Definition of paediatric foot posture 107
Historical overview of the flat foot 107
Observation and the development of clinical measures 113
The reliability of traditional measures of foot posture 114
Foot posture index (FPI-6) 115
Supination resistance test 115
Longitudinal arch angle (Feiss line) 117
Ankle range 117
Current view of children’s foot posture 118
The flat foot proforma (FFP): a clinical pathway 118
Alternative clinical measures to monitor treatment efficacy 119
Prevalence 121
Differential diagnosis 122
Basic steps to managing children with flat feet 126
Definition of paediatric foot posture
The anatomical position of the weight-bearing child’s foot, as clinically observed in the cardinal body planes.
While the flat foot is the major concern and the more common finding, it should not be forgotten that the highly arched, supinated foot is also a concern and needs to be appreciated (see Ch. 5, Charcot–Marie–Tooth disease Key Concepts box).
Historical overview of the flat foot
The flat foot has long been regarded as a disabling problem, either immediately or potentially. The wide array of synonyms for flat feet include: pes planus (Tareco et al 1999), calcaneovalgus (Aharonson et al 1992), pes valgus (Bleck & Berzins 1977), flexible flatfoot (Wenger et al 1989), flexible pes planus Kuhn et al 1999), planovalgus (Staheli 1987), postural valgus hindfeet (Powell 1983), hypermobile flatfoot (Bordelon 1980), pronated foot (Root et al 1977).
Much has been written about flat feet, yet a precise definition remains elusive. Historically, it has been observed that people whose feet were painful were often ‘flat’ or observed to have a lowered medial longitudinal arch and everted (or ‘valgus’) heel position. Some of these people were physically limited by their flat feet and seen as ‘weaker’, being less able to walk or run distances or to work efficiently. From the perspective of strengthening ‘weak’ flat feet, various arch supports have been developed and the basic principles of these are still incorporated into orthotic therapy today.
Definition of what exactly constitutes a flat foot remains debatable, as does the premise that flat feet are problematic. There is no doubt that some flat feet are associated with pain and disability and that orthotic therapy can be beneficial (Landorf & Keenan 2000). There is, however, much doubt and dispute about children’s flat feet being regarded as a problem (Bordelon 1980, 1983; Ganley 1987; Price 1982; Staheli 1987, 1999), and there is even more disagreement about the use of orthoses in children, particularly if asymptomatic (McDonald & Kidd 1998). The notion of prevention has seen children with flat feet treated with orthoses in an effort to save them from future disability. Unfortunately this notion (Bordelon 1983, Capasso 1993, D’Amico 1984, Jay & Schoenhaus 1992, Jay et al 1995, Kirby 1992, Mereday et al 1972, Valmassy 1996) is yet to be substantiated and clinicians continue to differ over the management of children with flat feet.
The definition of flat feet has not been helped by the varying techniques used to assess them. The medial longitudinal arch height, heel angle and footprints have all been used in efforts to measure the ‘flatness’ of feet. Clinical measures of the feet have been another area of great dissent among both clinicians and researchers. The last 20 years have seen investigation of clinical foot measures by evaluating the basic measurement principles of reliability and validity (Elveru et al 1988, Freeman 1990, Sell et al 1994). In general the reliability of these measures is poor and the validity questionable (Astrom & Arvidson 1995). Very little research has addressed the use of these measures in children’s feet.
Classification of flat feet
Staheli’s review articles (1987, 1994) notice the almost moralistic overtones with which the flat foot has been discussed. In contrast with the aristocratic, high-arched foot type, the flat foot was mooted as inferior. The ‘low’ arch was the ‘fallen’ arch, insinuated as being undesirable (perhaps even ‘loose’) as well as potentially disabling to the encumbered.
Methods of classification have consisted of footprint assessment, X-rays and visual observation.
The arch
Great attention has been paid to the medial longitudinal arch of the foot as a way of assessing foot posture. The normal infant’s foot begins as a flat foot with the medial longitudinal arch developing during childhood (Gould et al 1989, Morley 1957, Rao & Joseph 1992, Staheli 1987). It is accepted that the flatness of normal children’s feet and their age are inversely proportioned (Cappello & Song 1998). The arch has been assessed using:
• footprints (Staheli 1987)
• radiographic imaging
• pedotopography (observation of the weight-bearing foot using photography; Gould et al 1989)
• clinical measurements (Gould et al 1989, Saltzman et al 1995).
