22.2 CHEST DRAIN PLACEMENT
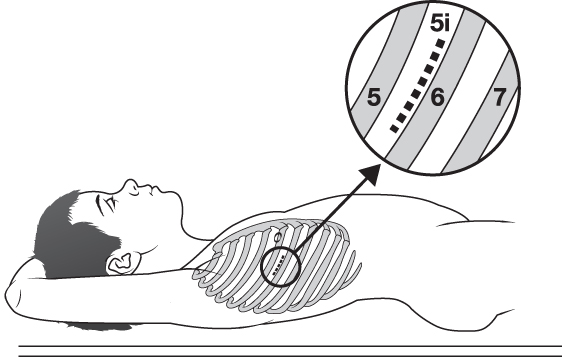
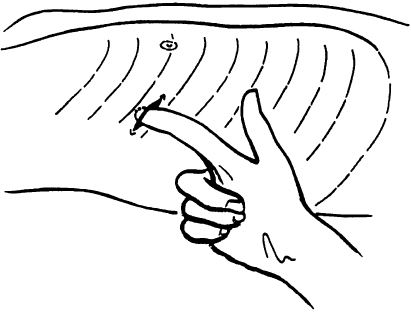
Chest drain placement should be performed using the open technique described here. This minimises lung damage. In general, the largest size drain that will pass between the ribs should be used.
Minimum Equipment
- Skin preparation and surgical drapes.
- Scalpel.
- Large clamps ×2.
- Suture.
- (Local anaesthetic.)
- Scissors.
- Chest drain tube.
- Underwater seal drain or Heimlich valve
Procedure
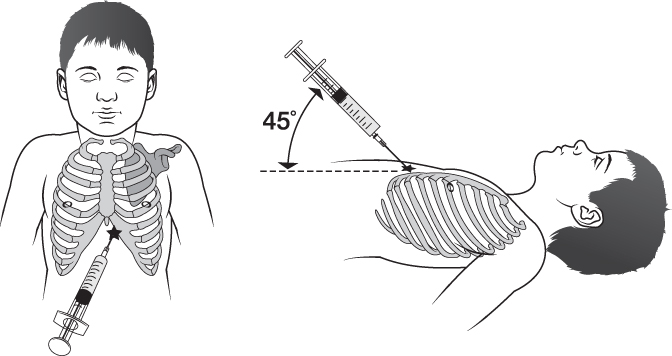
22.3 PERICARDIOCENTESIS
The removal of a small amount of fluid from the pericardial sac can be life saving. The procedure is not without risks and the electrocardiogram (ECG) should be closely monitored throughout. An acute injury pattern (ST segment changes or a widened QRS) indicates ventricular damage by the needle.
Minimum Equipment
- Skin preparation and surgical drapes.
- ECG monitor.
- (Local anaesthetic.)
- A 20 mL syringe.
- Large over-the-needle cannula (16 or 18 gauge).
Procedure
22.4 FEMORAL NERVE BLOCK
Femoral nerve blocks are commonly used for acute femoral fractures. Blockade of the femoral nerve results in anaesthesia of the anterior thigh, most of the femur and knee joint, and the skin on the lower leg’s medial aspect.
Recommended Blocks
- Blind fascia iliaca block.
- Ultrasound-guided femoral nerve block.
The blocks above have replaced the blind femoral nerve block as they confer increased efficacy and safety. Available evidence in children demonstrates that ultrasound guidance improves the quality, onset, duration and success rate of peripheral nerve blocks and lowers the local anaesthetic volume needed. Refer to the sectional below on avoiding nerve injury.
Anatomy
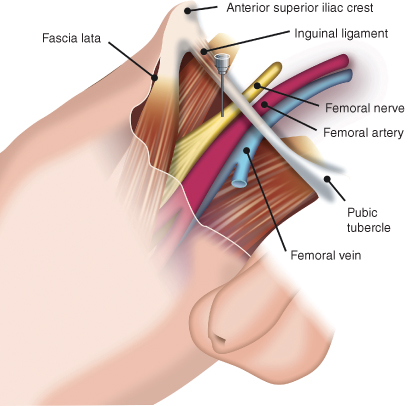
The femoral nerve passes underneath the inguinal ligament, lateral to the femoral artery. The mnemonic VAN (vein, artery, nerve) going from medial to lateral, aids recall of the relationship of the femoral nerve to the vessels. The blocks are performed just below the ligament. At this location the nerve is covered by the fascia lata (a continuation of the inguinal ligament) and fascia iliaca, which separates it from the femoral artery (Figure 22.6).
These fascia layers explain why ‘blind’ injection of local anaesthetic near the artery, or injection under the fascia lata only, can fail – the fascia iliaca prevents the spread of the local anaestheic to the femoral nerve.
Surface Anatomy
The inguinal ligament runs from the anterior superior iliac crest to the pubic tubercle. The arterial pulse is felt halfway along this line, with the femoral nerve lying just laterally. Femoral nerve block is performed at the femoral crease, about one to two patient finger breadths below the inguinal ligament.
Local Anaesthetic
A long acting anaesthetic should be used. The dose of bupivacaine is up to 0.8 mL/kg of 0.25% (up to 2 mg/kg); maximum 60 mL of 0.25%. Use a 20 mL syringe with flexible minimum volume extension tubing attached to the needle.
- Aseptic technique
- Use nerve stimulation over blind techniques
- Use ultrasound and direct visualisation
- Slow needle advancement
- Do not elicit paraesthesia
- Do not inject when the child complains of pain
- Avoid forceful, fast injections; limit the injection speed to 15–20 mL/min
- Use short bevel ‘blunt’ needles
- Fractionated injections: inject smaller doses and volumes of local anaesthetics (3–5 mL), pause and aspirate (to check for blood) to avoid inadvertent intravascular injection
- Do not inject when high pressures on injection are met; when injection of the first 1 mL of local anaesthetic proves difficult, abandon the injection, withdraw the needle completely and confirm its patency before reinserting
- Use of a 20 mL syringe avoids the generation of high pressures
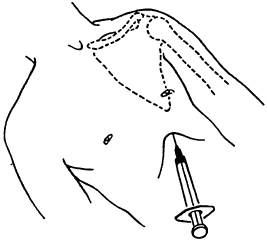
Fascia Iliaca Block
The fascia iliaca block is a modification of the femoral nerve block, and also blocks the lateral cutaneous nerve of thigh. It is simple to learn and a safe way to anaesthetise the femoral nerve in the emergency setting. The block is performed away from the femoral nerve and artery, and so carries a lower risk of neuropraxia or intravascular injection.
Equipment
- A ‘blunt’ (short bevelled) 22 g block needle or an epidural needle to obtain an obvious ‘popping’ sensation as the fascial layers are breached.
Procedure
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree