Background
Obesity and being overweight are becoming epidemic, and indeed, the proportion of such women of reproductive age has increased in recent times. Being overweight or obese prior to pregnancy is a risk factor for gestational diabetes mellitus, and increases the risk of adverse pregnancy outcome for both mothers and their offspring. Furthermore, the combination of gestational diabetes mellitus with obesity/overweight status may increase the risk of adverse pregnancy outcome attributable to either factor alone. Regular exercise has the potential to reduce the risk of developing gestational diabetes mellitus and can be used during pregnancy; however, its efficacy remain controversial. At present, most exercise training interventions are implemented on Caucasian women and in the second trimester, and there is a paucity of studies focusing on overweight/obese pregnant women.
Objective
We sought to test the efficacy of regular exercise in early pregnancy to prevent gestational diabetes mellitus in Chinese overweight/obese pregnant women.
Study Design
This was a prospective randomized clinical trial in which nonsmoking women age >18 years with a singleton pregnancy who met the criteria for overweight/obese status (body mass index 24≤28 kg/m 2 ) and had an uncomplicated pregnancy at <12 +6 weeks of gestation were randomly allocated to either exercise or a control group. Patients did not have contraindications to physical activity. Patients allocated to the exercise group were assigned to exercise 3 times per week (at least 30 min/session with a rating of perceived exertion between 12-14) via a cycling program begun within 3 days of randomization until 37 weeks of gestation. Those in the control group continued their usual daily activities. Both groups received standard prenatal care, albeit without special dietary recommendations. The primary outcome was incidence of gestational diabetes mellitus.
Results
From December 2014 through July 2016, 300 singleton women at 10 weeks’ gestational age and with a mean prepregnancy body mass index of 26.78 ± 2.75 kg/m 2 were recruited. They were randomized into an exercise group (n = 150) or a control group (n = 150). In all, 39 (26.0%) and 38 (25.3%) participants were obese in each group, respectively. Women randomized to the exercise group had a significantly lower incidence of gestational diabetes mellitus (22.0% vs 40.6%; P < .001). These women also had significantly less gestational weight gain by 25 gestational weeks (4.08 ± 3.02 vs 5.92 ± 2.58 kg; P < .001) and at the end of pregnancy (8.38 ± 3.65 vs 10.47 ± 3.33 kg; P < .001), and reduced insulin resistance levels (2.92 ± 1.27 vs 3.38 ± 2.00; P = .033) at 25 gestational weeks. Other secondary outcomes, including gestational weight gain between 25-36 gestational weeks (4.55 ± 2.06 vs 4.59 ± 2.31 kg; P = .9), insulin resistance levels at 36 gestational weeks (3.56 ± 1.89 vs 4.07 ± 2.33; P = .1), hypertensive disorders of pregnancy (17.0% vs 19.3%; odds ratio, 0.854; 95% confidence interval, 0.434–2.683; P = .6), cesarean delivery (except for scar uterus) (29.5% vs 32.5%; odds ratio, 0.869; 95% confidence interval, 0.494–1.529; P = .6), mean gestational age at birth (39.02 ± 1.29 vs 38.89 ± 1.37 weeks’ gestation; P = .5); preterm birth (2.7% vs 4.4%, odds ratio, 0.600; 95% confidence interval, 0.140–2.573; P = .5), macrosomia (defined as birthweight >4000 g) (6.3% vs 9.6%; odds ratio, 0.624; 95% confidence interval, 0.233–1.673; P = .3), and large-for-gestational-age infants (14.3% vs 22.8%; odds ratio, 0.564; 95% confidence interval, 0.284–1.121; P = .1) were also lower in the exercise group compared to the control group, but without significant difference. However, infants born to women following the exercise intervention had a significantly lower birthweight compared with those born to women allocated to the control group (3345.27 ± 397.07 vs 3457.46 ± 446.00 g; P = .049).
Conclusion
Cycling exercise initiated early in pregnancy and performed at least 30 minutes, 3 times per week, is associated with a significant reduction in the frequency of gestational diabetes mellitus in overweight/obese pregnant women. And this effect is very relevant to that exercise at the beginning of pregnancy decreases the gestational weight gain before the mid-second trimester. Furthermore, there was no evidence that the exercise prescribed in this study increased the risk of preterm birth or reduced the mean gestational age at birth.
