Delivery of the Head
With each contraction, the vulvovaginal opening is dilated by the fetal head to gradually form an ovoid and finally, an almost circular opening (Fig. 27-1). This encirclement of the largest head diameter by the vulvar ring is termed crowning. Unless an episiotomy has been made as described later, the perineum thins and especially in nulliparous women, may undergo spontaneous laceration. The anus becomes greatly stretched, and the anterior wall of the rectum may be easily seen through it.
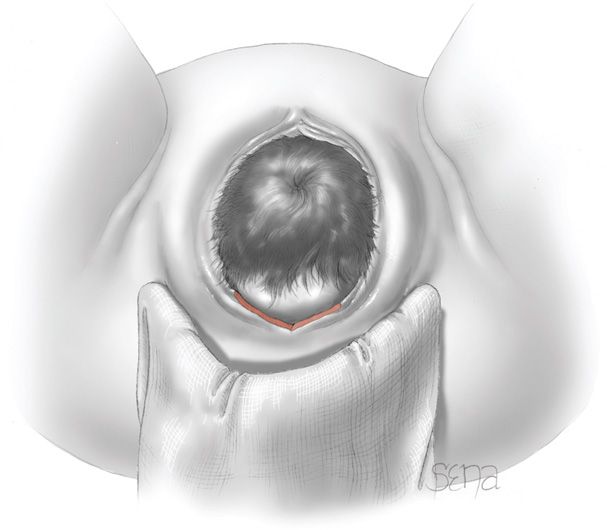
FIGURE 27-1 Delivery of the head. The occiput is being kept close to the symphysis by moderate pressure on the fetal chin at the tip of the maternal coccyx.
There once was considerable controversy concerning routine episiotomy use. It is now clear that episiotomy increases the risk of a tear into the external anal sphincter, the rectum, or both. Conversely, anterior tears involving the urethra and labia are more common in women in whom an episiotomy is avoided. Most, including us, advocate individualization and do not routinely perform episiotomy.
To limit spontaneous vaginal laceration, some perform intrapartum perineal massage to widen the introitus for head passage. With this, the perineum is grasped in the midline by both hands using the thumb and opposing fingers. Outward and lateral stretch against the perineum is then repeatedly applied. Evidence for this technique is limited and mixed regarding efficacy for perineal protection when applied either antepartum or intrapartum (Geranmayeh, 2012; Mei-dan, 2008; Stamp, 2001).
When the head distends the vulva and perineum enough to open the vaginal introitus to a diameter of 5 cm or more, a gloved hand may be used to support the perineum (Fig. 27-2). The other hand is used to guide and control the fetal head to avoid expulsive delivery. Slow delivery of the head may decrease lacerations (Laine, 2008). Alternatively, if expulsive efforts are inadequate or expeditious delivery is needed, the modified Ritgen maneuver may be employed. With this, gloved fingers beneath a draped towel exert forward pressure on the fetal chin through the perineum just in front of the coccyx. Concurrently, the other hand presses superiorly against the occiput (Fig. 27-3). Originally described in 1855, the Ritgen maneuver allows controlled fetal head delivery (Cunningham, 2008). It also favors neck extension so that the head passes through the introitus and over the perineum with its smallest diameters. Comparing the Ritgen maneuver with simple perineal support in 1623 women, Jönsson and colleagues (2008) found a similar incidence of third- and fourth-degree tears—5.5 percent with the maneuver and 4.4 percent with simple support. Last, some espouse a “hands-poised” method, in which the attendant does not touch the perineum during delivery of the head (Mayerhofer, 2002; McCandlish, 1998). Compared with traditional perineal support, this expectant method does not appear to offer greater third-degree laceration protection (Aasheim, 2011).

FIGURE 27-2 Delivery of the head. The mouth appears over the perineum.
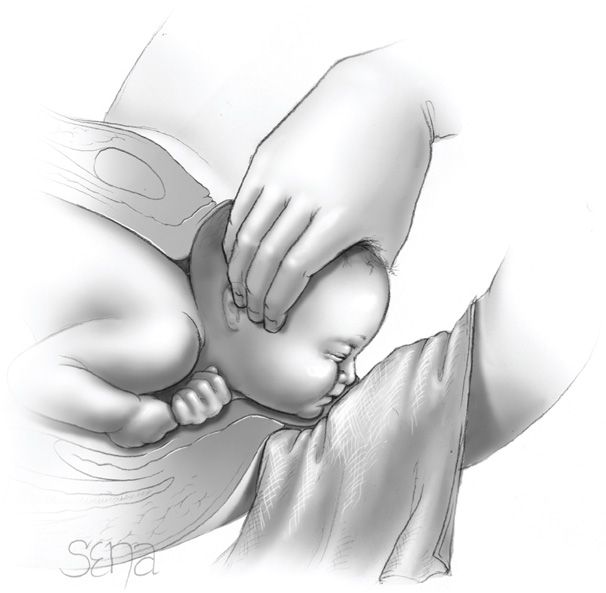
FIGURE 27-3 Modified Ritgen maneuver. Moderate upward pressure is applied to the fetal chin by the posterior hand covered with a sterile towel, while the suboccipital region of the fetal head is held against the symphysis.
 Delivery of the Shoulders
Delivery of the Shoulders
Following delivery of the fetal head, a finger should be passed across the fetal neck to determine whether it is encircled by one or more umbilical cord loops (Fig. 27-4). A nuchal cord is found in approximately 25 percent of deliveries and ordinarily causes no harm. If an umbilical cord coil is felt, it should be slipped over the head if loose enough. If applied too tightly, the loop should be cut between two clamps. Such tight nuchal cords complicate approximately 6 percent of all deliveries but are not associated with worse neonatal outcome than those without a cord loop (Henry, 2013).

FIGURE 27-4 The umbilical cord, if identified around the neck, is readily slipped over the head.
Following its delivery, the fetal head falls posteriorly, bringing the face almost into contact with the maternal anus. The occiput promptly turns toward one of the maternal thighs, and the head assumes a transverse position (Fig. 27-5). This external rotation indicates that the bisacromial diameter, which is the transverse diameter of the thorax, has rotated into the anteroposterior diameter of the pelvis.
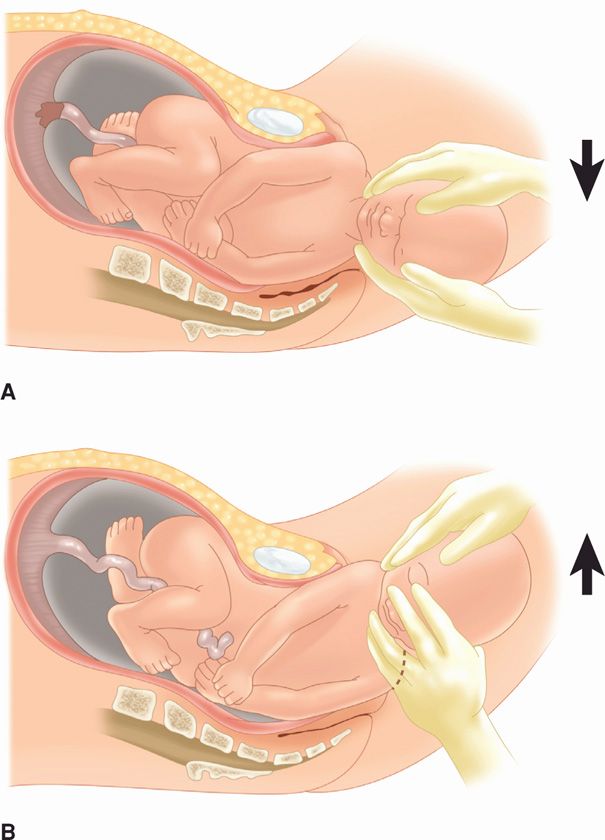
FIGURE 27-5 Delivery of the shoulders. A. Gentle downward traction to effect descent of the anterior shoulder. B. Delivery of the anterior shoulder completed. Gentle upward traction to deliver the posterior shoulder.
Most often, the shoulders appear at the vulva just after external rotation and are born spontaneously. If delayed, extraction aids controlled delivery. The sides of the head are grasped with two hands, and gentle downward traction is applied until the anterior shoulder appears under the pubic arch. Next, by an upward movement, the posterior shoulder is delivered. During delivery, abrupt or powerful force is avoided to avert brachial plexus injury.
The rest of the body almost always follows the shoulders without difficulty. With prolonged delay, however, its birth may be hastened by moderate traction on the head and moderate pressure on the uterine fundus. Hooking the fingers in the axillae is avoided. This can injure upper extremity nerves and produce a transient or possibly permanent paralysis. Traction, furthermore, should be exerted only in the direction of the long axis of the neonate. If applied obliquely, it causes neck bending and excessive brachial plexus stretching. Immediately after delivery of the newborn, there is usually a gush of amnionic fluid, often blood-tinged but not grossly bloody.
Previously, immediate nasopharyngeal bulb suctioning of the newborn was routine to remove secretions. It was found, however, that suctioning of the nasopharynx may lead to neonatal bradycardia (Gungor, 2006). The American Heart Association neonatal resuscitation recommendations currently eschew most suctioning immediately following birth—even with meconium present. This includes bulb syringe aspiration. Suctioning should be reserved for neonates who have obvious obstruction to spontaneous breathing or who require positive-pressure ventilation (Kattwinkel, 2010). Similarly, if meconium is present and the newborn is depressed, then intubation and tracheal suctioning is recommended (American College of Obstetricians and Gynecologists, 2013b). These aspects are discussed in further detail in Chapter 33 (p. 638).
 Clamping the Cord
Clamping the Cord
The umbilical cord is cut between two clamps placed 6 to 8 cm from the fetal abdomen, and later an umbilical cord clamp is applied 2 to 3 cm from its insertion into the fetal abdomen. A plastic clamp that is safe, efficient, and fairly inexpensive, such as the Double Grip Umbilical Clamp (Hollister), is used at Parkland Hospital.
