Syndrome or association
Characteristics
Holt-Oram
Heart defects, most commonly cardiac septal defects
Thrombocytopenia-absent radius (TAR) syndrome
Thrombocytopenia present at birth (may require transfusions), but improves over time
VACTERL association
Vertebral abnormalities, anal atresia, cardiac abnormalities, tracheoesophageal fistula, esophageal atresia, renal defects, radial dysplasia, lower limb abnormalities
Fanconi anemia
Aplastic anemia not present at birth, develops about 6 years of life
CHARGE syndrome
Coloboma of the eye, heart defects, atresia of the nasal choanae, retardation of growth and/or development, genital and/or urinary abnormalities, and ear abnormalities and deafness

Fig. 1
A 3 year-old child with CHARGE syndrome (Courtesy of Shriners Hospital for Children, Philadelphia)
Failure to make the diagnosis of an associated syndrome will have lifelong repercussions for the child, family, and physician. This consequence is especially evident in children with FA that can be diagnosed with a chromosomal challenge test. Early diagnosis allows for years of preparation to search for an appropriate bone marrow match that may prevent the child from succumbing to aplastic anemia. Innovative techniques, such as PGD (preimplantation genetic determination), allow the parents to have another child without FA, but with matching blood characteristics. Hence, cord blood can be harvested and used as a donor for the affected FA child. Many hand surgeons and pediatricians fail to consider the diagnosis of FA at the time of thumb reconstruction or consultation, leaving the child and their family to suffer the consequences of a painful terminal illness that could otherwise have been treated.
Diagnosis
The diagnosis of thumb deficiency is dependent upon the extent of deficiency and the presence or absence of any associated anomalies. Thumb hypoplasia and profound radial deficiency are usually diagnosed shortly after birth as the forearm is foreshortened and the hand deviated in a radial direction. In addition, florid thumb hypoplasia is recognized early in infancy as there is marked asymmetry between the thumbs. In contrast, mild thumb hypoplasia may go unrecognized for years and not present until adolescence, even if more severe hypoplasia is diagnosed on the contralateral side. This late presentation often is confusing to the patient and disconcerting to the parents. The parents cannot understand how they did not recognize their child’s discrepancy before adolescence and often relate the thumb hypoplasia to remote trauma. Our explanation is quite simple; “as one gets older the activities of daily of life become more complicated, and therefore subtle differences are not recognizable until the child is older.” For example, buttoning, tying, and keyboarding are tasks performed as the child becomes older and are not performed during infancy and early childhood. This explanation obviates any feeling of guilt and allows the family to focus on the treatment to remedy the problem.
Diagnosis is based upon a careful physical examination and corresponding x-rays. The length, girth, motion, and stability are important elements of the examination. The length and girth are usually compared to the contralateral side. The normal thumb length is just proximal to the proximal interphalangeal (PIP) joint of the index finger. X-ray length is approximately 70 % of the length of the adjacent index finger proximal phalanx. The thumb girth and nail width as a percentage of corresponding levels of the index finger girth and nail width are approximately 133 % and 105 %, respectively (Goldfarb et al. 2005). The overall thumb motion is assessed along with movement at the carpometacarpal (CMC), metacarpophalangeal (MCP), and interphalangeal (IP) joints. Similarly, the stability of each of these joints is assessed by clinical examination. Instability of the MCP and/or CMC joints is commonly associated with thumb hypoplasia and directly influences the surgical treatment paradigm. An inventory of present and absent intrinsic and extrinsic muscles is a necessary part of the examination, as this is critical to planning the surgical reconstruction.
Classification/Diagnosis
The classification of thumb hypoplasia truly guides management (Table 2) (Kozin 2010a; Soldado et al. 2013). Type I hypoplasia has minor generalized hypoplasia usually affecting the thenar muscles. As stated previously, this slight degree of hypoplasia may present later in life as the complexities of daily hand function become more intricate and complicated. Type I thumb hypoplasia may or may not warrant treatment depending on the impact on function. Incapacitating lack of opposition requires a tendon transfer to enhance thumb function.