Staheli (1987) devised an arch index from footprints in 441 subjects aged from 1 to 80 years. Staheli’s arch index was calculated by measuring the width of the footprint arch and the width of the footprint heel and dividing the arch measure by the heel measure. Arch index results ranged broadly as 0.70–1.35 in infancy and 0.30–1.0 after childhood, indicating a decline in footprint arch width with increasing age that was surmised by the authors to be indicative of increasing arch height during childhood.
Gould’s study looked specifically at the development of the child’s medial longitudinal arch in subjects aged 11 months to 5 years (Gould et al 1989). The children were studied for 4 years with X-ray, clinical and pedotopographical examinations each year. This study found that medial longitudinal arch development was rapid in the first 5 years of life and was faster until 3 years of age if arch support footwear was used. It must be noted that X-ray angles were used to categorize the feet as having ‘normal, slightly flat, moderate’ arches, which must have been difficult when using radiographs of such young incompletely ossified feet.
Saltzman et al (1995) performed clinical and radiographic assessments in adults in an effort to validate clinical measures of the medial longitudinal arch. The best anthropometric parameter to characterize medial longitudinal arch structure was found to be a ratio of navicular height to foot length.
The heel eversion angle
Heel eversion or hindfoot valgus (Powell 1983) is generally accepted as a normal finding in young, newly walking children and is expected to reduce with age. The eversion of the heel has been repeatedly used for determining the posture of the child’s foot (Wenger et al 1989). Originating in the orthopaedic literature (Morton 1937), it has been the view of podiatrists that a vertical heel (assessed by the bisection) is optimal for foot function (Fig. 6.1A, B; Root et al 1971, 1977). The basis for this principle comes from the attempts of Root (Root et al 1971, 1977) and co-authors to define all foot motion around the three cardinal body planes.
Recent research has challenged the Root model and suggested alternative methods (Dahle et al 1991; Elveru et al 1988; Keenan 1997; Menz 1995, 1998). The clinical measure of resting calcaneal stance position has guided clinicians in assessment of the child’s foot posture and calcaneal eversion has been suggested (but not shown) to reduce by a degree every 12 months to a vertical position by age 7 years (Valmassy 1996). More recently a study investigating the rear foot angle in 150 children aged from 6 to 16 years (Sobel et al 1999) found that the average rear foot angle for all children was 4° valgus (ranging from 0 to 9° valgus).
Foot flexibility
The literature includes many arguments about what constitutes a flat foot versus a floppy flat foot (Luhmann et al 2000, Powell 1983), with Jack’s great toe extension test seen as the delineating factor by many (Barry & Scranton 1983; Lin et al 1999; Rose et al 1985; Staheli 1987, 1999; Wenger et al 1989). Staheli (1987) has been emphatic about the distinction between pathological (rigid) and physiological (flexible) flat feet. The significance of the flexible flat foot continues to be the topic of much contention (Cohen & Cowell 1989, Garcia-Rodriguez et al 1999, Kanatli et al 2001, Lin et al 1999, Tareco et al 1999, Wenger et al 1989). The flat foot proforma (FFP) has been developed in an effort to make sense of this issue for the clinician (Evans 2007).
Clinical Tip
Jack’s test
Clinical Tip
Jack’s test
The hallux is manually dorsiflexed while the child is standing. If the medial longitudinal arch is seen to rise, the foot is deemed a flexible flat foot. If the arch remains static, this test designates a rigid flat foot.
The rise of the medial longitudinal arch, via tightening of the plantar fascia, without muscle activity, is referred to as the windlass mechanism, a fundamental aspect of sagittal plane foot functioning (Aquino & Payne 2001, Cornwall & McPoil 1999a).
