The uterine contractions that were one in every 2–2.5 min become one in every minute without any escalation of the oxytocin infusion precipitating prolonged deceleration. This is due to increasing sensitivity of the uterus to the same dose of oxytocin with advancing cervical dilatation.
Measurement of Uterine Activity: The Need and the Methods
Uterine activity has four components: resting uterine tone, frequency, amplitude and duration (Table 5.1). For clinical purposes, information about resting uterine tone is not needed in almost all cases other than in a few high-risk situations. With a uterine rupture the tone may be lost and with abruption there may be an increase. In these situations the clinical evaluation will point to the problem, in addition to the information on uterine tone. Prostaglandin or oxytocin use may also raise the resting tone but usually they are associated with markedly increased frequency of contractions. The presence of contractions and whether there is an increase in frequency and duration and whether they are regular is of value to manage preterm labour, i.e. to decide to inhibit contractions. In term labour, if there is slow progress of labour and there is inadequate uterine activity with no evidence of fetal compromise, augmentation of contractions may help with progress of labour and vaginal delivery.
| Parameter | Definition |
|---|---|
| Relaxation time | Time in seconds between offset of one contraction and onset of the next |
| Contraction duration | Duration in seconds between onset and offset of contractions |
| Contraction amplitude | Maximum uterine pressure above basal tone in mmHg |
| Contraction area | Area of contraction above baseline pressure in mmHg seconds |
| Contraction frequency | Number of contractions in a 10 min period |
In addition to the usefulness in inhibiting or augmenting contractions, it is of value to identify whether the fetus is likely to be compromised by the contractions that reduce or cut off the blood supply to the retro-placental area that produce late decelerations or compress the umbilical cord which cause variable decelerations. Monitoring the fetal heart rate (FHR) during and soon after contractions could pick up these decelerations. Identifying such compromise related to uterine contraction would prompt us to stop oxytocin infusion or to give tocolytic drugs.
Maternal Perception
All women feel painful uterine contractions during labour, although how they perceive the intensity may vary. Mothers in different cultures and women in the same culture react differently to pain. Obese women may have difficulties feeling the uterine contractions and parous women may feel the contractions to be less painful [9]. Maternal perception of the frequency of contractions can be relied upon, the duration is an approximation, but their assessment of intensity may not have any relationship to measured amplitude of uterine contractions. It is known that contractions with amplitudes of greater than 15 mmHg from the baseline is associated with pain and is also effective in bringing about cervical effacement and dilatation.
Contraction Assessment by Manual Palpation
Globally the commonest method of uterine contraction assessment is by palpation. Palpation provides a reliable assessment of frequency, but an approximation of the duration as the very start and end of contractions may be difficult to palpate [10]. Palpation will not be able to provide information on the strength or intensity, although in many centres the care givers make comments stating that the contractions are strong, moderately strong or weak – this has no scientific basis. The advantage of palpation is that it promotes the rapport between the care giver and the woman, does not need expensive technology and is adequate to manage most labours. Palpation can be done in any position adopted by the mother, i.e. lying, sitting, standing or in the water pool. Palpation is performed over a 10 min period, is assessed every 30 min and is plotted on the partogram (see Figure 2.2 in Chapter 2). The plotting in the partogram provides the frequency of contractions in 10 min and the average duration shaded differently for <20 sec, 20–40 sec and >40 sec.
Contraction Assessment by External Tocography
Uterine contractions cause the uterus to expand in an antero-posterior direction that causes protrusion of the abdomen in the uterine fundal region. An external pressure transducer placed between the fundus and the umbilicus perceives this change due to the thrust on the button or diaphragm of the transducer. This helps to monitor contraction frequency, duration and amplitude. Most fetal monitors provide for adjustment of baseline tone or pressure that is usually set at 20 mmHg. When applied properly, this non-invasive method of monitoring provides accurate assessment of the frequency, near accurate measurement of the duration, but only a relative assessment of the amplitude. The amplitude is much less accurate in obese women, in a restless woman or when the belt is loose [11]. External tocography does not assess the baseline pressure, which can be increased on the recording by tightening the toco transducer belt or by manipulating the toco button on the machine. The continuous display of contractions in relation to the fetal heart rate, i.e. cardiotocography (CTG), is useful to monitor high-risk labours [12]. More accurate assessment of baseline pressure, frequency, duration and amplitude can be obtained by internal tocography [13].
Contraction monitoring in the second stage of labour should be meticulous as the contraction frequency is maximal with risks to the fetus, especially when a woman is on oxytocin infusion (Figure 5.1). Medical negligence cases point to poor or no monitoring of contractions in the second stage and this may be due to the woman squatting or in the pool, or flicking the transducer to make the sensor face upwards, or loosening it due to discomfort. In such situations the contractions should be assessed by external palpation and a mark made on the CTG recording to indicate when the contractions occurred.
At times the ultrasound transducer can display the maternal heart rate (MHR) on CTG, especially in the second stage when the FHR is bradycardic. Normally the MHR accelerates coinciding with contractions in the second stage, while the FHR decelerates due to head compression. Despite these physiological differences that should alert the care giver, mistakes are made by continuing to monitor the MHR, thinking it is the FHR. To overcome this problem some toco transducers have inbuilt optical sensors which would identify the MHR from the maternal abdominal skin and record it separately on the CTG paper (Figure 5.2).
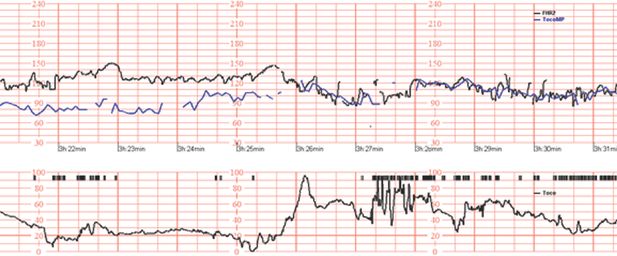
CTG recording that shows contractions, FHR and MHR.
Contraction Assessment by Internal Tocography
Intrauterine pressure measurement provides an accurate measure of resting tone, frequency, duration and amplitude [14]. It is used almost routinely in some centres/countries but is not popular universally because of the invasive nature of placing an intrauterine catheter in utero via the cervical canal and due to lack of clear evidence of benefit in clinical practice. The advantages are that pressure recordings are not influenced by the position of the mother and some catheters have ports for amnioinfusion when there is meconium-stained amniotic fluid or variable decelerations. Intra-amniotic placement provides more reliable readings compared with catheters placed in the extra amniotic space [15]. Complications of intrauterine pressure measurements are rare but include intrauterine infection, exceptionally perforation of fetal or placental vessels and injury to the fetus or the uterus [16,17].
Different types of catheters (fluid-filled, fibre-optic, pressure transducer-tipped) are available and provide reliable readings, but solid-tipped catheters are preferred as fluid-filled catheters may require more frequent adjustment and have an increased tendency for artefacts due to air bubbles, kinked cables and catheter occlusion by meconium, blood or fetal parts [18]. Figure 5.3 shows the transducer-tipped catheter with a bridge strain gauge deposited on a thin metal pressure-sensing surface at the end of a 90 cm catheter. The sensing area is recessed to minimize damage and lateral pressure measurements. Placement of flexible fibre-optic catheters is associated with hardly any placental or fetal injury. These catheters do not get damaged and can be used in the second stage of labour [19]. New dual-channel, multifunctional uterine probes and balloon probes were introduced for accurate FHR monitoring in addition to measurement of uterine activity, but are not readily available for clinical use [20].

The tip of a fibre-optic catheter with a smooth dome and distal fenestration housing the mirror arrangement is shown alongside the tip of the Gaeltec catheter with a recessed area behind the rounded tip.
Since there are possibilities of different pockets of fluid in the uterine cavity with little connection, the pressure measurement in one pocket of fluid may be different from another. When two catheters were placed in different sections of the uterus, small differences in the amplitude of contractions were observed but cumulative uterine activity was not so different as to influence clinical management [21,22]. The slight differences in pressure may be due to mechanical (direct force) rather than fluid pressure acting on the transducer.
Randomized controlled trials (RCTs) comparing external to internal tocography have failed to show any benefit in clinical outcome in terms of reduction of CS, operative vaginal delivery or better neonatal outcome in augmented labour [23,24]. This may be due to the fact that labour is managed by considering mainly the frequency of uterine contractions that are assessed reasonably well by external tocography even in the moderately obese. Studies have also shown no advantage of internal monitoring in induced labour [25]. There may be a special group of women who may benefit by internal tocography, i.e. where external tocography is not providing the needed information of frequency and duration of contractions due to severe obesity or restlessness. It is postulated that intrauterine pressure monitoring may be of value in women who are in labour with a previous CS scar, but there is no evidence to recommend such use.
Uterine Electromyography (EMG)
Measurements of uterine activity by EMG obtained by external abdominal probes provide nearly as accurate readings as those obtained by intrauterine pressure catheters [26,27]. Early studies suggested the possibility of detecting contractions that may lead to preterm labour from those that are unlikely to progress to labour by looking at the synchronous wave patterns from various parts of the uterus using a multi-channel myographic recording [28]. The complexity of equipment needed for EMG measurement that would measure the synchronization and concordance of contractions is constantly being improved and may find clinical usefulness in the future [29].
Quantification of Uterine Activity
Uterine activity has been expressed simply based on the baseline tone, frequency, duration and amplitude of contractions. Efficiency of contractions is not judged by the measurements but by what they are expected to achieve, i.e. cervical effacement and dilatation of the cervix, followed by descent of the head and delivery of the fetus, followed by the placenta and membranes. If a woman has few contractions that are of short duration but labour is progressing well, then she would not need augmentation of labour. Similarly, contractions may be in-coordinate (Figures 2.5 and 2.6), i.e. a few contractions together followed by single contractions every few minutes followed by another series of contractions together. Hence the description of in-coordinate contractions is based on what is seen on tocography. However, in-coordinate contractions do not mean that these contractions are inefficient.
In order to improve assessment of uterine activity by making maximum use of the measurements obtained, individual elements of the tocograph are considered and combined in different ways, e.g. multiplying mean amplitude of contractions over 10 min by the frequency of contractions, i.e. Montevideo units. Total contraction area is considered by calculating the area under a contraction, including the resting pressure. The basal intrauterine pressure is the pressure at the lowest point of the tracing between contractions, due to atmospheric pressure, hydrostatic pressure and elastic recoil of the uterus and surrounding tissues, and is unlikely to contribute to cervical dilatation or descent of the head [5]. Hence this pressure is excluded from quantitative measures because it is affected by variables that are not related to uterine activity. The refined measure is to calculate the active contraction area by considering only the area above the resting pressure and hence considering the active pressure, which is the difference between the maximum intrauterine pressure and the resting intrauterine pressure (Figure 5.4). In order to capture all the activity of the uterus in a continuous manner including that due to in-coordinate contractions, i.e. to calculate the total work done, continuous measurement of activity every 15 min was introduced as kPa secs/15 minutes, and this can be automatically calculated and reflected on the CTG paper as a horizontal mark read against a vertical axis of 0–2500 kPa secs (Figure 5.5) [11].
Recording of UAI as a short dark line against a vertical axis from 0 to 2500 kPa secs and the numerical printout of the UAI in addition to mode of recording, paper speed and time.
The clinical situations of sudden change in posture, e.g. sitting up or squatting, uterine hyper-stimulation by PG or oxytocin infusion, irritation of the uterus due to blood seeping into the myometrium in cases of abruption, can increase the baseline pressure and need to be recognized [30,31]. The shape of the contraction may be related to dysfunctional labour. The shape is measured by the F:R ratio, where the F (fall) is the time for a contraction to return to baseline from its peak and the R (rise) is the time for a contraction to rise to its peak [32]. An increased F:R ratio is associated with a higher need for caesarean delivery, although this concept needs further study [33]. The total amount of uterine activity per unit time can be described in different ways (see Table 5.2).