For term neonates, the timing of umbilical cord clamping remains debatable. A delay in umbilical cord clamping for up to 60 seconds may increase total body iron stores, expand blood volume, and decrease anemia incidence in the neonate (Andersson, 2011; Yao, 1974). This may be particularly valuable in populations in which iron deficiency is prevalent (Abalos, 2009). Conversely, and as discussed in Chapter 33 (p. 643), higher hemoglobin concentration increases risks for hyperbilirubinemia and extended hospitalization for neonatal phototherapy (McDonald, 2008). Delayed cord clamping may also hinder timely and needed neonatal resuscitation. Fortunately, in general, delayed umbilical cord clamping compared with early clamping does not worsen Apgar scores, umbilical cord pH, or respiratory distress caused by polycythemia. Regarding maternal outcomes, rates of postpartum hemorrhage are similar between early and delayed clamping groups (Andersson, 2013). Fewer data are available regarding cord “milking,” in which the operator pushes blood through the cord toward the newborn. This maneuver appears safe and may be advantageous if rapid cord clamping is clinically indicated (Upadhyay, 2013).
For the preterm neonate, delayed cord clamping has several benefits. These include higher red cell volume, decreased need for blood transfusion, better circulatory stability, and lower rates of intraventricular hemorrhage and of necrotizing enterocolitis (Rabe, 2012; Raju, 2013; Sommers, 2012).
The American College of Obstetricians and Gynecologists (2012c) has concluded that there is insufficient evidence to support or refute benefits from delayed umbilical cord clamping for term neonates in resource-rich settings. For preterm newborns, however, evidence supports delaying umbilical cord clamping to 30 to 60 seconds after birth. This opinion is also endorsed by the American Academy of Pediatrics (2013). Our policy is to clamp the cord after assessing the need to clear the airway, all of which usually requires approximately 30 seconds. The newborn is not elevated above the introitus at vaginal delivery or much above the maternal abdominal wall at the time of cesarean delivery.
PERSISTENT OCCIPUT POSTERIOR POSITION
Approximately 2 to 10 percent of singleton term cephalic fetuses deliver in an occiput posterior (OP) position (Cheng, 2010). As shown in Figure 27-6, many fetuses delivering OP were occiput anterior (OA) in early labor and reflect malrotation during labor. Predisposing risks include epidural analgesia, nulliparity, greater fetal weight, and prior OP position delivery (Cheng, 2006a; Gardberg, 2004; Lieberman, 2005).
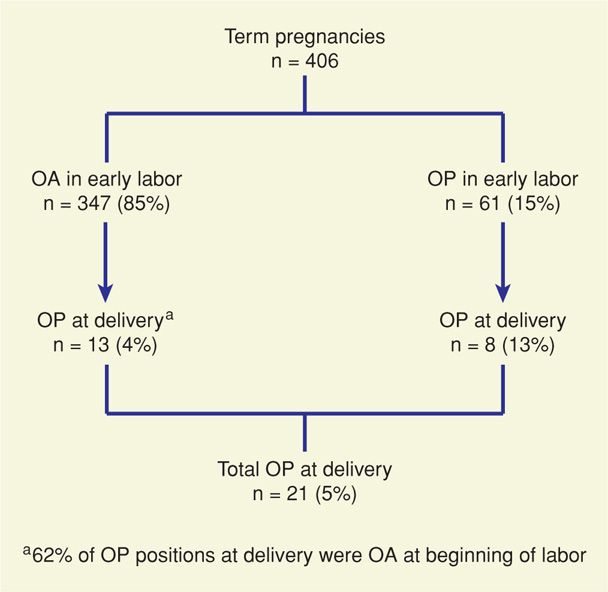
FIGURE 27-6 Occiput posterior (OP) presentation in early labor compared with presentation at delivery. Sonography was used to determine position of the fetal head in early labor. OA = occiput anterior. (Data from Gardberg, 1998.)
 Morbidity
Morbidity
Women with a persistent OP position have higher associated rates of prolonged second-stage labor, cesarean delivery, and operative vaginal delivery. For women who deliver vaginally, rates of blood loss and of third- and fourth-degree laceration, so-called higher-order vaginal lacerations, are increased (Senécal, 2005).
Infants delivered from an OP position have many more complications then those born positioned OA. Cheng and coworkers (2006b) compared outcomes of 2591 women undergoing delivery with a persistent OP position with those of 28,801 women whose newborns were delivered OA. Virtually every possible delivery complication was found more frequently with persistent OP position. Only 46 percent of these women delivered spontaneously, and the remainder accounted for 9 percent of cesarean deliveries performed. These investigators also found that an OP position at delivery was associated with increased adverse short-term neonatal outcomes that included acidemic umbilical cord gases, birth trauma, Apgar scores < 7, and intensive care nursery admission, among others. Similar results were reported by Ponkey (2003) and Fitzpatrick (2001) and their associates.
Methods to prevent persistent OP position and its associated morbidity have been investigated. First, digital examination for identification of fetal head position can be inaccurate, and sonography can be used to increase accuracy (Dupuis, 2005; Souka, 2003; Zahalka, 2005). Such information may provide an explanation for prolonged second-stage labor or may identify suitable candidates for manual rotation. In contrast, varying maternal position either before or during labor does not appear to lower rates of persistent OP position (Desbriere, 2013; Kariminia, 2004).
 Delivery of Persistent Occiput Posterior Position
Delivery of Persistent Occiput Posterior Position
Delivery of a fetus with an OP position may be completed by spontaneous or operative vaginal delivery. First, if the pelvic outlet is roomy and the vaginal outlet and perineum are somewhat relaxed from prior deliveries, rapid spontaneous OP delivery will often take place. Conversely, if the vaginal outlet is resistant to stretch and the perineum is firm, second-stage labor may be appreciably prolonged. During each expulsive effort, the head is driven against the perineum to a much greater degree than when the head position is OA. This leads to greater rates of higher-order perineal lacerations (Groutz, 2011; Melamed, 2013).
In some cases, spontaneous vaginal delivery from an OP position does not appear feasible or expedited delivery is needed. Here, manual rotation with spontaneous delivery from an OA position may be preferred. This technique is described fully in Chapter 29 (p. 580). Successful rotation rates range from 47 to 90 percent. And, as would be expected, lower rates of cesarean delivery, vaginal laceration, and maternal blood loss follow rotation to OA position and vaginal delivery (Le Ray, 2005; Sen, 2013; Shaffer, 2006, 2011). Disadvantageously, manual rotation is linked with higher cervical laceration rates. Thus, careful inspection of the cervix following rotation is prudent.
For exigent delivery, forceps or vacuum device can be applied to a persistent OP position. This is often performed in conjunction with an episiotomy. Also, if the head is engaged, the cervix fully dilated, and the pelvis adequate, forceps rotation may be attempted. These circumstances most likely prevail when expulsive efforts of the mother during the second stage are ineffective. Both these operative vaginal techniques are detailed in Chapter 29 (p. 582).
Infrequently, protrusion of fetal scalp through the introitus is the consequence of marked elongation of the fetal head from molding combined with formation of a large caput succedaneum. In some cases, the head may not even be engaged—that is, the biparietal diameter may not have passed through the pelvic inlet. In these, labor is characteristically long and descent of the head is slow. Careful palpation above the symphysis may disclose the fetal head to be above the pelvic inlet. Prompt cesarean delivery is appropriate.
At Parkland Hospital, spontaneous delivery or manual rotation is preferred for management of persistent OP position. In other cases, either manual rotation to OA position followed by forceps delivery or forceps delivery from the OP position is used. If neither can be completed with relative ease, cesarean delivery is performed.
OCCIPUT TRANSVERSE POSITION
In the absence of a pelvic architecture abnormality or asynclitism, the occiput transverse position is usually transitory. Thus, unless contractions are hypotonic, the head usually spontaneously rotates to an OA position. If hypotonic uterine contractions are suspected and cephalopelvic disproportion is absent, then an oxytocin infusion can be used to stimulate labor.
If rotation ceases because of poor expulsive forces, vaginal delivery usually can be accomplished readily in a number of ways. The easiest is manual rotation of the occiput either anteriorly to OA or less commonly, posteriorly to OP. If either is successful, Le Ray and coworkers (2007) reported a 4-percent cesarean delivery rate compared with a 60-percent rate in women in whom manual rotation was not successful. Some recommend rotation with Kielland forceps for the persistent occiput transverse position as outlined in Chapter 29 (p. 582). These forceps are used to rotate the occiput to the anterior position, and delivery is accomplished with the same forceps or by substitution with either Simpson or Tucker–McLane forceps.
In some cases, there may be an underlying cause leading to the persistent occiput transverse position that is not easily overcome. For example, a platypelloid pelvis is flattened anteroposteriorly and an android pelvis is heart shaped. With these, there may be inadequate space for occipital rotation to either an OA or OP position (Fig. 2-20, p. 34). Because of these concerns, undue force should be avoided if forceps delivery is attempted.
SHOULDER DYSTOCIA
Following complete emergence of the fetal head during vaginal delivery, the remainder of the body may not rapidly follow. The anterior fetal shoulder can become wedged behind the symphysis pubis and fail to deliver using normally exerted downward traction and maternal pushing. Because the umbilical cord is compressed within the birth canal, such dystocia is an emergency. Several maneuvers, in addition to downward traction on the fetal head, may be performed to free the shoulder. This requires a team approach, in which effective communication and leadership are critical.
Consensus regarding a specific definition of shoulder dystocia is lacking. Some investigators focus on whether maneuvers to free the shoulder are needed, whereas others use the head-to-body delivery time interval as defining (Beall, 1998). Spong and coworkers (1995) reported that the mean head-to-body delivery time in normal births was 24 seconds compared with 79 seconds in those with shoulder dystocia. These investigators proposed that a head-to-body delivery time > 60 seconds be used to define shoulder dystocia. Currently, however, the diagnosis continues to rely on the clinical perception that the normal downward traction needed for fetal shoulder delivery is ineffective.
Because of these differing definitions, the incidence of shoulder dystocia varies. Current reports cite an incidence between 0.6 percent and 1.4 percent (American College of Obstetricians and Gynecologists, 2012b). There is evidence that the incidence has increased in recent decades, likely due to increasing fetal birthweight (MacKenzie, 2007). Alternatively, this increase may be due to more attention given to appropriate documentation of dystocia (Nocon, 1993).
 Maternal and Neonatal Consequences
Maternal and Neonatal Consequences
In general, shoulder dystocia poses greater risk to the fetus than the mother. Postpartum hemorrhage, usually from uterine atony but also from vaginal lacerations, is the main maternal risk (Jangö, 2012; Rahman, 2009). In contrast, significant neonatal neuromusculoskeletal injury and even mortality are concerns. MacKenzie and associates (2007) reviewed 514 cases of shoulder dystocia and found that 11 percent were associated with serious neonatal trauma. Brachial plexus injury was diagnosed in 8 percent, and 2 percent suffered a clavicle, humeral, or rib fracture. Seven percent showed evidence of acidosis at delivery, and 1.5 percent required cardiac resuscitation or developed hypoxic ischemic encephalopathy. Mehta and colleagues (2007) found a similar number of injuries in a study of 205 shoulder dystocia cases, in which 17 percent had injury. Again, most involved the brachial plexus. These specific injuries are described more fully in Chapter 33 (p. 648). Of predictors, increasing fetal weight, maternal body mass index, and second-stage duration and a prior shoulder dystocia appear to raise the neonatal injury risk with shoulder dystocia (Bingham, 2010; Mehta, 2006).
 Prediction and Prevention
Prediction and Prevention
There has been considerable evolution in obstetrical thinking regarding the preventability of shoulder dystocia. Although there are clearly several risk factors associated with this complication, identification of individual instances before the fact has proved to be impossible. The American College of Obstetricians and Gynecologists (2012b) reviewed studies and concluded that:
1. Most cases of shoulder dystocia cannot be accurately predicted or prevented.
2. Elective induction of labor or elective cesarean delivery for all women suspected of having a macrosomic fetus is not appropriate.
3. Planned cesarean delivery may be considered for the nondiabetic woman with a fetus whose estimated fetal weight is > 5000 g or for the diabetic woman whose fetus is estimated to weigh > 4500 g.
Birthweight
Commonly cited maternal characteristics associated with increased fetal birthweight are obesity, postterm pregnancy, multiparity, diabetes, and gestational diabetes. There is universal agreement that increasing birthweight is associated with an increasing incidence of shoulder dystocia. In one study of nearly 2 million vaginal deliveries, Overland and coworkers (2012) noted that in 75 percent of shoulder dystocia cases, newborns weighed > 4000 g. That said, the concept that cesarean delivery is indicated for large fetuses, even those estimated to weigh 4500 g, should be tempered. Rouse and Owen (1999) concluded that a prophylactic cesarean delivery policy for macrosomic fetuses would require more than 1000 cesarean deliveries with attendant morbidity as well as millions of dollars to avert a single permanent brachial plexus injury.
Intrapartum Factors
Some labor characteristics have been associated with an increased shoulder dystocia risk and include prolonged second-stage labor, operative vaginal delivery, and prior shoulder dystocia (Mehta, 2004; Moragianni, 2012; Overland, 2009). Of these, the risk of recurrent shoulder dystocia ranges from 1 to 13 percent (Bingham, 2010; Moore, 2008; Ouzounian, 2013). For many women with prior shoulder dystocia, a trial of labor may be reasonable. The American College of Obstetricians and Gynecologists (2012b) recommends that estimated fetal weight, gestational age, maternal glucose intolerance, and severity of prior neonatal injury be evaluated and risks and benefits of cesarean delivery discussed with any woman with a history of shoulder dystocia. After discussion, either mode of delivery is appropriate.
 Management
Management
Because shoulder dystocia cannot be accurately predicted, clinicians should be well versed in its management principles. Because of ongoing cord compression with this dystocia, one goal is to reduce the head-to-body delivery time. This is balanced against the second goal, which is avoidance of fetal and maternal injury from aggressive manipulations. Accordingly, an initial gentle attempt at traction, assisted by maternal expulsive efforts, is recommended. Adequate analgesia is certainly ideal. Some clinicians advocate performing a large episiotomy to provide room for manipulations. Of note, Paris (2011) and Gurewitsch (2004) and their colleagues reported no change in the brachial plexus injury rate for groups in which episiotomy was not performed during shoulder dystocia management.
After gentle traction, various techniques can be used to free the anterior shoulder from its impacted position behind the symphysis pubis. Of these, moderate suprapubic pressure can be applied by an assistant, while downward traction is applied to the fetal head. Pressure is applied with the heel of the hand to the anterior shoulder wedged above and behind the symphysis. The anterior shoulder is thus either depressed or rotated, or both, so the shoulders occupy the oblique plane of the pelvis and the anterior shoulder can be freed.
The McRoberts maneuver was described by Gonik and associates (1983) and named for William A. McRoberts, Jr., who popularized its use at the University of Texas at Houston. The maneuver consists of removing the legs from the stirrups and sharply flexing them up onto the abdomen (Fig. 27-7). Gherman and associates (2000) analyzed the McRoberts maneuver using x-ray pelvimetry. They found that the procedure caused straightening of the sacrum relative to the lumbar vertebrae, rotation of the symphysis pubis toward the maternal head, and a decrease in the angle of pelvic inclination. Although this does not increase pelvic dimensions, pelvic rotation cephalad tends to free the impacted anterior shoulder. Gonik and coworkers (1989) tested the McRoberts position objectively with laboratory models and found that the maneuver reduced the forces needed to free the fetal shoulder.

FIGURE 27-7 The McRoberts maneuver. The maneuver consists of removing the legs from the stirrups and sharply flexing the thighs up onto the abdomen. The assistant is also providing suprapubic pressure simultaneously (arrow).
Another maneuver, delivery of the posterior shoulder, consists of carefully sweeping the posterior arm of the fetus across its chest, followed by delivery of the arm. The shoulder girdle is then rotated into one of the oblique diameters of the pelvis with subsequent delivery of the anterior shoulder (Fig. 27-8).
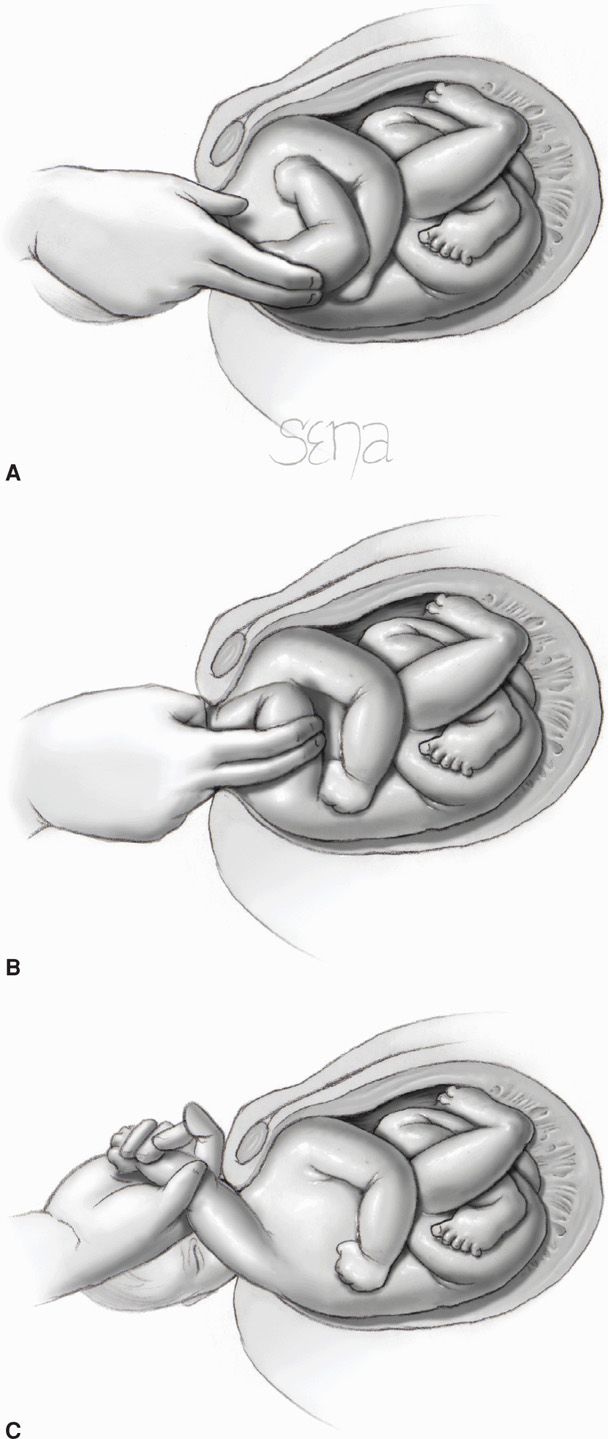
FIGURE 27-8 Delivery of the posterior shoulder for relief of shoulder dystocia. A. The operator’s hand is introduced into the vagina along the fetal posterior humerus. B. The arm is splinted and swept across the chest, keeping the arm flexed at the elbow. C. The fetal hand is grasped and the arm extended along the side of the face. The posterior arm is delivered from the vagina.
Woods (1943) reported that by progressively rotating the posterior shoulder 180 degrees in a corkscrew fashion, the impacted anterior shoulder could be released. This is frequently referred to as the Woods corkscrew maneuver (Fig. 27-9). Rubin (1964) recommended two maneuvers. First, the fetal shoulders are rocked from side to side by applying force to the maternal abdomen. If this is not successful, the pelvic hand reaches the most easily accessible fetal shoulder, which is then pushed toward the anterior surface of the chest. This maneuver most often abducts both shoulders, which in turn produces a smaller shoulder-to-shoulder diameter. This permits displacement of the anterior shoulder from behind the symphysis (Fig. 27-10).
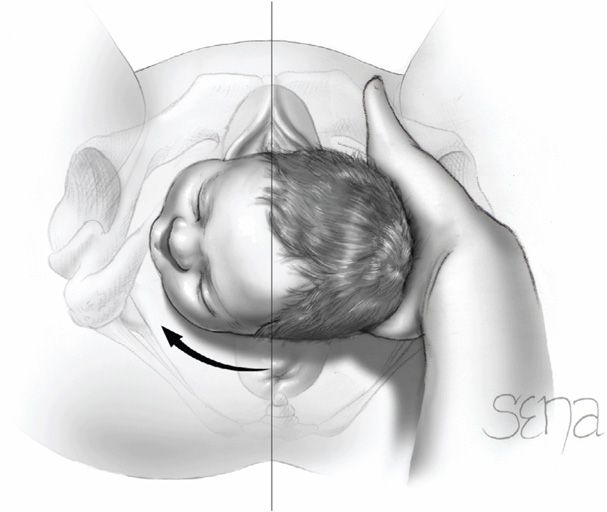
FIGURE 27-9 Woods maneuver. The hand is placed behind the posterior shoulder of the fetus. The shoulder is then rotated progressively 180 degrees in a corkscrew manner so that the impacted anterior shoulder is released.
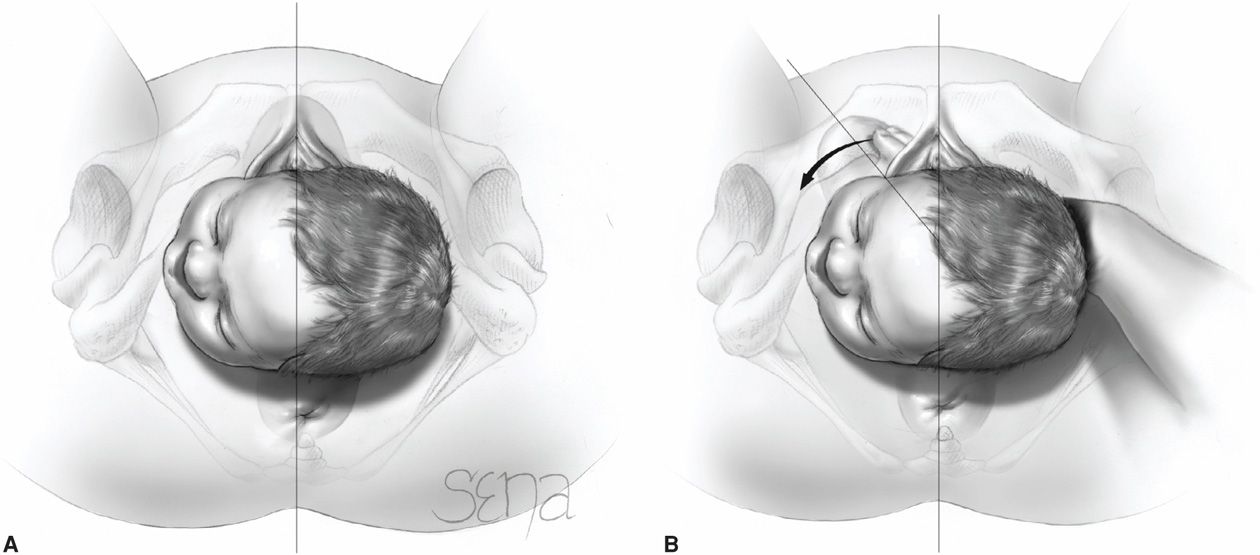
FIGURE 27-10 The second Rubin maneuver. A. The shoulder-to-shoulder diameter is aligned vertically. B. The more easily accessible fetal shoulder (the anterior is shown here) is pushed toward the anterior chest wall of the fetus (arrow). Most often, this results in abduction of both shoulders, which reduces the shoulder-to-shoulder diameter and frees the impacted anterior shoulder.
Importantly, progression from one maneuver to the next should be organized and methodical. As noted, the urgency to relieve the dystocia should be balanced against potentially injurious traction forces and manipulations. Lerner and coworkers (2011) in their evaluation of 127 shoulder dystocia cases reported that all neonates without sequelae from shoulder dystocia were born by 4 minutes. Conversely, most depressed neonates—57 percent—had head-to-body delivery intervals > 4 minutes. The percentage of depressed neonates rose sharply after 3 minutes.
Deliberate fracture of the anterior clavicle by using the thumb to press it toward and against the pubic ramus can be attempted to free the shoulder impaction. In practice, however, deliberate fracture of a large neonate clavicle is difficult. If successful, the fracture will heal rapidly and is usually trivial compared with brachial nerve injury, asphyxia, or death.