When applying Jack’s test in adults, an immediate rising of the arch indicates greater tensile forces with the plantar fascia. In contrast, a delayed rise of the arch is associated with a more inverted heel strike, greater rear foot eversion and less re-supination (Kappel-Bargas et al 1998; Fig. 6.2).
 |
| Figure 6.2 |
Footprints
Footprints have been used intuitively to assess the foot’s posture, the effects of orthotic intervention (Capasso 1993, Cappello & Song 1998, Sachithanandam & Joseph 1995), and especially to study flat feet in various populations (Capasso 1993, Cappello & Song 1998, Didia et al 1987, Harris & Beath 1948, Kanatli et al 2001, Lin et al 1999, Morley 1957, Rao & Jospeh 1992, Rose et al 1985, Sachithanandam & Joseph 1995, Staheli 1987, Tareco et al 1999). Rose et al (1985) developed the valgus index as an early measure of flat feet. The footprint continues to be included as a proxy indicator of arch height and has formed the basis of plantar pressure measurement using:
• foot-ground pressure patterns (Aharonson et al 1992)
• dynamic plantar pressure systems, e.g. Emed™, Musgrave™, Vifor™ (Widhe 1997).
Whether or not footprints reflect the real morphology of the medial longitudinal arch is still controversial (Carranza-Bencano et al 1997, Volpon 1994). However, the recent development of a normative databank for foot loading patterns and foot shape parameters in new walking children does find initial correlation between dynamic pressure patterns and static footprints. This valuable and ongoing investigation has also found an increase in peak pressures of the paediatric forefoot approximating 11% per year with a simultaneous decrease of 9% per year in the midfoot area (Bosch et al 2007). Earlier, and less comprehensive, plantar pressure research found an almost three times higher load in the infant midfoot as compared to adult feet (Henning & Rosenbaum 1991). Using the Chippaux-Smirak Index in a study of 1676 children’s feet, the highest percentage of lowered medial longitudinal arch was found in younger children and reduced with age, supporting the long observed physiologically increasing arch height proportional to age (Forriol & Pascual 1990, Nikalaidou & Boudolos 2006).
X-rays
Many studies have attempted to assess children’s foot posture types using X-rays (Bleck & Berzins 1977, Bordelon 1980, Capasso 1993, Kanatli et al 2001, Price 1982). Staheli (1987) suggests that X-rays are only appropriate to determine the aetiology of rigid (pathological) flat feet and that these views should be taken in stance. Rose stated categorically that X-rays should be interpreted with caution when used to assess children’s foot posture due to bony development and superimposition of structures (Rose et al 1985). X-rays were used to assess foot morphology in Wenger’s clinical trial for foot orthoses (Wenger et al 1989) and shoes in pre-school children and also in Bordelon’s uncontrolled observations (1980), hence limiting the conclusions of these studies.
Observation and the development of clinical measures
Visual appearance of the flat foot has been the basis of all other observations and has resulted in the development of quantitative measures. As previously mentioned, the arch, heel, ability of the foot to flex and form an arch and footprints have all been aspects observed and judged as constituents of the flat foot structure. X-rays have enabled an extension of visual observation, if limited to static, osseous, two-plane images. Rose was the first investigator to promote the concept of subtalar joint stability and also attempted one of the first measures of foot stability, the valgus index (Rose et al 1985). While based on the footprint, the valgus index was the first measure to focus on the rear of the heel and preceded the clinical measures developed by Root (Root et al 1977).
Podiatrists adopted the Root foot biomechanics model until the late 1980s when critical inquiry into these clinically accepted measures began (Elveru et al 1988, Mueller et al 1993, Picciano et al 1993). Developed in the 1970s, the work of Root, Orien and Weed (Root et al 1971, 1977) became the fundamental principles for podiatry students for 20 years. STJ (subtalar joint) neutral position is the essence of the Root theories, as normal feet should theoretically function from this point. It is also the reference mark from which measurements are made but lacks definition (Elveru et al 1988) as a starting point for measuring the foot (Weiner-Ogilvie et al 1997). The more recent questioning of the principles of Root biomechanics has resulted in debate and investigations into the reliability of these measures (Freeman 1990, Menz 1995, Sell et al 1994, Weiner-Ogilvie & Rome 1998, Weiner-Ogilvie et al 1997).