| Unit of measurement | Components considered | Comments |
|---|---|---|
| Montevideo unit [34] | Mean amplitude × mean frequency over 10 min | The duration and shape of the contractions not considered |
| Alexandria unit [35] | Montevideo × unit mean duration over 10 min | Shape not considered. Incorporating duration showed longer duration was associated with shorter labour |
| Uterine activity unit (UAU) [36] | Area under the pressure curve (Torr-min) over 1 min – 1UAU = 1 Torr-min (included frequency, duration and amplitude) | Included baseline pressure which did not actively contribute to uterine work |
| Uterine activity integral (UAI) or active contraction area [37] | Active area under the pressure curve over 15 min (intrauterine pressure minus the baseline pressure) (Figure 5.5) | Active pressure measurements may include maternal efforts, in the second stage |
| Mean active pressure (MAP) [38] | UAI divided by 900 (kPa), measuring over 1 sec (15 min × 60 = 900 sec) | Complex measurement but is independent of duration |
| Mean contraction active pressure (MCAP) [38] | UAI/total duration of contraction | When the integration period is with respect to one contraction |
Uterine Activity Measurement
The cumulative work done by the uterus has been expressed by taking different elements of the components of the uterine contractions (Table 5.2).
Uterine activity measurements may concentrate on the work done by the uterus, but one needs to remember that too frequent contractions of low amplitude may be reflected as low uterine activity but may compromise the fetus especially if one increases the oxytocin infusion to achieve a higher uterine activity. Hence it is important not to increase the oxytocin infusion to achieve more than four or five contractions in 10 min while trying to increase the uterine activity measurements performed by Montevideo units or UAIs. The in-coordinate nature and shape of contractions are not considered with area measurements. Despite sophistication in equipment and technology and different methods of quantifying, internal tocography and quantifying uterine activity has not improved the clinical outcome in spontaneous, augmented or induced labour [39,40].
Uterine Activity in Normal Labour
A healthy, well-grown fetus with normal amniotic fluid and no medical or obstetric disorder is not easily compromised by uterine contractions of spontaneous normal labour. The contractions of labour start infrequently from about one in ten minutes. Gradually it increases in frequency, duration and amplitude. The uterine activity peaks towards the end of the first stage due to the ‘Ferguson reflex’, which is due to the reflex release of oxytocin due to the presenting part stretching the almost fully dilated cervix and the upper vagina. Towards the end of the first stage of labour the contraction frequency may be 3–5 in 10 min, with each contraction lasting longer than 60 sec and with amplitudes of >50 mmHg. In cases with slow progress of labour, oxytocin titration to achieve a contraction frequency of four in 10 min leads to satisfactory progress [41]. A contraction frequency greater than 5 min may reduce the uterine relaxation time. It has been shown that if this time is less than 51 sec in the first stage and 36 sec in the second stage it may lead to fetal compromise [42]. It is simple to understand that increase in the contraction frequency and a decrease in relaxation time would be associated with lower umbilical artery pH. Infrared spectroscopic studies have shown that fetal cerebral oxygen saturation remains stable or even increases if the contractions are every 2–3 min or longer [43].
Uterine Contractions and Parity
Studies on oxytocin-induced labour evaluated the total uterine activity needed to achieve full dilatation of the cervix. The total uterine activity needed is influenced by the parity and cervical score and reflects the work needed to overcome the cervical and pelvic tissue resistance [44].
If a woman has not reached full dilatation despite the uterine activity exceeding the total uterine activity which is the norm for that cervical score and parity, and there are associated clinical signs of failure in cervical dilatation, increasing caput and moulding with no progress, then it suggests cephalo-pelvic disproportion. Since some women in the same parity group progress normally with low levels of uterine activity and there is a broad spectrum of uterine activity associated with normal progress of labour, it is difficult to prognosticate possible labour progress based on uterine activity [45,46] (Figure 5.6). Hence labour progress needs to be monitored by assessing the progress of cervical dilatation. If partographic progress is normal, then uterine activity measurements would not be of great value. The parous uterus needs to expend significantly less effort to affect normal vaginal delivery than its nulliparous counterpart until the late first stage, suggesting that parity may have a greater influence on the resistance offered by the cervix than the pelvic tissues [47].
Cervical dilatation-specific uterine activity in kPa/15 min in nulliparous spontaneous normal labour.
Maternal Characteristics that Affect Uterine Contractions
Increasing body mass index in our population, especially in the reproductive age group, is partly to blame for slow and prolonged labour and the cause for increasing CSs. This may be due to poor uterine contractility or larger babies, or decreased available space in the pelvis or for a combination of all three [48]. The poor contractility is attributed to the in-vitro findings that relate to elevated cholesterol in obese women that may disrupt the signalling mechanisms that impair contractions [49]. Intracellular acidification decreases and alkalization increases contractility [50]. In recent times, amniotic fluid lactate is measured to identify myometrial hypoxia and lactic acidosis associated with dysfunctional labour [51]. Early research of preloading the mother with bicarbonate solutions suggests this appears to reduce the incidence of intrauterine lactic acidosis, just as with muscles in athletes, but this aspect needs further study. Such interventions may help to reduce the incidence of dysfunctional labour.
Uterine Contractions and Previous Caesarean Section (CS)
The main concern in labour with a previous CS scar is the possibility that the scar may give way and cause morbidity to the mother and severe morbidity or mortality to the fetus and the newborn. Aspects of vaginal birth after previous CS are discussed in detail in Chapter 23. In terms of prognostication for possible vaginal delivery it is known that women who had a previous normal labour and vaginal delivery either before or after the CS have a better chance of achieving vaginal delivery. It is also reassuring to know that the uterine activity in these women is much lower than in those who had no vaginal delivery, which in some way reassures that the chance of rupture may be less because of less total uterine activity on the scar [52]. Previous labour and delivery reduces the uterine work done to overcome the cervical and pelvic tissue resistance compared with women who had elective CS or CS in the latent phase of labour. When labour is not progressing adequately, oxytocin augmentation is used to increase the uterine activity. The augmented uterine activity is higher than that observed in normal labour. Augmentation improves poor uterine activity and helps to overcome any minor disproportion due to malposition. In the cohort of women with augmented labour, if the labour progresses normally, i.e. 1 cm/h, then the uterine activity is less than those who have a slow or no progress of labour despite augmentation, indicating that it may be wise to consider delivery by CS if the progress of labour is not optimal in the first four hours of augmentation. Those who have satisfactory progress of labour during the first four hours of augmentation are likely to deliver vaginally. Others can be given more time, but with a longer duration of augmented labour with higher levels of uterine activity the risk of scar rupture is likely to increase. Hence careful monitoring of the mother, fetus and labour is needed, with ready recourse to CS in cases where labour is managed with a previous CS; signs of scar rupture may be first noted as abnormalities of the FHR pattern [53,54].
Scar rupture is dependent on (a) the integrity of the scar and (b) the force of uterine activity on the scar, which is dependent on the intensity and duration of uterine contractions. Based on such a hypothesis, quantifying uterine activity at 15 min intervals or cumulative uterine activity calculations should help to predict the possibility of scar rupture, but this has not been found to be the case. One or two strong contractions due to hyper-stimulation in a case with otherwise normal uterine activity may also rupture the scar. Hence the evidence for the use of intrauterine catheters to measure pressures or uterine activity to predict or diagnose scar rupture is not that strong [55,56].
In the intact uterus, the head forms a seal at the cervix and pelvis and the intrauterine pressure builds up with contractions. If the scar gives way then the liquor will leak out and the fetus may also be extruded with early loss of integrity of the scar. This should lead to reduction in the resting uterine pressure or tone. The reduction of the uterine tone and amplitude of contractions or absence of recording contractions should alert to the possibility of scar rupture [57]. The expected reduction of baseline resting pressure or the amplitude may not be affected if the catheter tip lies in a localized well-enclosed pocket of amniotic fluid. The presence of contractions may also be seen in cases of scar dehiscence where the visceral peritoneum is intact and helps to maintain the resting tone and also the build-up of contraction pressure, but these contractions may stretch the dehisced scar and lack of pull on the cervix to make it dilate [58]. Loss of uterine contraction recording with external tocography is common and is due to the loosening of the toco belt or change in position of the mother. Sudden loss of uterine contractions with intrauterine pressure measurement should suggest scar dehiscence unless the catheter has slipped out or has become blocked (with fluid-filled catheters). More often than not, the first sign is the sudden appearance of prolonged deceleration or repeated profound decelerations.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


