormal Labor Patterns, Diagnostic Criteria, and Methods of Treatment
 Mechanisms of Dystocia
Mechanisms of Dystocia
Dystocia as described by Williams (1903) in the first edition of this text is still true today. Figure 23-1 demonstrates the mechanical process of labor and potential obstacles. The cervix and lower uterus are shown at the end of pregnancy and at the end of labor. At the end of pregnancy, the fetal head, to traverse the birth canal, must encounter a relatively thick lower uterine segment and undilated cervix. The uterine fundus muscle is less developed and presumably less powerful. Uterine contractions, cervical resistance, and the forward pressure exerted by the leading fetal part are the factors influencing the progress of first-stage labor.
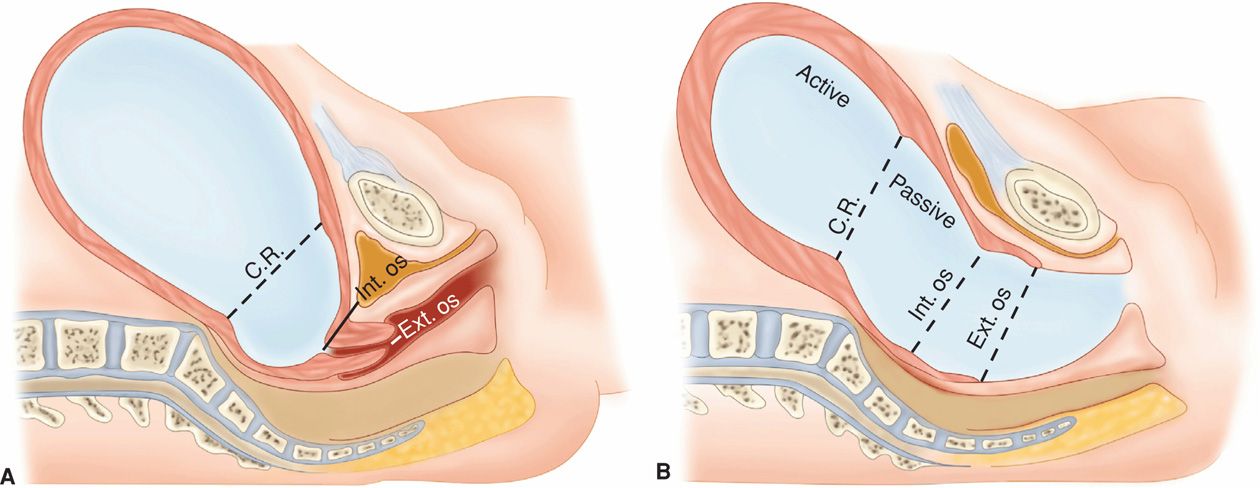
FIGURE 23-1 Diagrams of the birth canal. A. At the end of pregnancy. B. During the second-stage of labor, showing formation of the birth canal. C.R. = contraction ring; Int. = internal; Ext = external. (Adapted from Williams, 1903.)
As also shown in Figure 23-1B, after complete cervical dilatation, the mechanical relationship between the fetal head size and position and the pelvic capacity, namely fetopelvic proportion, becomes clearer as the fetus descends. Because of this, abnormalities in fetopelvic proportions become more apparent once the second stage is reached.
Uterine muscle malfunction can result from uterine overdistention or obstructed labor or both. Thus, ineffective labor is generally accepted as a possible warning sign of fetopelvic disproportion. Although artificial separation of labor abnormalities into pure uterine dysfunction and fetopelvic disproportion simplifies classification, it is an incomplete characterization because these two abnormalities are so closely interlinked. Indeed, according to the American College of Obstetricians and Gynecologists (2013), the bony pelvis rarely limits vaginal delivery. In the absence of objective means of precisely distinguishing these two causes of labor failure, clinicians must rely on a trial of labor to determine if labor can be successful in effecting vaginal delivery.
 Revised Dystocia Diagnosis
Revised Dystocia Diagnosis
In 2009, the total cesarean delivery rate for all births in the United States reached a record high of 32.9 percent (Martin, 2011). This was the 13th consecutive year in which the cesarean rate increased, and it represented a nearly 60-percent increase compared with 20.7 percent in 1996. The 2010 rate of 32.8 percent could suggest that this long trend of increasing cesarean rates may now be moderating (Martin, 2012). Given that many repeat cesarean deliveries are performed after primary operations for dystocia, it is estimated that 60 percent of all cesarean deliveries in the United States are ultimately attributable to the diagnosis of abnormal labor (American College of Obstetricians and Gynecologists, 2013).
To address this increasing cesarean delivery rate, a workshop was convened by the National Institute of Child Health and Human Development (NICHD) and the American College of Obstetricians and Gynecologists (Spong, 2012). The workshop recommended new definitions for arrest of labor progress to prevent unnecessary first cesarean deliveries. Specifically, it concluded that “adequate time for normal latent and active phases of the first stage and for the second stage should be allowed as long as the maternal and fetal conditions permit. The adequate time for each of these stages appears to be longer than traditionally estimated.” The implication of this viewpoint is that changing the diagnostic criteria of abnormal labor will reduce the excessive cesarean birth rate. Shown in Table 23-3 is a synopsis of some of these workshop recommendations for revised labor management criteria. According to the workshop, these definitions “vary somewhat from published criteria and are recommended in recognition of more recent findings regarding labor progress that challenge our long-held practices based on the Friedman curve.”
TABLE 23-3. Evidence for Adequate and Arrested Labor
Arrest of labor: “… the diagnosis of arrest of labor should not be made until adequate time has elapsed.”
Adequate labor: “… includes greater than 6 cm dilation with membrane rupture and 4 or more hours of adequate contractions (e.g., greater than 200 Montevideo units) or 6 hours or more if contractions inadequate with no cervical change. … ”
Second-stage labor: “… no progress for more than 4 hours in nulliparous women with an epidural, more than 3 hours in nulliparous women without an epidural. … ”
“No cesarean before these time limits … in the presence of reassuring maternal and fetal status.”