The reliability of traditional measures of foot posture
There are many measures of foot posture which can be used by clinicians. Overall, reliability of the traditional Root measures of foot posture has been found lacking. Some measures (e.g. navicular height) display acceptable reliability (Mathieson et al 2004, Sell et al 1994, Weiner-Ogilvie & Rome 1998) while others (e.g. resting calcaneal stance position and neutral calcaneal stance position) are less reliable. Neutral calcaneal stance position involves the locating of subtalar joint neutral position (Elveru et al 1988, Keenan 1997, Menz 1995, Pierrynowski et al 1996). The unsatisfactory reliability of neutral calcaneal stance position requires podiatrists to question the use of this measure for orthotic prescription. The validity of these measures has been very sparsely investigated (Backer & Kofoed 1989, Herbsthofer et al 1998, Schon et al 1998, Weseley et al 1969).
A number of observational assessment scales have been developed to try and address the issue of the poor reliability of foot measures. Most recently has been the development of the foot posture index (FPI; Redmond 2000; Redmond et al 2001a, 2001b), which is now used as the FPI-6 (Keenan et al 2006, Redmond et al 2006).
Foot posture index (FPI-6)
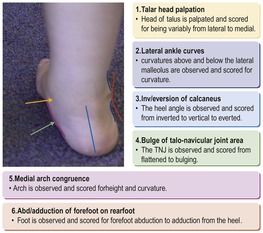
As described by Redmond (2000), the FPI-6 consists of six specific criteria:
2. curves above and below lateral malleolus
3. inversion/eversion of the calcaneus
4. bulge in the region of the TNJ
5. congruence of medial longitudinal arch
6. abduction/adduction of the forefoot on rear foot.
Figure 6.4 and Table 6.1 illustrate the six individual FPI criteria as observed and scored. The index identifies foot types, i.e. supinated, neutral or pronated, by its scoring system (Redmond 2000, Redmond et al 2001a). The inter-rater reliability of the FPI (both the initial FPI-8 and the modified FPI-6) has been found to vary (Evans et al 2003a, Cornwall et al 2008), but is better than many other measures. The validity of the FPI has also been investigated (Keenan et al 2006, Schartfbillig et al 2004). The FPI-6 is a useful clinical tool.
Supination resistance test
A simple test used to estimate the magnitude of pronatory moments is the supination resistance test (Kirby 1992; Fig. 6.3). The foot is manually supinated and the force required is assessed as being low, moderate or high. The higher the force required, the greater the supination resistance and the stronger the pronatory forces. The force needed to supinate the foot is scaled from 0 to 5. The reliability of the supination resistance test has been found to be good (ICC = 0.89) (Noakes & Payne 2003). The supination resistance test correlates moderately with mechanical loading (r = 0.57) and the FPI-8 (r = 0.60). The mean supination resistance has been assessed as 113.5 N ± 30.5 N in adult subjects (Payne et al 2003).
 |
| Figure 6.3 |
Similarly to STJ palpation, the supination resistance test is a useful guide for orthotic selection/prescription. In basic terms, the greater the supination resistance test, the greater the emphasis on anti-pronatory orthotic features, namely medial skive, inverted pour, medial rear foot post flare, etc.
Longitudinal arch angle (Feiss line)
The Feiss line connects the medial malleolus, the navicular and the first metatarsal head on the medial aspect of the weight-bearing foot (Fig. 6.4). In Jack’s test, extension of the first metatarsophalangeal joint checks:
• foot flexibility (a rigid foot will not move)
• the onset of the windlass mechanism by tensioning the plantar fascia.
The Feiss line (malleolus – navicular – first metatarsal head) increases when Jack’s test activates supination and raises the arch height. Investigation of the longitudinal arch angle found a mean value approximating 140° ± 6°, with only small associated error (SEM = 1.3°).
The reliability of the Feiss line is very good (ICC = 0.97), and there is good correlation between this angle when static and in gait (r = 0.97).
The angle of the Feiss line for adults is:
| •130–150° | normal foot |
| •<130° | pronated foot |
| •>150° | supinated foot (McPoil & Cornwall 2005). |
Ankle range
The standing lunge test has long been known to correlate with functional ankle range and to be predicative of sporting injury. An average of 35° ankle dorsiflexion is required for normal adult gait (Bennell et al 1998). Children’s ankle range assessment is generally an unreliable measure, as typically assessed when the child is non-weight-bearing (Evans & Scutter 2006). Clinically, I suggest looking at a child’s ability to squat, heel walk and increase stride length (without early heel lift).
Current view of children’s foot posture
From the research that has explored this area, it seems likely that the examination of young children’s feet may require a different approach from adult feet (Evans 2007, Evans et al 2003a, 2003b, 2004).
Clinical Tip
Clinical Tip
The use of varying forms of in-shoe devices and orthoses in symptomatic children is generally supported (Evans 2003, McDonald & Kidd 1998, Mereday et al 1972, Rodgers 1999, Wenger et al 1989). In most cases a prefabricated and relatively inexpensive orthotic device will suffice. Footwear needs to be optimized for the child’s circumstances primarily (Ch. 14).
The use of orthoses in adults is well supported, with positive effects on pain and foot deformity (Landorf et al 2000). There is much less evidence to support the use of any form of orthosis in children without pain (McDonald & Kidd 1998) and the notion of ‘correcting’ a child’s foot posture by utilizing orthoses is, at best, tenuous given the quality of the research to date (Bordelon 1980, 1983; Wenger et al 1989).
Opinion is still divided about whether there is a need to intervene when the child’s foot posture is ‘flat’ (Staheli 1999). Orthopaedists generally accept the use of orthoses in symptomatic children and podiatrists have developed a better appreciation of developmental trends of the paediatric foot and also the doubt surrounding mechanical intervention in asymptomatic children (Evans 2003, McDonald & Kidd 1998). The Cochrane Library systematic review provides the best available scientific evidence for intervention (Rome et al 2006; Table 6.2).
| Wenger et al 1989 | Powell et al 2005 | Whitford & Esterman 2007 | |
|---|---|---|---|
| Number of subjects | 98 | 40 | 180 |
| Age | 1–6 | 5–19 | 7–11 |
| Condition | Flexible flat feet | Juvenile arthritis, Foot pain for 1–24 months | ‘Flexible excessive pronation’ |
| Trial groups | Shoe Helfet heel cups UCBL orthoses Control | Athletic shoes Neoprene insoles Custom orthoses | Generic orthoses Custom orthoses Control |
| Outcome measures | X-rays | Pediatric pain questionnaire Timed walking Foot function index Ped QoL (physical) | Motor skills Physical activity Self-perception |
| Findings | No significant difference between groups | Orthoses group showed significant improvement in: pain, function, QoL | No significant difference between groups |
The flat foot proforma (FFP): a clinical pathway
Recognizing the clinical dilemma and building on clinical guidelines (Harris et al 2004), the flat foot proforma (FFP) is a recent attempt at classifying children’s flat feet to help direct clinical practice (Evans 2007, 2008a) (Appendix 6.1). The FFP has been developed by the author by incorporating clinical guidelines (Harris et al 2004) with results from investigations into the reliability and validity of children’s foot measures (Evans & Scutter, 2006; Evans et al 2003a, 2003b, 2003c, 2004) and the Cochrane Library review (Rome et al 2006). Recent reliability testing of the FFP has resulted in a revised version (the paediatric-FFP/p-FFP). The p-FFP has fewer items, demonstrated levels of inter-rater reliability and is quicker to use (Evans 2008b) (Appendix 6.2).
Alternative clinical measures to monitor treatment efficacy
If foot orthoses are to be used, clinicians need to demonstrate their efficacy for ongoing use to be justified. Two user-friendly methods of monitoring treatment effect for an individual clinical case are the single case experimental design and the patient generated index.
1. Single case experimental design (SCED)
The SCED is a useful clinical research tool that can identify cause–effect relationships without large sample sizes. By definition this ‘n = 1’ design can be easily used for clinical recording about treatment efficacy for an individual case. SCED has limitations in terms of the level of evidence (Portney & Watkins 2000); it uses the principles of ‘control’ to establish a causal relationship. SCEDs allow conclusions to be drawn about the effects of an intervention based on the responses of a single subject under controlled conditions (Evans 2003; Table 6.3).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree