Fig. 6.1
Transrectal US with TVS probe imaging of a uterine agenesis with vaginal agenesis of the upper vaginal part: 1+ —-+ normal hypoechoic lower vaginal tract with hyperechoic upper fibrotic agenetic tract. 2+—-+ uretra
Complete agenesis and hypoplasia without functioning endometrium could be observed in puberty with primary amenorrhea. Secondary sexual characteristics are present, which reflects the normal ovarian function with normal ovaries that can be seen during transrectal, transvaginal or transabdominal US. Primary amenorrhea with severe cyclic pelvic pain may reflect isolated vaginal agenesis and the presence of a uterus with functional endometrium secondary obstructed, resulting in hematometra. Hematometra appearance by ultrasound looks like a cystic structure containing dense fluid with ground-glass appearance (blood).
SHG has no role in the evaluation of müllerian agenesis and hypoplasia.
Hemi-uterus (ESHRE/ESGE Class U4) or Former AFS Unicornuate Uterus (AFS Class II)
On 2D TVS and TAS images, an isolated unicornuate uterus appears as a normal or slightly smaller than normal uterus and the characteristically asymmetric ellipsoidal shape is very difficult to be seen [22]. It can be suspected by an extremely laterodeviation of the uterus, an endometrial stripe in transverse section with circle shape and the visualization of only one intramural tubal part (Figs. 6.2 and 6.3a, b). A rudimentary horn in the presence of a small uterus could confirm the diagnosis. If a coronal section can be obtained transabdominally by a half-full bladder technique [23], the unicornuate uterus showed banana shaped endometrial cavity without the usual rounded fundal contour and without the triangular appearance of the fundal cavity (Figs. 6.2 and 6.3a, b).
Fig. 6.2
Comparison in a schematic view of a normal and a unicornuate uterus by 2D US. The normal transverse section of the uterus shows a typical ovoidal endometrial stripe, whereas in the unicornuate uterus the endometrial stripe appears with circle shape and only one intramural tubal part is seen. If a coronal section can be obtained transabdominally by a half-full bladder technique (Fedele) or by 3D US the unicornuate uterus showed banana shaped endometrial cavity without the usual rounded or straight fundal contour and without the typical appearance of the fundal cavity in transverse section
Fig. 6.3
Three planar (A) transverse section, (B) longitudinal section, (C) coronal section view of a normal (a) and unicornuate uterus (b). Note the round shaped endometrial stripe in the transverse section (A) of the unicornuate uterus (b) compared to the normal uterus (a). The coronal views (C) show also different morphologies (banana shapeded) in the unicornuate uterus (b) and fundal triangular in the normal uterus (a), where as the longitudinal sections (B) are quite similar
Unicornuate uterus could be associated with variable degrees of a rudimentary uterine horn. TVS can see a non-cavitary rudimentary horn without associate endometrium as a round shape myometrial structure near the single uterine corn and may be difficult to differentiate from a uterine peduncolate myoma. In case of rudimentary horn with endometrium a differential diagnosis in communicating or noncommunicating horn must be performed. The communication between the two horns can be evaluated by SHG.
On SHG images, speculum inspection of the cervix demonstrates a small cervix and a poorly developed contralateral vaginal fornix. After instillation of contrast material, the endometrial cavity assumes a fusiform shape, tapering at the apex and draining into a solitary fallopian tube. Filling of a small communicating rudimentary horn may be seen, although SHG cannot clearly delineate noncavitary and noncommunicating rudimentary horns [24].
The diagnosis of unicornuate uterus is usually incidental unless a non communicating rudimentary horn is present. Dysmenorrhea with hematometra may manifest at menarche in this subgroup. Unicornuate uterus is often diagnosed in infertile patients during the diagnostic workup by SHG or hysteroscopy. In addition, the incidence of endometriosis is increased in this subgroup, similar to the case of other uterine anomalies [25].
Renal abnormalities are more commonly associated with unicornuate uterus than with other müllerian duct anomalies and have been reported in 40 % of the patients [26]. The anomaly is always ipsilateral to the rudimentary horn. Renal agenesis is the most commonly reported abnormality, occurring in 67 % of cases. Ectopic kidney, horseshoe kidney, cystic renal dysplasia and duplicated collecting systems have also been described [26]. Therefore the evaluation by TAS is mandatory in these cases.
Complete Bicorporeal Uterus with Double Cervix (ESHRE/ESGE Class U3bC2) or Former AFS Didelphys Uterus (AFS Class III)
Uterus didelphys, which constitutes approximately 5 % of müllerian duct anomalies, is the result of nearly complete failure of fusion of the müllerian ducts. No communication is present between the two endometrial cavities and the two horns. A longitudinal vaginal septum is associated in 75 % of these anomalies [27]. In this type of anomaly, two separate normal-sized uteri and cervices are observed. A vaginal septum may be difficult to visualize by 2D US.
On TA US images, two separate divergent uterine horns are identified, with a large fundal cleft (Figs. 6.4a, b and 6.5).
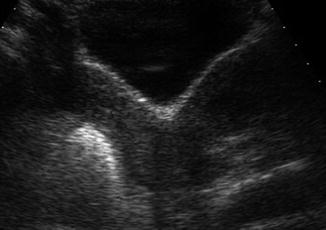
Fig. 6.4
TAS images of a dydelphus uterus in transverse section: (a) two separate uterine horns are seen (b) Color Doppler shows a typical uterine vascularization in each horn, arcuate and radial vessels in the myometrium around the endometrial layer
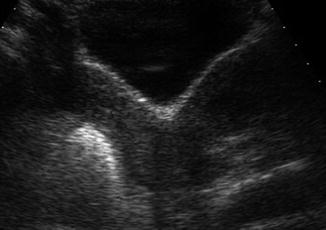
Fig. 6.5
Half full bladder TAS images of a dydelphus uterus, the coronal or frontal view shows two separate divergent uterine horns with a large fundal cleft
On TVS US two separate horns can be easily identify on the transverse section (Fig. 6.6). On the longitudinal section two endometrial cavities are seen uniformly separate, with no evidence of communication. The two uterine horns are usually widely displayed and endometrial and myometrial zonal widths are preserved. Two separate cervices need to be documented by identifying in transverse section two separate cervical canals and on the longitudinal section two external cervical os (Fig. 6.7). Color Doppler shows a typical uterine vascularization in each horn, arcuate and radial vessels in the myometrium around the endometrial layer (Fig. 6.4a, b).
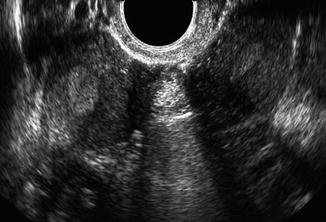
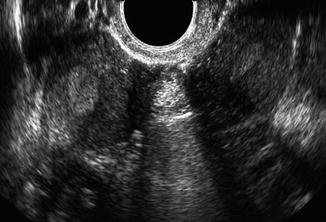
Fig. 6.6
TVS images of a dydelphus uterus, two separate uterine horns are seen transverse section completely separated from each other
Fig. 6.7
Schematic view of a dydelphus uterus, two completely separate uterine horns are seen in the transverse and frontal planes of the uterus, only the two cervix can appear separated or fused medially together
SHG demonstrates two separate endocervical canal, that open into separate fusiform endometrial cavities, with no communication between the two horns, the two cervical must be incannulated by two different catheters. However, if the anomaly is associated with an obstructed longitudinal vaginal septum, only one cervical os may be depicted, and it may be cannulated with the endometrial configuration mimicking a unicornuate uterus [28].
Non obstuctive uterus didelphys is usually asymptomatic, while uterus didelphys with unilateral vaginal obstruction may become symptomatic at menarche and manifest as dysmenorrhea. In case of obstructive vaginal septum, hematocolpo and hematometra can be observed on TVS and TAS (Fig. 6.8). Endometriosis and pelvic adhesions have an increased prevalence and are reported to be secondary to retrograde menstrual flow in the subset of patients with obstruction [25].
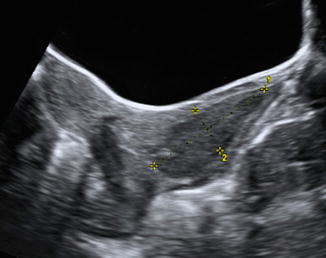
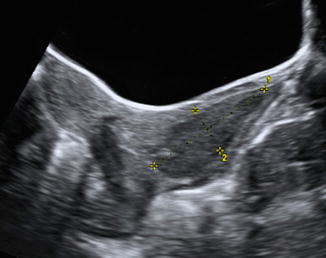
Fig. 6.8
TAS images of a hematocolpo in a young patient with didelphus uterus and an imperforated vaginal septum (Note the hypoechoic, dense fluid (blood) amount below the uterine cervix in the upper part of the vagina (1 longitudinal diameter, 2 anteroposterior diameter of the hematocolpo)
Bicorporeal Uterus (ESHRE/ESGE Class U3) or Former AFS Bicornuate Uterus (AFS Class IV)
The bicornuate uterus results from incomplete fusion of the uterovaginal horns at the level of the fundus and accounts for approximately 10 % of müllerian duct [13]. A bicornuate uterus consists of two symmetric cornua that are fused caudal with partial communication of the endometrial cavities, most often at the level of the uterine isthmus. The intervening cleft of the complete bicornuate uterus extends to the internal cervical os (bicornuate unicollis) while the cleft of a partial bicornuate configuration is of variable length. A bicornuate bicollis uterus is characterized by a cleft that extends to the external cervical os.
By 2D US, complete bicornuate uterus is very similar to the feature of the didelphus and only the assessment of one uterine isthmic cavity or cervical canal can made the diagnosis. In case of partial bicornuate uterus the length of the cleft between the two horns is important to be evaluated and several variations can be observed with different degree of communication between the two horns. The diagnosis of bicornuate bicollis uterus is very difficult by 2D ultrasound and probably the vaginal examination and hysteroscopy can be useful in evaluating two separate cervix.