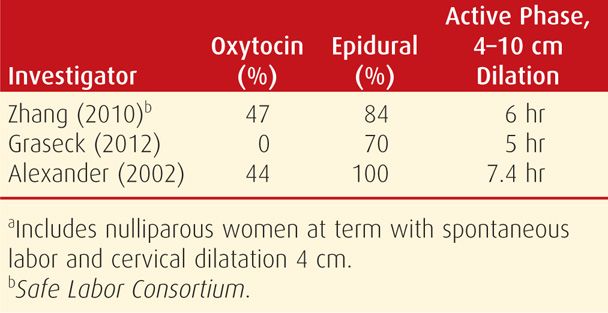
These proposed new criteria listed in Table 23-3 for normal, and therefore also abnormal labor, were heavily dependent on results of the NICHD-sponsored Safe Labor Consortium and on an NICHD-sponsored report on second-stage labor duration (Rouse, 2009; Zhang, 2010). Shown in Table 23-4 is a comparison of active labor phase duration in the Safe Labor Consortium compared with other contemporary reports. It is important to note that almost half of the Consortium cohort received oxytocin and 84 percent had received epidural analgesia—both factors associated with longer active-phase labor. Indeed, cases using oxytocin and epidural analgesia in the studies of Graseck (2012) and Alexander (2002) had similar active-labor phase durations to those from the Consortium. Importantly, all these reports were based on contemporary obstetrical practices.
TABLE 23-4. Duration of Active Phase Labor: Comparison in Contemporary Reportsa
The Safe Labor Consortium report by Zhang and associates (2010) was a multicenter retrospective study using abstracted 2002 to 2008 data from electronic medical records in 19 hospitals across the United States. One purpose of this study was to analyze labor patterns and develop contemporary criteria for labor progress in nulliparas. Shown in Figure 23-2 is a synopsis of the study cohort, which formed the basis of the proposed new criteria for labor progress. Importantly, all women with cesarean delivery were excluded as were all of those with compromised newborn infants. Because of these major exclusions, the pattern of labor now defined as normal is problematic given that only women who achieved vaginal birth with a normal infant outcome were included. It is also problematic to conclude that these revised labor criteria will reduce the cesarean rate when the overall rate in the Safe Labor Consortium was 30.5 percent using the newly proposed first-stage labor intervals. The authors of a report from the Maternal Fetal Medicine Units Network of the NICHD analyzed labor management practices in 8546 women undergoing primary cesarean delivery for dystocia in a wide cross section of hospitals in the United States (Alexander, 2003). Approximately 92 percent of the cesareans for dystocia were performed in the active phase of labor defined as ≥ 4 cm cervical dilatation. The median admission to delivery interval was 17 hours, and the median cervical dilation was 6 cm before the dystocia diagnosis in women in active-phase labor. Oxytocin was used in 90 percent of women diagnosed with dystocia. It was concluded that bona-fide efforts were being made in contemporary practice to achieve active labor before diagnosing dystocia leading to cesarean delivery.
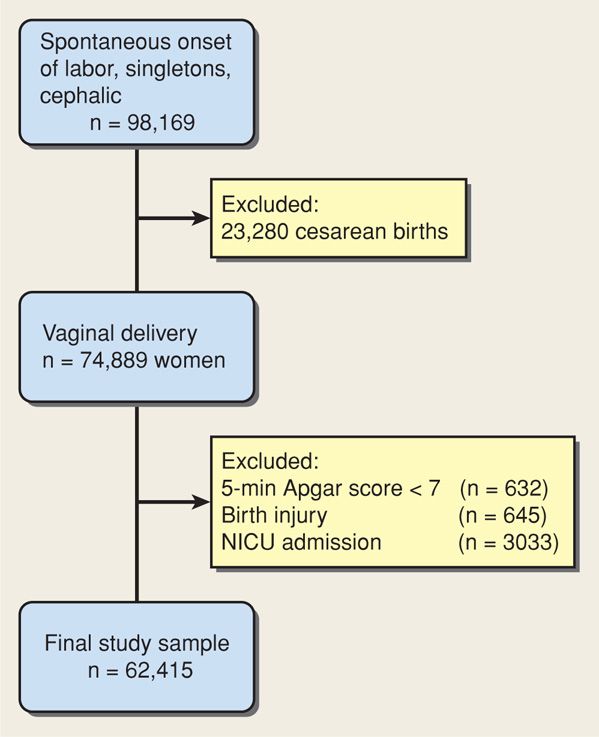
FIGURE 23-2 Study cohort for the analysis of spontaneous labor in the Safe Labor Consortium. NICU = neonatal intensive care unit. (Data from Zhang, 2010.)
The report by Rouse and colleagues (2009) on second-stage labor was a secondary analysis of 4126 nulliparous women who reached the second stage during a randomized trial to study fetal pulse oximetry. Of the 360 women—9 percent—whose second stage was > 3 hours, 95 percent had received epidural analgesia. A third of these 360 women—3.5 percent of the whole cohort—had a second stage > 4 hours. The results of this study were interpreted as support for extending the duration of the second stage in nulliparas to beyond the current recommended 3 hours when epidural analgesia is used (American College of Obstetricians and Gynecologists, 2013). The investigators concluded that a fetus born after a > 3-hour second stage had a higher—albeit still low—neonatal intensive care unit (NICU) admission rate and a low risk for brachial plexus injury (Rouse, 2009).
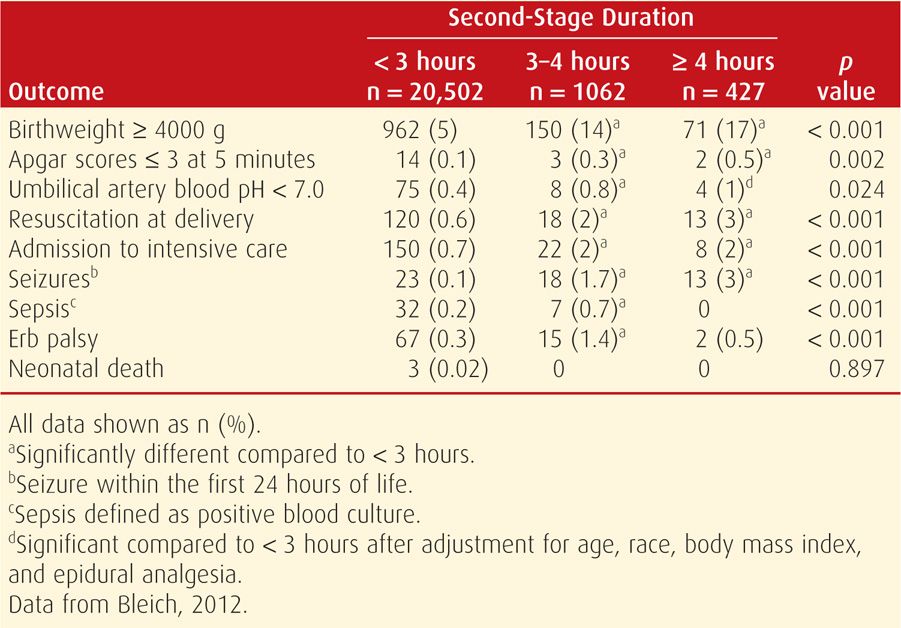
These latter results are in contrast to those associated with prolonged second-stage labors at Parkland Hospital (Bleich, 2012). This study included 21,991 women of whom 7 percent had a second-stage labor > 3 hours. Most of the 2 percent of women reaching 4 hours in the second stage had been given epidural analgesia and were awaiting cesarean delivery that was decided on at the 3-hour time point. Typically, oxytocin had been discontinued, and they also had reassuring fetal heart rate tracings that permitted temporization awaiting operative space. Thus, such prolonged second stages were unintentional in that further efforts to effect vaginal delivery were not made. Despite these caveats, virtually every adverse infant outcome analyzed increased significantly when the second stage exceeded 3 hours in women with labor epidural analgesia (Table 23-5).
TABLE 23-5. Neonatal Outcomes in Relation to Second-Stage Labor Duration
We conclude that at this time, an improved definition of the adequacy of a trial of labor before diagnosing dystocia remains an elusive goal. The newly proposed criteria for first-stage labor are already in use in contemporary practice, and thus they are unlikely to have much impact on the cesarean delivery rate for abnormal labor. Importantly, the purported safety of the proposed new criteria for second-stage labor management should be viewed with caution until more published experiences accrue.
ABNORMALITIES OF THE EXPULSIVE FORCES
Cervical dilatation and propulsion and expulsion of the fetus are brought about by contractions of the uterus, which are reinforced during the second stage by voluntary or involuntary muscular action of the abdominal wall—“pushing.” The diagnosis of uterine dysfunction in the latent phase is difficult and sometimes can be made only in retrospect (Chap. 22, p. 446). Women who are not yet in active labor commonly are erroneously treated for uterine dysfunction.
Beginning in the 1960s, there have been at least three significant advances in the treatment of uterine dysfunction. First is the realization that undue labor prolongation may contribute to maternal and perinatal morbidity and mortality rates. Second, dilute intravenous infusion of oxytocin is used for treatment of certain types of uterine dysfunction. Last, cesarean delivery is selected rather than difficult midforceps delivery when oxytocin fails or its use is inappropriate.
 Types of Uterine Dysfunction
Types of Uterine Dysfunction
Reynolds and coworkers (1948) emphasized that uterine contractions of normal labor are characterized by a gradient of myometrial activity. These forces are greatest and last longest at the fundus—considered fundal dominance—and they diminish toward the cervix. Caldeyro-Barcia and colleagues (1950) from Montevideo, Uruguay, inserted small balloons into the myometrium at various levels (Chap. 24, p. 498). They reported that in addition to a gradient of activity, there was a time differential in the onset of the contractions in the fundus, mid-zone, and lower uterine segments. Larks (1960) described the stimulus as starting in one cornu and then several milliseconds later in the other. The excitation waves then join and sweep over the fundus and down the uterus. Normal spontaneous contractions often exert pressures approximating 60 mm Hg (Hendricks, 1959). Even so, the Montevideo group ascertained that the lower limit of contraction pressure required to dilate the cervix is 15 mm Hg.
From these observations, it is possible to define two types of uterine dysfunction. In the more common hypotonic uterine dysfunction, there is no basal hypertonus and uterine contractions have a normal gradient pattern (synchronous), but pressure during a contraction is insufficient to dilate the cervix. In the second type, hypertonic uterine dysfunction or incoordinate uterine dysfunction, either basal tone is elevated appreciably or the pressure gradient is distorted. Gradient distortion may result from more forceful contraction of the uterine midsegment than the fundus or from complete asynchrony of the impulses originating in each cornu or a combination of these two.
 Active-Phase Disorders
Active-Phase Disorders
Labor abnormalities are divided into either a slower-than-normal progress—protraction disorder—or a complete cessation of progress—arrest disorder. A woman must be in the active phase of labor with cervical dilatation to at least 3 to 4 cm to be diagnosed with either of these. Handa and Laros (1993) diagnosed active-phase arrest, defined as no dilatation for 2 hours or more, in 5 percent of term nulliparas. This incidence has not changed since the 1950s (Friedman, 1978). Inadequate uterine contractions, defined as less than 180 Montevideo units, calculated as shown in Figure 23-3, were diagnosed in 80 percent of women with active-phase arrest.
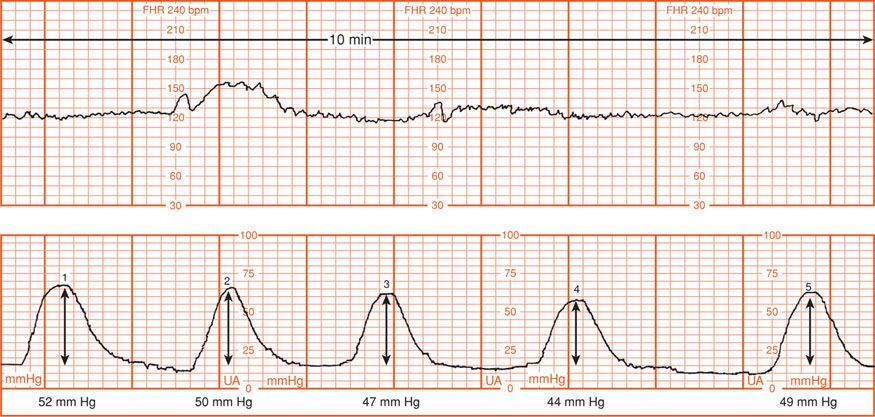
FIGURE 23-3 Montevideo units are calculated by subtracting the baseline uterine pressure from the peak contraction pressure for each contraction in a 10-minute window and adding the pressures generated by each contraction. In the example shown, there were five contractions, producing pressure changes of 52, 50, 47, 44, and 49 mm Hg, respectively. The sum of these five contractions is 242 Montevideo units.
Protraction disorders are less well described, and the time necessary before diagnosing slow progress is undefined. The World Health Organization (1994) has proposed a labor management partograph in which protraction is defined as less than 1 cm/hr cervical dilatation for a minimum of 4 hours. Criteria for the diagnosis of protraction and arrest disorders have been recommended by the American College of Obstetricians and Gynecologists (2013). These criteria were adapted from those of Cohen and Friedman (1983), shown in Table 23-2.
Hauth and coworkers (1986, 1991) reported that when labor is effectively induced or augmented with oxytocin, 90 percent of women achieve 200 to 225 Montevideo units, and 40 percent achieve at least 300 Montevideo units. These results suggest that there are certain minimums of uterine activity that should be achieved before performing cesarean delivery for dystocia. Accordingly, the American College of Obstetricians and Gynecologists (2013) has suggested that before the diagnosis of first-stage labor arrest is made, specific criteria should be met. First, the latent phase has been completed, and the cervix is dilated 4 cm or more. Also, a uterine contraction pattern of 200 Montevideo units or more in a 10-minute period has been present for 2 hours without cervical change. Rouse and associates (1999) have challenged the “2-hour rule” on the grounds that a longer time, that is, at least 4 hours, is necessary before concluding that the active phase of labor has failed. We agree.
 Second-Stage Disorders
Second-Stage Disorders
As discussed in Chapter 21 (p. 415), fetal descent largely follows complete dilatation. Moreover, the second stage incorporates many of the cardinal movements necessary for the fetus to negotiate the birth canal. Accordingly, disproportion of the fetus and pelvis frequently becomes apparent during second-stage labor.
Until recently, there have been largely unquestioned second-stage rules that limited its duration. These rules were established in American obstetrics by the beginning of the 20th century. They stemmed from concerns about maternal and fetal health, likely regarding infection, and led to difficult forceps operations. The second stage in nulliparas was limited to 2 hours and extended to 3 hours when regional analgesia was used. For multiparas, 1 hour was the limit, extended to 2 hours with regional analgesia.
Cohen (1977) investigated the fetal effects of second-stage labor length at Beth Israel Hospital. He included 4403 term nulliparas in whom electronic fetal heart rate monitoring was performed. The neonatal mortality rate was not increased in women whose second-stage labor exceeded 2 hours. Epidural analgesia was used commonly, and this likely accounted for the large number of pregnancies with a prolonged second stage. These data influenced decisions to permit an additional hour for the second stage when regional analgesia is used.
Menticoglou and coworkers (1995a,b) challenged the prevailing dictums on second-stage duration. These arose because of grave neonatal injuries associated with forceps rotations to shorten second-stage labor. As a result, they allowed a longer second stage to decrease the operative vaginal delivery rate. Between 1988 and 1992, second-stage labor exceeded 2 hours in a fourth of 6041 nulliparas at term. Labor epidural analgesia was used in 55 percent. The length of the second stage, even in those lasting up to 6 hours or more, was not related to neonatal outcome. These results were attributed to careful use of electronic monitoring and scalp pH measurements. These investigators concluded that there is no compelling reason to intervene with a possibly difficult forceps or vacuum extraction because a certain number of hours have elapsed. They observed, however, that after 3 hours in the second stage, delivery by cesarean or other operative method increased progressively. By 5 hours, the prospects for spontaneous delivery in the subsequent hour are only 10 to 15 percent.
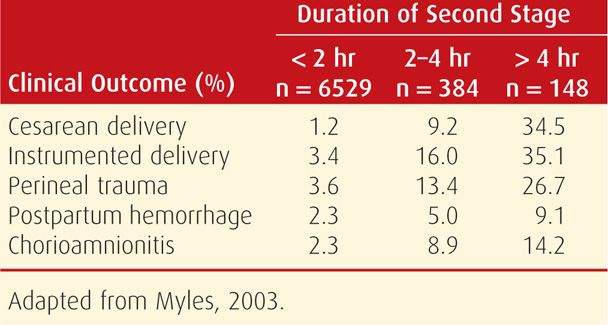
Adverse maternal outcomes, however, are increased with prolonged second-stage labor. Myles and Santolaya (2003) analyzed both the maternal and neonatal consequences of this in 7818 women in Chicago between 1996 and 1999. Adverse maternal outcomes in relation to the duration of second-stage labor were increased as shown in Table 23-6. Neonatal mortality and morbidity rates were not related to the length of the second stage.
TABLE 23-6. Clinical Outcomes in Relation to the Duration of Second-Stage Labor
Relationship between First- and Second-Stage Labor Duration
It is possible that prolonged first-stage labor presages that with the second stage. Nelson and associates (2013) studied the relationships between the lengths of the first and second stages of labor in 12,523 nulliparous women at term delivered at Parkland Hospital. The length of the second stage significantly increased concomitantly with increasing length of the first stage. The 95th percentile was 15.6 and 2.9 hours for the first and second stages, respectively. Women with first stages lasting longer than 15.6 hr (> 95th percentile) had a 16.3 percent rate of a second-stage labor lasting 3 hr (95th percentile) compared with a 4.5-percent rate in women with first-stages labors lasting less than the 95th percentile.
Maternal Pushing Efforts
With full cervical dilatation, most women cannot resist the urge to “bear down” or “push” each time the uterus contracts (Chap. 22, p. 451). The combined force created by contractions of the uterus and abdominal musculature propels the fetus downward. Bloom and colleagues (2006) studied effects of actively coaching expulsive efforts. They reported that although the second stage was slightly shorter in coached women, there were no other maternal advantages.
At times, force created by abdominal musculature is compromised sufficiently to slow or even prevent spontaneous vaginal delivery. Heavy sedation or regional analgesia may reduce the reflex urge to push and may impair the ability to contract abdominal muscles sufficiently. In other instances, the inherent urge to push is overridden by the intense pain created by bearing down. Two approaches to second-stage pushing in women with epidural analgesia have yielded contradictory results. The first advocates pushing forcefully with contractions after complete dilation, regardless of the urge to push. With the second, analgesia infusion is stopped and pushing begun only after the woman regains the sensory urge to bear down. Fraser and coworkers (2000) found that delayed pushing reduced difficult operative deliveries, whereas Manyonda and associates (1990) reported the opposite. Hansen and colleagues (2002) randomly assigned 252 women with epidural analgesia to one of the two approaches. There were no adverse maternal or neonatal outcomes linked to delayed pushing despite significantly prolonging second-stage labor. Plunkett and coworkers (2003), in a similar study, confirmed these findings.
 Fetal Station at Onset of Labor
Fetal Station at Onset of Labor
Descent of the leading edge of the presenting part to the level of the ischial spines (0 station) is defined as engagement. Friedman and Sachtleben (1965, 1976) reported a significant association between higher station at the onset of labor and subsequent dystocia. Handa and Laros (1993) found that fetal station at the time of arrested labor was also a risk factor for dystocia. Roshanfekr and associates (1999) analyzed fetal station in 803 nulliparous women at term in active labor. At admission, the third with the fetal head at or below 0 station had a 5-percent cesarean delivery rate. This is compared with a 14-percent rate for those with higher stations. The prognosis for dystocia, however, was not related to incrementally higher fetal head stations above the pelvic midplane (0 station). Importantly, 86 percent of nulliparous women without fetal head engagement at diagnosis of active labor delivered vaginally. These observations apply especially for parous women because the head typically descends later in labor.
 Reported Causes of Uterine Dysfunction
Reported Causes of Uterine Dysfunction
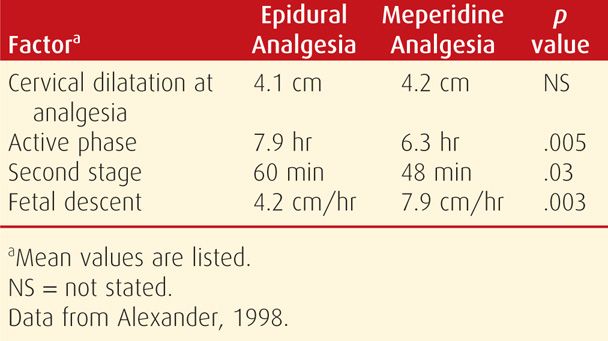
Epidural Analgesia
Various labor factors have been implicated as causes of uterine dysfunction. Of these, epidural analgesia can slow labor (Sharma, 2000). As shown in Table 23-7, epidural analgesia has been associated with lengthening of both first- and second-stage labor and with slowing of the rate of fetal descent. This is documented further in Chapter 25 (p. 515).
TABLE 23-7. Effect of Epidural Analgesia on the Progress of Labor in 199 Nulliparous Women Delivered Spontaneously at Parkland Hospital
Chorioamnionitis
Because of the association of prolonged labor with maternal intrapartum infection, some clinicians have suggested that infection itself contributes to abnormal uterine activity. Satin and coworkers (1992) studied the effects of chorioamnionitis on oxytocin stimulation in 266 pregnancies. Infection diagnosed late in labor was found to be a marker of cesarean delivery performed for dystocia, whereas this was not a marker in women diagnosed as having chorioamnionitis early in labor. Specifically, 40 percent of women developing chorioamnionitis after requiring oxytocin for dysfunctional labor later required cesarean delivery for dystocia. It is likely that uterine infection in this clinical setting is a consequence of dysfunctional, prolonged labor rather than a cause of dystocia.
Maternal Position During Labor
Advocacy for recumbency or ambulation during labor has vacillated. Proponents of walking report it to shorten labor, decrease rates of oxytocin augmentation, decrease the need for analgesia, and lower the frequency of operative vaginal delivery (Flynn, 1978; Read, 1981). But other observations do not support this. According to Miller (1983), the uterus contracts more frequently but with less intensity with the mother lying on her back rather than on her side. Conversely, contraction frequency and intensity have been reported to increase with sitting or standing. Lupe and Gross (1986) concluded, however, that there is no conclusive evidence that upright maternal posture or ambulation improves labor. They reported that women preferred to lie on their side or sit in bed. Few chose to walk, fewer to squat, and none wanted the knee-chest position. They tended to assume fetal positions in later labor. Most women enthusiastic about ambulation returned to bed when active labor began (Carlson, 1986; Williams, 1980).
Bloom and colleagues (1998) conducted a randomized trial to study the effects of walking during first-stage labor. In 1067 women with uncomplicated term pregnancies delivered at Parkland Hospital, these investigators reported that ambulation did not affect labor duration. Ambulation did not reduce the need for analgesia, nor was it harmful to the perinate. Because of these observations, we give women without complications the option to select either recumbency or supervised ambulation during labor. This policy is in agreement with the American College of Obstetricians and Gynecologists (2013), which has concluded that ambulation in labor is not harmful, and mobility may result in greater comfort.
Birthing Position in Second-Stage Labor
Considerable interest has been shown in alternative second-stage labor birth positions and their effect on labor. Gupta and Hofmeyr (2004) in their Cochrane database review compared upright positions with supine or lithotomy positions. Upright positions included sitting in a “birthing chair,” kneeling, squatting, or resting with the back at a 30-degree elevation. With these positions, they found a 4-minute shorter interval to delivery, less pain, and a lower incidence both of nonreassuring fetal heart rate patterns and of operative vaginal delivery. There was, however, an increased rate of blood loss > 500 mL with the upright positions. Berghella and colleagues (2008) hypothesized that parity, less intense aortocaval compression, improved fetal alignment, and larger pelvic outlet diameters might explain these findings. In an earlier study, Russell (1969) described a 20- to 30-percent increase in the area of the pelvic outlet with squatting compared with that in the supine position. Finally, Babayer and associates (1998) cautioned that prolonged sitting or squatting during the second stage may cause common fibular nerve neuropathy.
Water Immersion
A birthing tub or bath has been advocated as a means of relaxation that may contribute to more efficient labor. Cluett and coworkers (2004) randomly assigned 99 laboring women at term in first-stage labor identified to have dystocia to immersion in a birthing pool or to oxytocin augmentation. Water immersion lowered the rate of epidural analgesia use but did not alter the rate of operative delivery. More infants of women in the immersion group were admitted to the NICU. These findings were similar to their subsequent Cochrane database review, except that NICU admission rates were not increased (Cluett, 2009).
Robertson and associates (1998) reported that immersion was not associated with chorioamnionitis or uterine infection. Moreover, Kwee and coworkers (2000) studied the effects of immersion in 20 women and reported that blood pressure decreased, whereas fetal heart rate was unaffected. Neonatal complications unique to underwater birth that have been described include drowning, hyponatremia, waterborne infection, cord rupture, and polycythemia (Austin, 1997; Pinette, 2004).
PREMATURELY RUPTURED MEMBRANES AT TERM
Membrane rupture at term without spontaneous uterine contractions complicates approximately 8 percent of pregnancies. Until recently, management generally included labor stimulation if contractions did not begin after 6 to 12 hours. This intervention evolved more than 50 years ago because of maternal and fetal complications due to chorioamnionitis (Calkins, 1952). Such routine intervention was the accepted practice until challenged by Kappy and colleagues (1979). These investigators reported excessive cesarean delivery in term pregnancies with ruptured membranes managed with labor stimulation compared with those expectantly managed.
Subsequent research included that of Hannah (1996) and Peleg (1999) and their associates, who enrolled a total of 5042 pregnancies with ruptured membranes in a randomized investigation. They measured the effects of induction versus expectant management and also compared induction using intravenous oxytocin with that using prostaglandin E2 gel. There were approximately 1200 pregnancies in each of the four study arms. They concluded that labor induction with intravenous oxytocin was the preferred management. This determination was based on significantly fewer intrapartum and postpartum infections in women whose labor was induced. There were no significant differences in cesarean delivery rates. Subsequent analysis by Hannah and coworkers (2000) indicated increased adverse outcomes when expectant management at home was compared with in-hospital observation. Mozurkewich and associates (2009) reported lower rates of chorioamnionitis, metritis, and NICU admissions for women with term ruptured membranes whose labors were induced compared with those managed expectantly. At Parkland Hospital, labor is induced soon after admission when ruptured membranes are confirmed at term. The benefit of prophylactic antibiotics in women with ruptured membranes before labor at term is unclear (Passos, 2012).
PRECIPITOUS LABOR AND DELIVERY
Labor can be too slow, but it also can be abnormally rapid. Precipitous labor and delivery is extremely rapid labor and delivery. It may result from an abnormally low resistance of the soft parts of the birth canal, from abnormally strong uterine and abdominal contractions, or rarely from the absence of painful sensations and thus a lack of awareness of vigorous labor.
According to Hughes (1972), precipitous labor terminates in expulsion of the fetus in < 3 hours. Using this definition, 89,047 live births—2 percent—were complicated by precipitous labor in the United States during 2006 (Martin, 2009). Despite this incidence, there is little published information concerning adverse effects.
 Maternal Effects
Maternal Effects
Precipitous labor and delivery seldom are accompanied by serious maternal complications if the cervix is effaced appreciably and compliant, if the vagina has been stretched previously, and if the perineum is relaxed. Conversely, vigorous uterine contractions combined with a long, firm cervix and a noncompliant birth canal may lead to uterine rupture or extensive lacerations of the cervix, vagina, vulva, or perineum. It is in these latter circumstances that the rare condition of amnionic-fluid embolism most likely develops (Chap. 41, p. 812).
Precipitous labor is frequently followed by uterine atony. The uterus that contracts with unusual vigor before delivery is likely to be hypotonic after delivery. Postpartum hemorrhage from uterine atony is discussed in Chapter 41 (p. 784).
Mahon and colleagues (1994) described 99 pregnancies delivered within 3 hours of labor onset. Short labors were defined as a rate of cervical dilatation of 5 cm/hr or faster for nulliparas and 10 cm/hr for multiparas. Such short labors were more common in multiparas who typically had contractions at intervals less than 2 minutes and were associated with placental abruption, meconium, postpartum hemorrhage, cocaine abuse, and low Apgar scores.
 Fetal and Neonatal Effects
Fetal and Neonatal Effects
Adverse perinatal outcomes from precipitous labor may be increased considerably for several reasons. The tumultuous uterine contractions, often with negligible intervals of relaxation, prevent appropriate uterine blood flow and fetal oxygenation. Resistance of the birth canal may rarely cause intracranial trauma. Acker and coworkers (1988) reported that Erb or Duchenne brachial palsy was associated with such labors in a third of cases (Chap. 33, p. 648). Finally, during an unattended birth, the newborn may fall to the floor and be injured, or it may need resuscitation that is not immediately available.
 Treatment
Treatment
Unusually forceful spontaneous uterine contractions are not likely to be modified to a significant degree by analgesia. The use of tocolytic agents such as magnesium sulfate is unproven in these circumstances. Use of general anesthesia with agents that impair uterine contractibility, such as isoflurane, is often excessively heroic. Certainly, any oxytocin agents being administered should be stopped immediately.
FETOPELVIC DISPROPORTION
 Pelvic Capacity
Pelvic Capacity
Fetopelvic disproportion arises from diminished pelvic capacity, excessive fetal size, or more usually both. Any contraction of the pelvic diameters that diminishes its capacity can create dystocia during labor. There may be a contraction of the pelvic inlet, the midpelvis, or the pelvic outlet, or a generally contracted pelvis may be caused by combinations of these. Normal pelvic dimension are additionally discussed in Chapter 2 (p. 32).
Contracted Inlet
The pelvic inlet usually is considered to be contracted if its shortest anteroposterior diameter is < 10 cm or if the greatest transverse diameter is < 12 cm. The anteroposterior diameter of the inlet is commonly approximated by manually measuring the diagonal conjugate, which is approximately 1.5 cm greater (Chap. 2, p. 33). Therefore, inlet contraction usually is defined as a diagonal conjugate < 11.5 cm.
Using clinical and at times, imaging pelvimetry, it is important to identify the shortest anteroposterior diameter through which the fetal head must pass. Occasionally, the body of the first sacral vertebra is displaced forward so that the shortest distance may actually be between this abnormal sacral promontory and the symphysis pubis.
Before labor, the fetal biparietal diameter has been shown to average from 9.5 to as much as 9.8 cm. Therefore, it might prove difficult or even impossible for some fetuses to pass through an inlet that has an anteroposterior diameter of less than 10 cm. Mengert (1948) and Kaltreider (1952), employing x-ray pelvimetry, demonstrated that the incidence of difficult deliveries is increased to a similar degree when either the anteroposterior diameter of the inlet is < 10 cm or the transverse diameter is < 12 cm. As expected, when both diameters are contracted, dystocia is much greater than when only one is contracted.
A small woman is likely to have a small pelvis, but she is also likely to have a small neonate. Thoms (1937) studied 362 nulliparas and found that the mean birthweight of their offspring was significantly lower—280 g—in women with a small pelvis than in those with a medium or large pelvis. In veterinary obstetrics, in most species, maternal size rather than paternal size is the important determinant of fetal size.
Normally, cervical dilatation is aided by hydrostatic action of the unruptured membranes or after their rupture, by direct application of the presenting part against the cervix (Fig. 21-7, p. 414). In contracted pelves, however, because the head is arrested in the pelvic inlet, the entire force exerted by the uterus acts directly on the portion of membranes that contact the dilating cervix. Consequently, early spontaneous rupture of the membranes is more likely.
After membrane rupture, absent pressure by the head against the cervix and lower uterine segment predisposes to less effective contractions. Hence, further dilatation may proceed very slowly or not at all. Cibils and Hendricks (1965) reported that the mechanical adaptation of the fetal passenger to the bony passage plays an important part in determining the efficiency of contractions. The better the adaptation, the more efficient the contractions. Thus, cervical response to labor provides a prognostic view of labor outcome in women with inlet contraction.
A contracted inlet also plays an important part in the production of abnormal presentations. In normal nulliparas, the presenting part at term commonly descends into the pelvic cavity before labor onset. When the inlet is contracted considerably or there is marked asynclitism, descent usually does not take place until after labor onset, if at all. Cephalic presentations still predominate, but the head floats freely over the pelvic inlet or rests more laterally in one of the iliac fossae. Accordingly, very slight influences may cause the fetus to assume other presentations. In women with contracted pelves, face and shoulder presentations are encountered three times more frequently, and the cord prolapses four to six times more often.
Contracted Midpelvis
This finding is more common than inlet contraction. It frequently causes transverse arrest of the fetal head, which potentially can lead to a difficult midforceps operation or to cesarean delivery.
The obstetrical plane of the midpelvis extends from the inferior margin of the symphysis pubis through the ischial spines and touches the sacrum near the junction of the fourth and fifth vertebrae (Chap. 2, p. 33). A transverse line theoretically connecting the ischial spines divides the midpelvis into anterior and posterior portions. The former is bounded anteriorly by the lower border of the symphysis pubis and laterally by the ischiopubic rami. The posterior portion is bounded dorsally by the sacrum and laterally by the sacrospinous ligaments, forming the lower limits of the sacrosciatic notch.
Average midpelvis measurements are as follows: transverse, or interischial spinous, 10.5 cm; anteroposterior, from the lower border of the symphysis pubis to the junction of S4–5, 11.5 cm; and posterior sagittal, from the midpoint of the interspinous line to the same point on the sacrum, 5 cm. The definition of midpelvic contractions has not been established with the same precision possible for inlet contractions. Even so, the midpelvis is likely contracted when the sum of the interspinous and posterior sagittal diameters of the midpelvis—normally, 10.5 plus 5 cm, or 15.5 cm—falls to 13.5 cm or less. This concept was emphasized by Chen and Huang (1982) in evaluating possible midpelvic contraction. There is reason to suspect midpelvic contraction whenever the interspinous diameter is < 10 cm. When it measures < 8 cm, the midpelvis is contracted.
Although there is no precise manual method of measuring midpelvic dimensions, a suggestion of contraction sometimes can be inferred if the spines are prominent, the pelvic sidewalls converge, or the sacrosciatic notch is narrow. Moreover, Eller and Mengert (1947) noted that the relationship between the intertuberous and interspinous diameters of the ischium is sufficiently constant that narrowing of the interspinous diameter can be anticipated when the intertuberous diameter is narrow. A normal intertuberous diameter, however, does not always exclude a narrow interspinous diameter.
Contracted Outlet
This finding usually is defined as an interischial tuberous diameter of 8 cm or less. The pelvic outlet may be roughly likened to two triangles, with the interischial tuberous diameter constituting the base of both. The sides of the anterior triangle are the pubic rami, and its apex is the inferoposterior surface of the symphysis pubis. The posterior triangle has no bony sides but is limited at its apex by the tip of the last sacral vertebra—not the tip of the coccyx. Diminution of the intertuberous diameter with consequent narrowing of the anterior triangle must inevitably force the fetal head posteriorly. Floberg and associates (1987) reported that outlet contractions were found in almost 1 percent of more than 1400 unselected nulliparas with term pregnancies. A contracted outlet may cause dystocia not so much by itself but by an often-associated midpelvic contraction. Outlet contraction without concomitant midplane contraction is rare.
Although the disproportion between the fetal head and the pelvic outlet is not sufficiently great to give rise to severe dystocia, it may play an important part in perineal tears. With increased narrowing of the pubic arch, the occiput cannot emerge directly beneath the symphysis pubis but is forced farther down upon the ischiopubic rami. The perineum, consequently, becomes increasingly distended and thus exposed to risk of laceration.
 Pelvic Fractures
Pelvic Fractures
Vallier (2012) reviewed experiences with pelvic fractures and pregnancy. Trauma from automobile collisions was the most common cause. Moreover, they note that fracture pattern, minor malalignment, and retained hardware are not absolute indications for cesarean delivery. A history of pelvic fracture warrants careful review of previous radiographs and possibly pelvimetry later in pregnancy.
 Estimation of Pelvic Capacity
Estimation of Pelvic Capacity
The techniques for clinical evaluation using digital examination of the bony pelvis during labor are described in detail in Chapter 2 (p. 32). Briefly, the examiner attempts to judge the anteroposterior diameter of the inlet—the diagonal conjugate, the interspinous diameter of the midpelvis, and the intertuberous distances of the pelvic outlet. A narrow pelvic arch of less than 90 degrees can signify a narrow pelvis. An unengaged fetal head can indicate either excessive fetal head size or reduced pelvic inlet capacity.