Table 2
Thumb deficiency classification and treatment paradigm
Type | Findings | Treatment |
|---|---|---|
I | Minor generalized hypoplasia | No treatment |
II | Absence of intrinsic thenar muscles | Opponensplasty |
First web space narrowing | First-web release | |
Ulnar collateral ligament (UCL) insufficiency | UCL reconstruction | |
III | Similar findings as type II plus: | A: Reconstruction |
Extrinsic muscle and tendon abnormalities | B: Pollicization | |
Skeletal deficiency | ||
A: Stable CMC joint | ||
B: Unstable CMC joint | ||
IV | “Pouce flottant” or floating thumb | Pollicization |
V | Absence | Pollicization |
Type II hypoplasia has distinct findings that direct treatment (Fig. 2). There is absence of the thenar muscles innervated by the recurrent branch of the median nerve (abductor pollicis brevis, opponens pollicis, and superficial head of the flexor pollicis brevis) (Fig. 2a). The ulnar nerve-innervated deep head of the flexor pollicis brevis is usually present and provides MCP joint flexion. The MCP is often unstable with incompetency of the ulnar collateral ligament (Fig. 2b). The MCP joint can also be globally unstable with incompetency of both the ulnar and radial collateral ligaments. The thumb-index or first web space is narrowed, and the skin is tight (Fig. 2c). The web space can appear less narrow as the unstable MCP joint drifts into valgus during the examination.
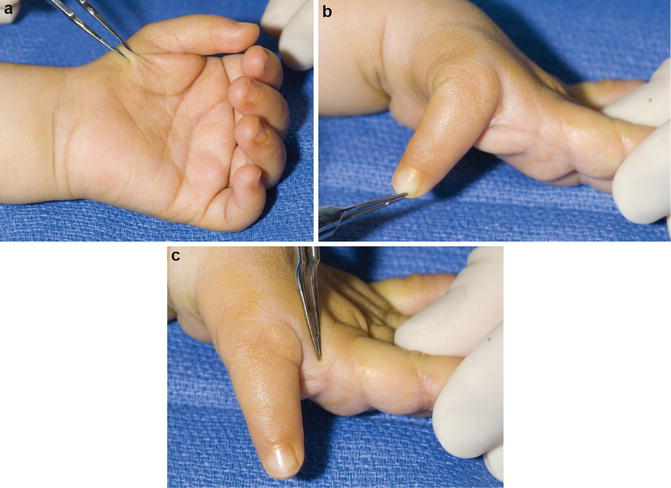
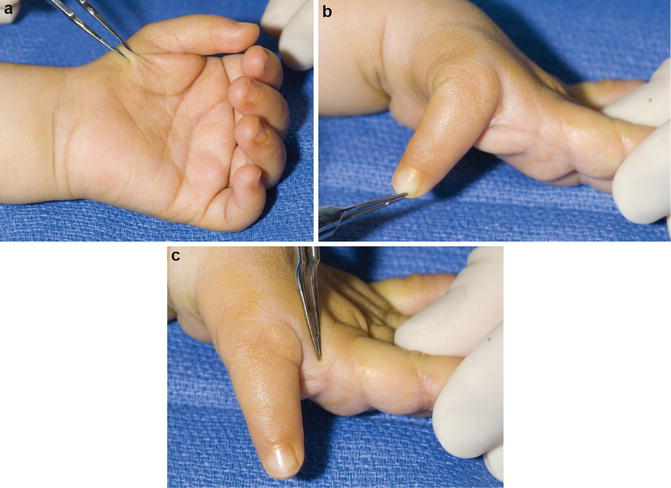
Fig. 2
A 2- year-old with type II left thumb deficiency (Courtesy of Shriners Hospital for Children, Philadelphia). (a) Absent thenar muscles. (b) Ulnar collateral ligament insufficiency. (c) Narrow thumb-index web space
Type III hypoplasia has the same characteristics as type II hypoplasia as well as extrinsic muscle and tendon deficiencies. Absence or hypoplasia of the extrinsic extensors (extensor pollicis longus and extensor pollicis brevis) or flexors (flexor pollicis longus) requires a careful examination of the active movement at the MCP and IP joints. Type III hypoplasia is also subdivided into IIIA and IIIB, which is a critical demarcation in the treatment paradigm. A type IIIA thumb has a stable CMC joint that is worthy of reconstruction and provides a useful prehensile thumb. A type IIIB thumb has an unstable CMC joint that requires ablation and pollicization. The unstable CMC joint precludes reconstruction as the surgery cannot overcome the basal joint instability. A simple explanation to parents is that this effort would be similar to “trying to build a house without a stable foundation.” Multiple valiant surgical attempts to reconstruct the CMC joint have paled in comparison to a successful index finger pollicization with respect to outcome and function (Kozin et al. 1992; Kozin 2012).
Differentiating between a type IIIA (stable) and a type IIIB (unstable) thumb can be difficult in some cases, but crucial to formulating a treatment plan. Because the first metacarpal base and the trapezium ossify around 6 years of age, radiographs are unreliable for evaluation of the CMC joint. In a very unstable CMC joint, the metacarpal base tapers to a point rather than having the typical metaphyseal flare (Fig. 3). However, this plain x-ray finding is inconsistent. Advanced imaging studies, such as ultrasound or MRI, can be helpful to evaluate the integrity of the cartilaginous metacarpal base and the trapezium (Soldado et al. 2013). Repeat examinations, however, may be equally as reliable to detect a thumb unworthy of reconstruction. If the child completely bypasses her or his thumb in favor of scissor pinch, the index finger pronates, and the index-long web space widens, then thumb reconstruction is contraindicated, and index pollicization is preferred.


Fig. 3
X-ray of a 2-year-old revealing a thumb metacarpal that tapers to a point is indicative of an unstable carpometacarpal joint (Courtesy of Shriners Hospital for Children, Philadelphia Unit)
Type IV hypoplasia represents a substantial deficiency known as a “pouce flottant” or floating thumb (Fig. 4). The thumb remnant is attached to the hand solely by its neurovascular bundle and skin. The thumb is floppy and is not incorporated into prehension. Type V is complete absence of the thumb. On occasion, there will be a small nubbin remnant present. Scissor pinching is performed between the index and long finger.


Fig. 4
A 1 year-old with severe type IV thumb hypoplasia (pouce flottant or floating thumb) (Courtesy of Shriners Hospital for Children, Philadelphia Unit)
Thumb hypoplasia can also be found in children with ulnar deficiency. A similar treatment paradigm is applied. Pollicization is indicated for marked thumb hypoplasia. The surgical technique is similar with minor modifications, such as skin design.
The standard surgical indications for pollicization can be expanded to include a thumb smaller than a small finger (Kozin 2012). Reconstruction of a small hypoplastic thumb even with a stable CMC joint will not function like pollicization of a mobile index finger (Foucher et al. 2001). This decision requires a “heart to heart” conversation with the parents. Parents usually come to appreciate that “function trumps form” and that thumb ablation and index pollicization will result in enhanced function versus reconstruction of a small scrawny thumb. When in doubt, parents are offered the opportunity to discuss their decision with other parents who have made a similar difficult decision.
Treatment
There is little role for nonoperative management of the hypoplastic thumb. An experienced therapist evaluation, however, is invaluable. Their input can be helpful by providing support for the family and facilitating the decision-making process. On occasion, preoperative fabrication of a thumb spica splint may stabilize an unstable MCP joint. Following surgery, the therapist’s role escalates to act as a primary provider of care that directly impacts the success of the procedure (Tables 3 and 4).