In class IV or U3 anomalies, 2D US may demonstrate 2 uterine cavities with normal endometrium (Fig. 6.9a). The most important imaging finding is a concave fundus with a fundal cleft greater than 1 cm [5, 15, 29]. This has been shown to be a reliable means of distinguishing partial bicornuate uteri from septate uteri. 3D US plays actually the most important role in making this diagnosis. The cleft is visualized best on coronal or frontal image of the uterus that can be obtained by 2D TAS and half-full bladder technique (Fig. 6.5) or by 3D US. In case of partial bicornuate uterus on TVS transverse section near the fundus of the uterus, a double endometrial/myometrial view is seen whereas in the middle part of the uterus a double endometrial stripe is detected in one large uterine corpus (Figs. 6.9 and 6.10). On the longitudinal planes, the length of the corpus measured to each horn is greater than the length of the corpus taken through the midline (Fig. 6.10). This indentation between the two horns is much more easier to be detected by 3D US on the uterine coronal section. The cut-off level of this length of the indentation between the two horns to distinguish a partial bicornuate uterus from the septate uterus is 10 mm [15].
Fig. 6.9
TVS images of a bicornuate uterus (a) in comparison to a septate uterus (b): two separate uterine horns are seen the transverse section of the bicornuate uterus (a) whereas only double endometrial layer without doubling of the myometrium tissue around is seen in the septate uterus (b)
Fig. 6.10
Comparison in a schematic view of a partial bicornuate and a partial septate uterus by 2D US. In case of partial bicornuate uterus on TVS transverse section near the fundus of the uterus, a double endometrial/myometrial view is seen, whereas in the middle part of the uterus a double endometrial stripe is detected in one large uterine corpus. On the longitudinal planes, the length of the corpus measured to each horn is greater than the length of the corpus taken through the midline in case of bicornuate uterus, it is equal in case of septate uterus
It is also important in case of partial bicornuate uterus to evaluate the length of the communicating cavity and the presence of a partial septate cavity due to the fusion of uterine horns. In fact, in some partial bicornuate uterus, a hysteroscopy metroplasty can be performed in case of cavity with partial septum. It is therefore very important to measure the distance between the fundal indentation and the endometrial cavity. This can be done by 2D ultrasound in a longitudinal section calculating the difference of the distance of the residual myometrial tissue laterally on the horns and centrally at the level of the indentation and the common septum (Figs. 6.10 and 6.11). The septum separating the 2 horns demonstrates echogenicity identical to that of myometrium. The inferior portion of the septum (extending for a variable length inferiorly) may be fibrous [6].
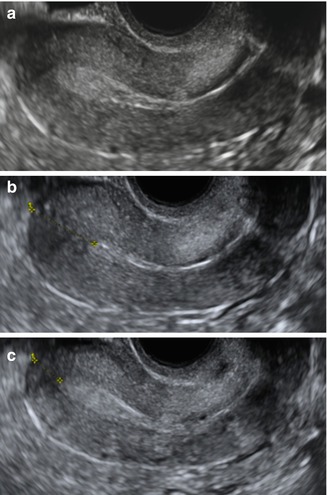
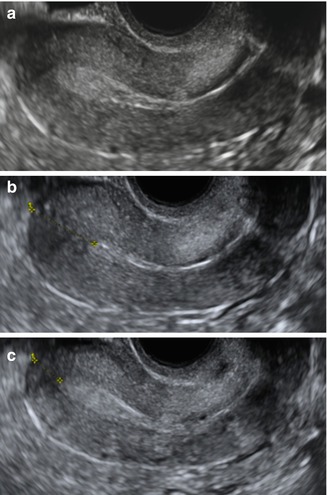
Fig. 6.11
TVS longitudinal view of a septate uterus in three different sections: (a) lateral on the left al the level of the tubal angle, (b) in the uterine middle at the level of the septum, (c) lateral on the right. Note the length of the corpus measured to each horn (diameter 1 in c) is equal to the length of the corpus taken through the midline (diameter 1 in b). Septum length can be obtained calculating the difference of the distance of the residual myometrial tissue laterally on the horns (a or c) and centrally at the level of the indentation and the common septum (b)
SHG can be useful in evaluating the communication between the cavities. The presence of uterine septum may create some difficulties to perform SHG accurately. In this case, as in the didelphus uterus, the two cervical must be incannulated by two different catheters. SHG gives also the opportunity to evaluate intracavitary anomaly such as polyps and fibroids.
Longitudinal upper vaginal septa are reported to coexist in 25 % of bicornuate uteri. In presence of imperforated septa or vaginal septa a hematocolpo can be observed (Fig. 6.8) [5, 15]. Features such as extreme anteflexion or retroflexion and the presence and deformity caused by overlying leiomyomas made the differential diagnosis extremely difficult.
Septate Uterus (ESHRE/ESGE Class U2 or Former AFS Class V)
The septate uterus composes approximately 55 % of müllerian duct anomalies [30] and results from partial or complete failure of resorption of the utero-vaginal septum after fusion of the paramesonephric ducts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