Introduction
The global epidemics of overweight and obesity are leading health burdens worldwide; moreover, the proportion of overweight and obese women of reproductive age is increasing. Overweight and obesity are widely accepted to affect the entire pregnancy process and to constitute major risk factors for perinatal complications, such as gestational diabetes mellitus (GDM), hypertensive syndrome, fetal growth disorders, cesarean delivery, postoperative complications, wound infections, and deep vein thrombosis. Among them, GDM is a particular concern because of its own effects on other adverse pregnancy outcomes, such as preeclampsia, macrosomia, or cesarean delivery. Our previous study showed that overweight and obese pregnant women have a >2-fold increased risk of developing GDM compared with nonobese women. Furthermore, the combination of GDM and overweight or obesity aggravates the adverse pregnancy outcomes caused by either factor alone. Importantly, these poor outcomes also potentially impact the long-term health of both the mothers and their offspring. Thus, focusing on women who are overweight or obese before pregnancy and seeking ways to decrease their risk of GDM and other adverse pregnancy outcomes are of great importance.
As an important part of lifestyle interventions, exercise has received increasing attention from investigators worldwide. In nonpregnant subjects, the value of regular exercise for reducing the risk of type 2 diabetes and cardiovascular disease is well established. However, whether exercise is effective in reducing the risk of GDM and other adverse pregnancy outcomes is not clear because the few randomized controlled trials (RCTs) that investigated these topics showed conflicting results. Moreover, most of the current correlative researches were carried out on Caucasian women and few focus on overweight and obese pregnant women. In particular, most exercise training interventions are implemented in the second trimester. However, a recent meta-analysis including 29 RCTs with 11,487 pregnant women addressed that exercise could only play a role in preventing GDM in women with intervention <15 gestational weeks, whereas, among women with intervention afterward, it did not work. In addition, a quasiexperimental study of Chinese pregnant women pointed out that lifestyle intervention including exercise, diet, and weight-gain counseling from 8-12 gestational weeks could lower the risk of GDM.
Therefore, the objective of this study was to determine whether a program of regular exercise begun in early pregnancy could reduce the frequency of GDM in Chinese overweight/obese women.
Materials and Methods
Study design and participants
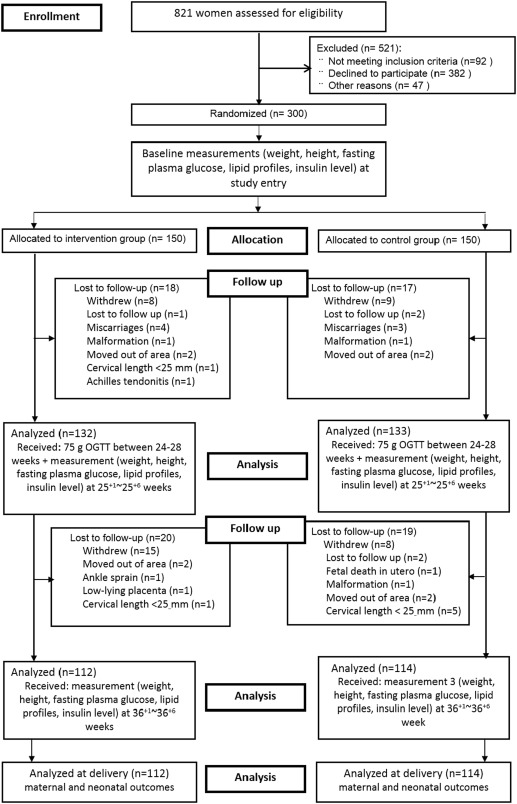
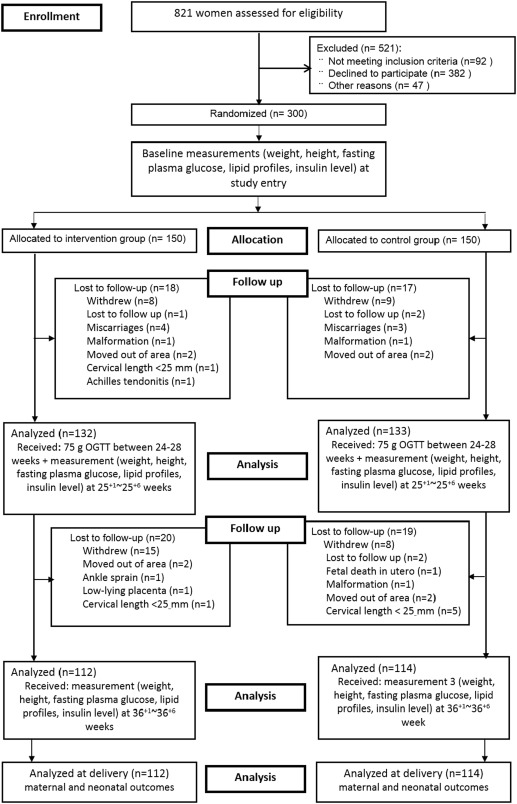
We conducted a RCT at Peking University First Hospital from December 2014 through July 2016. A flow chart of the protocol is shown in the Figure . Overweight and obesity were determined based on body mass index (BMI) recommendations of the Group of China Obesity Task Force of the Chinese Ministry of Health accounting for interracial differences: overweight BMI ≥24-<28 kg/m 2 and obese BMI ≥28 kg/m 2 . Singleton, nonsmoking pregnant women with a prepregnancy BMI (p-BMI) of ≥24 kg/m 2 at <12 +6 weeks’ gestation were eligible for the study. The exclusion criteria were the following: (1) age <18 years; (2) women unwilling to provide informed consent; (3) women with cervical insufficiency (historical painless cervical dilation leading to recurrent second-trimester births in the absence of other causes; dilated cervix on manual or speculum examination; transvaginal ultrasound cervical length <25 mm at <24 weeks of gestation in singleton gestations with ≥1 prior spontaneous preterm births at 14-36 weeks) ; (4) women on any medication for preexisting hypertension, diabetes, cardiac disease, renal disease, systemic lupus erythematosus, thyroid disease, or psychosis; and (5) women who were currently being treated with metformin or corticosteroids.
This study was reviewed and approved by the Institutional Review Board of Peking University First Hospital (reference number: 2014[726]) and registered at www.clinicaltrials.gov (NCT02304718). All participants provided written informed consent, and the ethics committee approved the consent procedure.
Randomization and masking
Eligible women were randomly allocated (ratio 1:1) into either an exercise intervention group or a control group following an allocation concealment process using an automatic computer-generated random number table. The 3 parts of the randomization process, that is, sequence generation, allocation concealment, and implementation, were conducted by 3 different individuals. Due to the nature of the intervention, all participants and research staff were aware of the allocations.
Research procedures
Eligible pregnant women were approached by research staff at a prenatal care class specifically for women in early pregnancy at the Department of Obstetrics and Gynecology, Peking University First Hospital, and provided the project details. Those who were willing to participate were asked to complete a questionnaire to assess demographic information, medical and family history, and current pregnancy information. Qualified participants were then asked to sign informed consent and randomly allocated into a group. Provided permission was granted, and demographic information was collected from women who declined participation.
Participants allocated to the control group continued with their usual daily activities and were not discouraged from participating in exercise sessions on their own. In contrast, the participants randomized to the exercise group engaged in a supervised cycling program involving at least 3 sessions per week. The intervention was initiated within 3 days of randomization and continued to the end of the third trimester (weeks 36-37). All women received standard prenatal care throughout the intervention period, and they had equal numbers of usual visits with their obstetricians during pregnancy. All women received general advice about the positive effects of physical activity during pregnancy, and no special dietary recommendation were given.