Hibbard (1982) recommended that pressure be applied to the fetal jaw and neck in the direction of the maternal rectum, with strong fundal pressure applied by an assistant as the anterior shoulder is freed. Strong fundal pressure, however, applied at the wrong time may result in even further impaction of the anterior shoulder. Gross and associates (1987) reported that fundal pressure in the absence of other maneuvers “resulted in a 77-percent complication rate and was strongly associated with (fetal) orthopedic and neurologic damage.”
Sandberg (1985) reported the Zavanelli maneuver for cephalic replacement into the pelvis followed by cesarean delivery. The first part of the maneuver consists of returning the head to the occiput anterior or posterior position. Terbutaline, 0.25 mg, is given subcutaneously to produce uterine relaxation. The operator flexes the head and slowly pushes it back into the vagina. Cesarean delivery is then performed. Sandberg (1999) reviewed 103 reported cases in which the Zavanelli maneuver was used. It was successful in 91 percent of cephalic cases and in all cases of breech head entrapments. Despite successful replacement, fetal injuries were common but may have resulted from the multiple manipulations used before the Zavanelli maneuver (Sandberg, 2007). Six stillbirths, eight neonatal deaths, and 10 neonates who suffered brain damage were described. Uterine rupture also was reported.
Symphysiotomy, in which the intervening symphyseal cartilage and much of its ligamentous support is cut to widen the symphysis pubis, is described in Chapter 28 (p. 567). It has been used successfully for shoulder dystocia (Hartfield, 1986). Goodwin and colleagues (1997) reported three cases in which symphysiotomy was performed after the Zavanelli maneuver had failed. All three neonates died, and maternal morbidity was significant due to urinary tract injury. Cleidotomy consists of cutting the clavicle with scissors or other sharp instruments and is usually done for a dead fetus (Schramm, 1983).
Hernandez and Wendel (1990) suggested use of a shoulder dystocia drill to better organize emergency management:
1. Call for help—mobilize assistants and anesthesia and pediatric personnel. Initially, a gentle attempt at traction is made. Drain the bladder if it is distended.
2. A generous episiotomy may be desired to afford room posteriorly.
3. Suprapubic pressure is used initially by most practitioners because it has the advantage of simplicity. Only one assistant is needed to provide suprapubic pressure, while normal downward traction is applied to the fetal head.
4. The McRoberts maneuver requires two assistants. Each assistant grasps a leg and sharply flexes the maternal thigh against the abdomen.
These maneuvers will resolve most cases of shoulder dystocia.
If the above listed steps fail, the following steps may be attempted, and any of the maneuvers may be repeated:
5. Delivery of the posterior arm is attempted. With a fully extended arm, however, this is usually difficult to accomplish.
6. Woods screw maneuver is applied.
7. Rubin maneuver is attempted.
Other techniques generally should be reserved for cases in which all other maneuvers have failed. These include intentional fracture of the anterior clavicle and the Zavanelli maneuver. The American College of Obstetricians and Gynecologists (2012b) has concluded that no one maneuver is superior to another in releasing an impacted shoulder or reducing the chance of injury. Performance of the McRoberts maneuver, however, was deemed a reasonable initial approach. The College (2012a) also has created a Patient Safety Checklist to guide the documentation process with shoulder dystocia.
Shoulder dystocia training and protocols using simulation-based education and drills has evidence-based support. These tools improve performance and retention of drill steps (Buerkle, 2012; Crofts, 2008; Grobman, 2011). Their use has translated into improved neonatal outcome in some, but not all, investigations (Draycott, 2008; Inglis, 2011; Walsh, 2011).
SPECIAL POPULATIONS
Typical vaginal delivery may be challenging in women with perineal limitations or with a large anomalous fetus. Delivery in women with prior pelvic reconstructive surgeries and in those with scarring from female genital mutilation is described here. The special needs of women with congenital vaginal septa, giant condyloma, Crohn disease, or connective-tissue disorders are discussed in chapters covering those topics.
 Female Genital Mutilation
Female Genital Mutilation
Inaccurately called female circumcision, mutilation refers to medically unnecessary vulvar and perineal modification. In the United States it is a federal crime to perform unnecessary genital surgery on a girl younger than 18 years. That said, forms of female genital mutilation are practiced in countries throughout Africa, the Middle East, and Asia. As many as 130 million women worldwide have undergone one of these procedures, and approximately 230,000 live in the United States (Nour, 2006). Cultural sensitivity is imperative, because many women may be offended by the suggestion that they have been assaulted or mutilated (American College of Obstetricians and Gynecologists, 2007).
The World Health Organization (1997) classifies genital mutilations into four types (Table 27-1). Complications include infertility, dysmenorrhea, diminished sexual quality of life, and propensity for vulvovaginal infection (Almroth, 2005; Andersson, 2012; Nour, 2006). In general, women with significant symptoms following type III procedures are candidates for corrective surgery. Specifically, division of midline scar tissue to reopen the vulva is termed defibulation or deinfibulation.
TABLE 27-1. World Health Organization Classification of Female Genital Mutilation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