The value of radiologic imaging to assess pelvic capacity has also been examined. First, with x-ray pelvimetry alone, the prognosis for successful vaginal delivery in any given pregnancy cannot be established (Mengert, 1948). Thus, the American College of Obstetricians and Gynecologists (2009) considers x-ray pelvimetry to be of limited value in the management of labor with a cephalic presentation.
Advantages of pelvimetry with computed tomography (CT), such as that shown in Figure 23-4, compared with those of conventional x-ray pelvimetry include reduced radiation exposure, greater accuracy, and easier performance. With either method, costs are comparable, and x-ray exposure is small (Chap. 46, p. 934). Depending on the machine and technique employed, fetal doses with CT pelvimetry may range from 250 to 1500 mrad (Moore, 1989).
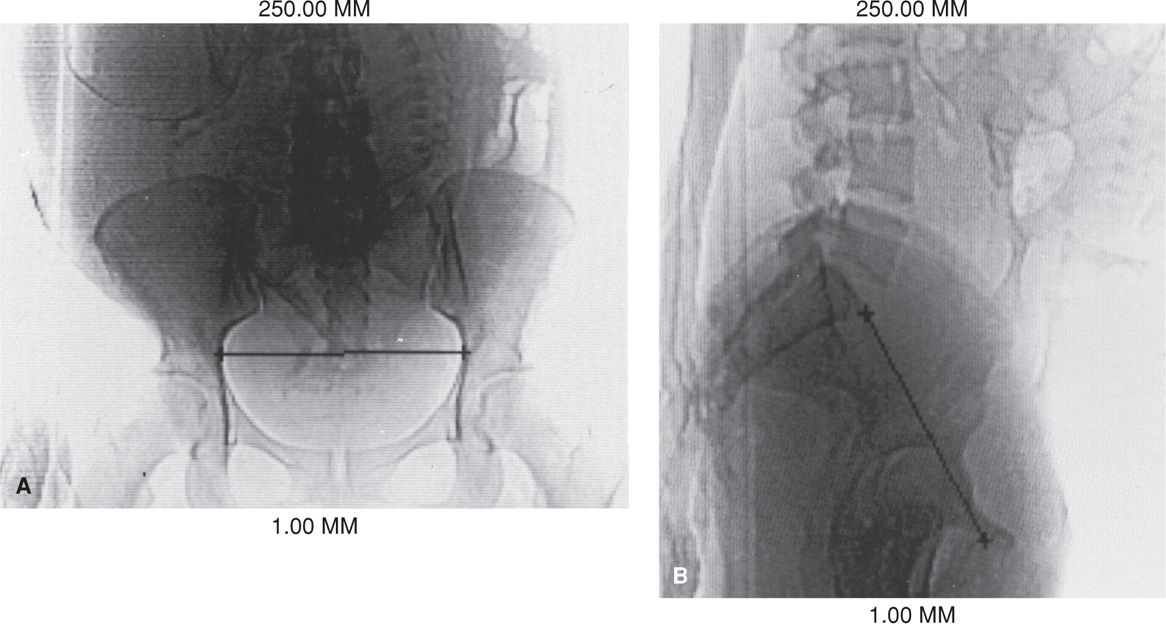
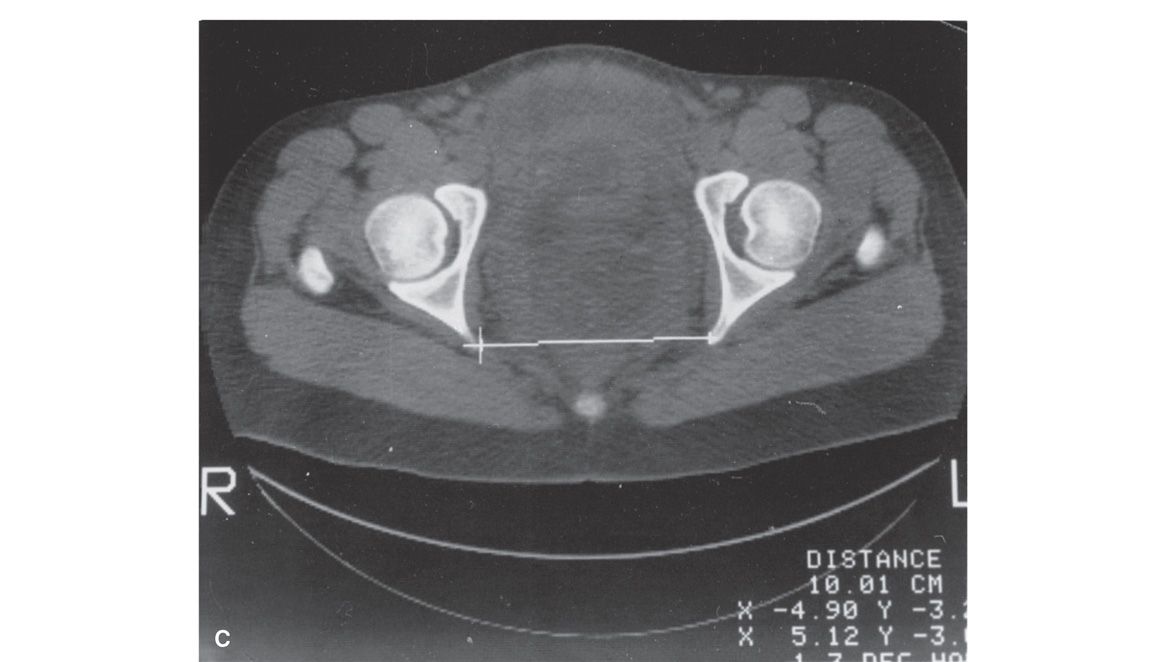
FIGURE 23-4 A. Anteroposterior view of a digital radiograph. Illustrated is the measurement of the transverse diameter of the pelvic inlet using an electronic cursor. The fetal body is clearly outlined. B. Lateral view of a digital radiograph. Illustrated are measurements of the anteroposterior diameters of the inlet using the electronic cursor. C. An axial computed tomographic section through the midpelvis. The level of the fovea of the femoral heads was ascertained from the anteroposterior digital radiograph because it corresponds to the level of the ischial spines. The interspinous diameter is measured using the electronic cursor. The total fetal radiation dose using these three exposures is approximately 250 mrad.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