The exercise protocol was based on a previous study showing the benefits of regular stationary cycling exercise for blood glucose control in women with GDM. All the exercise sessions occurred at Peking University First Hospital under supervision. Sessions were conducted on alternate days with the supervisor maintaining detailed records regarding the participants’ physiological indexes and compliance. At the start of the intervention, each exercise session consisted of stationary cycling for 30 minutes, beginning with a 5-minute warm-up at low intensity, which was 55-65% of the age-predicted heart rate maximum (HRmax) and a rating of perceived exertion (RPE) according to Borg scale between 9-11. RPE is the perceived score of difficulty when exercising, and is frequently used to subjectively monitor the exercise intensity based on individual perception. The Borg scale is the most frequently used method to evaluate individual RPE. This scale ranges from 6-20, where exercise is perceived to be “no exertion at all” to “very very hard,” respectively. Subsequently, 5 minutes of continuous moderate-intensity cycling (65-75% of the age-predicted HRmax; RPE 12-14) ensued. Next, the participants completed a period of interval cycling consisting of 30 seconds of rapid pedaling (sprints, higher intensity efforts) at 75-85% of the age-predicted HRmax and RPE 15-16 every 2 minutes for 3-5 intervals. This sprinting was followed by 5 minutes of continuous cycling at low-to-moderate intensity (60-70% of the age-predicted HRmax; RPE 10-12) before beginning another period of interval cycling. During this interval phase, continuous moderate-intensity cycling at 65-75% of the age-predicted HRmax (RPE 12-14) was interspersed with 1-minute periods of pedaling against increased resistance (hill climb) at 75-85% of the age-predicted HRmax (RPE 13-15); these periods alternated every 2 minutes for 3 repeats. Each session ended with a 5-minute cool down of easy cycling. At the start of the intervention, the women exercised at the lower end of the calculated heart rate ranges, with progressive increases as the program continued. Additionally, the exercise duration was progressively increased to 45-60 minutes by adding 5 minutes to the intervals or the continuous moderate-intensity cycling phases according to individual ability. The inclusion of periods of interval cycling was based on a previous study showing benefits for energy expenditure and exercise enjoyment in pregnant women.
All pregnant women who receive standard prenatal care at Peking University First Hospital have 4 routine ultrasound examinations throughout pregnancy at 11-13 +6 , 20-23 +6 , 30-30 +6 , and 36-36 +6 gestational weeks. Cervical length was measured at each examination. Due to the possibility of an increased risk of preterm birth caused by cycling-induced shortening of cervical length, to ensure and evaluate the safety of exercise during pregnancy, we recorded and reviewed cervical length at each examination and excluded those women with a cervical length <25 mm at any time during the intervention because uterine cervix length is an accurate predictor of the risk of preterm birth. For consistency, we also excluded those participants in the control group with a cervical length <25 mm.
Furthermore, at study entry, we measured each participant’s height to the nearest 0.5 cm without shoes and weight accurate to 0.1 kg with light clothing. BMI was calculated as maternal weight divided by height (kg/m 2 ). Additionally, blood was drawn from the antecubital vein after the participant had fasted for at least 8 hours but not >14 hours and was collected in sterile vacutainer tubes preloaded with heparin. There was at least 24 hours between the last exercise bout and the time of blood draw. Blood was centrifuged at 1800 g at 4°C for 10 minutes within 4 hours of collection; subsequently, the plasma was separated and glucose was measured immediately. The remaining plasma was stored at –80°C for later analysis of insulin and lipid parameters (triglyceride, total cholesterol, and low- and high-density lipoprotein cholesterol). Insulin was measured using radioimmunoassay commercial kits (Beifang Institute of Biochemical Technology, Beijing, China). The insulin resistance index was calculated according to the homeostasis model of assessment: fasting plasma insulin (μU/mL) × fasting glucose (mmol/L)/22.5. Fasting lipid profiles were measured using an automatic analyzer (7600; Hitachi High-Technologies Corp, Tokyo, Japan) in the Department of Clinical Laboratory, Peking University First Hospital. Maternal body weight measurement and biochemical tests were repeated at 25 and 36 gestational weeks.
To assess the participants’ physical activity levels during pregnancy, the International Physical Activity Questionnaire was used at study entry and at 25 and 36 weeks’ gestation. The questionnaire included questions about the number of days per week and the time spent sitting, walking, and doing moderate and vigorous activities, and then a score, which is expressed as metabolic equivalents of task min/wk, can be calculated using the formula 8.0 × vigorous activity + 4.0 × moderate activity + 3.3 × light activity (walking) for the different activity categories.
At 24-28 weeks’ gestation, all participants underwent a 75-g oral glucose tolerance test (OGTT) after an overnight fast to diagnose GDM. Similarly, at least 24 hours elapsed between the last exercise session and the OGTT. According to the new criteria amended in August 2014 in China, GDM was diagnosed when any 1 value was ≥5.1 mmol/L at 0 hours, ≥10.0 mmol/L at 1 hour, or ≥8.5 mmol/L at 2 hours. Values of 7.0 mmol/L at 0 hours or 11.1 mmol/L at 2 hours were diagnosed as diabetes mellitus, regardless of pregnancy stage.
Outcomes
The primary outcome was the incidence of GDM (this has been reported as a letter in Diabetes Care , but this article includes a number of other important outcomes). The secondary outcomes included physical activity levels; gestational weight gain; biochemical outcomes, including insulin resistance and lipid profiles; maternal outcomes, such as gestational hypertension (defined as blood pressure elevation [systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg] >20 weeks’ gestation in the absence of proteinuria), preeclampsia (defined as new-onset hypertension [systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg] and new-onset proteinuria [300 mg of protein in 24 hours or a urine protein/creatinine ratio of 0.3 mg/dL] >20 weeks’ gestation or, in the absence of proteinuria, new-onset hypertension with new-onset thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema, or cerebral or visual disturbances), and mode of delivery (vaginal, operative vaginal, or cesarean); and neonatal outcomes, including gestational age at delivery, preterm birth (<37 and <34 weeks), Apgar score, birthweight, macrosomia (birthweight >4000 g), large-for-gestational-age (LGA) infants (birthweight >90th percentile for gestational age), and small-for-gestational-age (SGA) infants (birthweight <10th percentile for gestational age), both LGA and SGA were defined in accordance with international standards for sex-specific newborn size for each gestational age based on data from the Newborn Cross-Sectional Study subpopulation.
Statistical analysis
We calculated that a sample size of 121 participants in each group was sufficient to detect a 50% reduction in the incidence of GDM with an α of 0.05 and a statistical power (1-β) of 0.8 based on our previous study. Assuming a dropout rate of 10-15%, the target sample size was 150 in each group.
Data were analyzed using statistical software (SPSS, 17.0, IBM Corp, Armonk, NY). Continuous variables are presented as mean ± SD, and categorical variables are presented as numbers and percentages. Differences in the means between groups were evaluated using independent sample t tests and analysis of variance. Pearson χ 2 test was used for categorical variables. Analysis was by intention to treat. The level of statistical significance was set at .05.
Materials and Methods
Study design and participants
We conducted a RCT at Peking University First Hospital from December 2014 through July 2016. A flow chart of the protocol is shown in the Figure . Overweight and obesity were determined based on body mass index (BMI) recommendations of the Group of China Obesity Task Force of the Chinese Ministry of Health accounting for interracial differences: overweight BMI ≥24-<28 kg/m 2 and obese BMI ≥28 kg/m 2 . Singleton, nonsmoking pregnant women with a prepregnancy BMI (p-BMI) of ≥24 kg/m 2 at <12 +6 weeks’ gestation were eligible for the study. The exclusion criteria were the following: (1) age <18 years; (2) women unwilling to provide informed consent; (3) women with cervical insufficiency (historical painless cervical dilation leading to recurrent second-trimester births in the absence of other causes; dilated cervix on manual or speculum examination; transvaginal ultrasound cervical length <25 mm at <24 weeks of gestation in singleton gestations with ≥1 prior spontaneous preterm births at 14-36 weeks) ; (4) women on any medication for preexisting hypertension, diabetes, cardiac disease, renal disease, systemic lupus erythematosus, thyroid disease, or psychosis; and (5) women who were currently being treated with metformin or corticosteroids.
This study was reviewed and approved by the Institutional Review Board of Peking University First Hospital (reference number: 2014[726]) and registered at www.clinicaltrials.gov (NCT02304718). All participants provided written informed consent, and the ethics committee approved the consent procedure.
Randomization and masking
Eligible women were randomly allocated (ratio 1:1) into either an exercise intervention group or a control group following an allocation concealment process using an automatic computer-generated random number table. The 3 parts of the randomization process, that is, sequence generation, allocation concealment, and implementation, were conducted by 3 different individuals. Due to the nature of the intervention, all participants and research staff were aware of the allocations.
Research procedures
Eligible pregnant women were approached by research staff at a prenatal care class specifically for women in early pregnancy at the Department of Obstetrics and Gynecology, Peking University First Hospital, and provided the project details. Those who were willing to participate were asked to complete a questionnaire to assess demographic information, medical and family history, and current pregnancy information. Qualified participants were then asked to sign informed consent and randomly allocated into a group. Provided permission was granted, and demographic information was collected from women who declined participation.
Participants allocated to the control group continued with their usual daily activities and were not discouraged from participating in exercise sessions on their own. In contrast, the participants randomized to the exercise group engaged in a supervised cycling program involving at least 3 sessions per week. The intervention was initiated within 3 days of randomization and continued to the end of the third trimester (weeks 36-37). All women received standard prenatal care throughout the intervention period, and they had equal numbers of usual visits with their obstetricians during pregnancy. All women received general advice about the positive effects of physical activity during pregnancy, and no special dietary recommendation were given.
The exercise protocol was based on a previous study showing the benefits of regular stationary cycling exercise for blood glucose control in women with GDM. All the exercise sessions occurred at Peking University First Hospital under supervision. Sessions were conducted on alternate days with the supervisor maintaining detailed records regarding the participants’ physiological indexes and compliance. At the start of the intervention, each exercise session consisted of stationary cycling for 30 minutes, beginning with a 5-minute warm-up at low intensity, which was 55-65% of the age-predicted heart rate maximum (HRmax) and a rating of perceived exertion (RPE) according to Borg scale between 9-11. RPE is the perceived score of difficulty when exercising, and is frequently used to subjectively monitor the exercise intensity based on individual perception. The Borg scale is the most frequently used method to evaluate individual RPE. This scale ranges from 6-20, where exercise is perceived to be “no exertion at all” to “very very hard,” respectively. Subsequently, 5 minutes of continuous moderate-intensity cycling (65-75% of the age-predicted HRmax; RPE 12-14) ensued. Next, the participants completed a period of interval cycling consisting of 30 seconds of rapid pedaling (sprints, higher intensity efforts) at 75-85% of the age-predicted HRmax and RPE 15-16 every 2 minutes for 3-5 intervals. This sprinting was followed by 5 minutes of continuous cycling at low-to-moderate intensity (60-70% of the age-predicted HRmax; RPE 10-12) before beginning another period of interval cycling. During this interval phase, continuous moderate-intensity cycling at 65-75% of the age-predicted HRmax (RPE 12-14) was interspersed with 1-minute periods of pedaling against increased resistance (hill climb) at 75-85% of the age-predicted HRmax (RPE 13-15); these periods alternated every 2 minutes for 3 repeats. Each session ended with a 5-minute cool down of easy cycling. At the start of the intervention, the women exercised at the lower end of the calculated heart rate ranges, with progressive increases as the program continued. Additionally, the exercise duration was progressively increased to 45-60 minutes by adding 5 minutes to the intervals or the continuous moderate-intensity cycling phases according to individual ability. The inclusion of periods of interval cycling was based on a previous study showing benefits for energy expenditure and exercise enjoyment in pregnant women.
All pregnant women who receive standard prenatal care at Peking University First Hospital have 4 routine ultrasound examinations throughout pregnancy at 11-13 +6 , 20-23 +6 , 30-30 +6 , and 36-36 +6 gestational weeks. Cervical length was measured at each examination. Due to the possibility of an increased risk of preterm birth caused by cycling-induced shortening of cervical length, to ensure and evaluate the safety of exercise during pregnancy, we recorded and reviewed cervical length at each examination and excluded those women with a cervical length <25 mm at any time during the intervention because uterine cervix length is an accurate predictor of the risk of preterm birth. For consistency, we also excluded those participants in the control group with a cervical length <25 mm.
Furthermore, at study entry, we measured each participant’s height to the nearest 0.5 cm without shoes and weight accurate to 0.1 kg with light clothing. BMI was calculated as maternal weight divided by height (kg/m 2 ). Additionally, blood was drawn from the antecubital vein after the participant had fasted for at least 8 hours but not >14 hours and was collected in sterile vacutainer tubes preloaded with heparin. There was at least 24 hours between the last exercise bout and the time of blood draw. Blood was centrifuged at 1800 g at 4°C for 10 minutes within 4 hours of collection; subsequently, the plasma was separated and glucose was measured immediately. The remaining plasma was stored at –80°C for later analysis of insulin and lipid parameters (triglyceride, total cholesterol, and low- and high-density lipoprotein cholesterol). Insulin was measured using radioimmunoassay commercial kits (Beifang Institute of Biochemical Technology, Beijing, China). The insulin resistance index was calculated according to the homeostasis model of assessment: fasting plasma insulin (μU/mL) × fasting glucose (mmol/L)/22.5. Fasting lipid profiles were measured using an automatic analyzer (7600; Hitachi High-Technologies Corp, Tokyo, Japan) in the Department of Clinical Laboratory, Peking University First Hospital. Maternal body weight measurement and biochemical tests were repeated at 25 and 36 gestational weeks.
To assess the participants’ physical activity levels during pregnancy, the International Physical Activity Questionnaire was used at study entry and at 25 and 36 weeks’ gestation. The questionnaire included questions about the number of days per week and the time spent sitting, walking, and doing moderate and vigorous activities, and then a score, which is expressed as metabolic equivalents of task min/wk, can be calculated using the formula 8.0 × vigorous activity + 4.0 × moderate activity + 3.3 × light activity (walking) for the different activity categories.
At 24-28 weeks’ gestation, all participants underwent a 75-g oral glucose tolerance test (OGTT) after an overnight fast to diagnose GDM. Similarly, at least 24 hours elapsed between the last exercise session and the OGTT. According to the new criteria amended in August 2014 in China, GDM was diagnosed when any 1 value was ≥5.1 mmol/L at 0 hours, ≥10.0 mmol/L at 1 hour, or ≥8.5 mmol/L at 2 hours. Values of 7.0 mmol/L at 0 hours or 11.1 mmol/L at 2 hours were diagnosed as diabetes mellitus, regardless of pregnancy stage.
Outcomes
The primary outcome was the incidence of GDM (this has been reported as a letter in Diabetes Care , but this article includes a number of other important outcomes). The secondary outcomes included physical activity levels; gestational weight gain; biochemical outcomes, including insulin resistance and lipid profiles; maternal outcomes, such as gestational hypertension (defined as blood pressure elevation [systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg] >20 weeks’ gestation in the absence of proteinuria), preeclampsia (defined as new-onset hypertension [systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg] and new-onset proteinuria [300 mg of protein in 24 hours or a urine protein/creatinine ratio of 0.3 mg/dL] >20 weeks’ gestation or, in the absence of proteinuria, new-onset hypertension with new-onset thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema, or cerebral or visual disturbances), and mode of delivery (vaginal, operative vaginal, or cesarean); and neonatal outcomes, including gestational age at delivery, preterm birth (<37 and <34 weeks), Apgar score, birthweight, macrosomia (birthweight >4000 g), large-for-gestational-age (LGA) infants (birthweight >90th percentile for gestational age), and small-for-gestational-age (SGA) infants (birthweight <10th percentile for gestational age), both LGA and SGA were defined in accordance with international standards for sex-specific newborn size for each gestational age based on data from the Newborn Cross-Sectional Study subpopulation.
Statistical analysis
We calculated that a sample size of 121 participants in each group was sufficient to detect a 50% reduction in the incidence of GDM with an α of 0.05 and a statistical power (1-β) of 0.8 based on our previous study. Assuming a dropout rate of 10-15%, the target sample size was 150 in each group.
Data were analyzed using statistical software (SPSS, 17.0, IBM Corp, Armonk, NY). Continuous variables are presented as mean ± SD, and categorical variables are presented as numbers and percentages. Differences in the means between groups were evaluated using independent sample t tests and analysis of variance. Pearson χ 2 test was used for categorical variables. Analysis was by intention to treat. The level of statistical significance was set at .05.
Results
From December 2014 through July 2016, 821 pregnant women with a BMI ≥24 kg/m 2 were screened for eligibility. Among those individuals, 300 singleton women at 10 weeks’ gestational age and with a mean p-BMI of 26.78 ± 2.75 kg/m 2 were recruited. They were randomized to either the exercise group (n = 150) or the control group (n = 150). In all, 39 (26.0%) and 38 (25.3%) participants were obese in each group, respectively. The baseline characteristics of these individuals are summarized in Table 1 , and the 2 groups were well matched at baseline, with no significant differences in age, p-BMI, gestational age, family history of diabetes, personal history of GDM, or fasting plasma glucose at study entry. Compared with women who declined to participate but agreed to the use of their routine data, the participants had a fasting plasma glucose that was 0.08 mmol/L higher and were more likely to have a family history of diabetes mellitus ( P < .05).