Table 3
Thumb hypoplasia: Nonoperative management
Indications | Contraindications |
|---|---|
Few indications | None |
Unstable joints | |
Determining the degree of thumb hypoplasia and prehensile pattern of the child |
Table 4
Thumb hypoplasia: Physical/occupational therapy recommendations
Assessment of thumb hypoplasia and thumb usage during prehension |
Thumb spica splint |
Education of parents |
Participate in the decision-making process |
The classification schema guides treatment. Type I hypoplasia usually does not warrant surgical intervention. Type II and IIIA hypoplasia often requires surgery to provide stability, improve motion, and enhance function. Type IV and V hypoplasia requires index finger pollicization as long as the index is “fit” to be a thumb. A stiff index finger will make a stiff thumb that may not improve hand function. Therefore, the risk/benefit ratio requires calculation and consideration. The operation should follow the Peter Carter 2–4 rule. In other words, for some children surgery can indeed be done “to” them, but it may not necessarily be “for” them.
Thumb Reconstruction
Thumb reconstruction for type II and IIA hypoplasia requires addressing all the elements that are deficient. The narrowed thumb-index web space, MCP instability, and thenar muscle absence all require treatment. Thumb-index web space narrowing is treated with skin rearrangement and soft tissue release. A four-flap Z-plasty lengthens the tight skin and provides a rounded contour to the web space. The deeper soft tissue release includes the investing fascia around the adductor pollicis. The princeps pollicis artery and its branches must be identified and protected before division of the fascia. An extremely tight web space may also require partial release of the adductor muscle and/or first dorsal interosseous muscle.
MCP instability requires stabilization. Unidirectional instability with an incompetent ulnar collateral ligament is the most common finding. Ligament reconstruction can be performed with the residual length of donor tendon from the opposition transfer. Bidirectional or global instability is more difficult to manage. Reconstruction of both the radial and ulnar collateral ligaments with tendon graft has been described. MCP joint chondrodesis is preferred to achieve firm stability and provide a stable fulcrum for the opposition transfer to function. The details of this procedure are covered in chapter “Arthrogryposis.” UCL insufficiency can be secondary to an anomalous connection between the flexor pollicis longus and extensor pollicis longus muscles (a.k.a. pollex abductus) (Tupper 1969; Fitch et al. 1984; Lister 1991). This pollex abductus attenuates the UCL over time and prevents active interphalangeal joint motion. Surgery must release the pollex abductus at the time of UCL reconstruction.
Thenar absence requires a tendon transfer to provide thumb opposition. There are a variety of donor muscle-tendon units to choose from including flexor digitorum superficialis (long or ring), abductor digiti minimi , extensor carpi ulnaris, and extensor indicis proprius. Each donor muscle-tendon unit has its advocates, advantages, and disadvantages. The long or ring finger flexor digitorum superficialis (FDS) is preferred secondary to its length, technical ease, power, expendability, and synergism. If the FDS is unavailable, the other donor options are considered.
Technique: Flexor Digitorum Superficialis Opponensplasty with UCL Reconstruction (Opposition and UCL Reconstruction Video)
The patient is placed supine on the operating room table (Video 1). The procedure is usually performed under general anesthesia. A single dose of intravenous preoperative antibiotics is administered. The limb is prepped and draped in sterile fashion. Chlorhexidine gluconate and alcohol prep (ChloraPrep; CareFusion, Leawood, Kansas, USA) is preferred, which may be more effective in eliminating bacteria and avoids iodine that can migrate beneath the tourniquet and cause burns (Saltzman et al. 2009; Table 5)

Table 5
Thumb reconstruction: Preoperative planning
OR table: regular |
Position/positioning aids: supine |
Fluoroscopy location: ipsilateral |
Equipment: standard, drill, K-wires |
Tourniquet: sterile |

Video 1
Opposition and UCL Reconstruction
The limb is exsanguinated and the tourniquet is inflated. The incisions are carefully drawn (Fig. 5). The narrowed thumb-index web space is widened via a four-flap Z-plasty. Each limb of the Z-plasty should be equal in length except for the radial limb that is extended in a proximal direction to expose the UCL and the MCP joint. The ring finger FDS tendon is isolated at the base of finger and in the distal forearm. A short oblique incision is made at the base of the ring finger, and a zigzag or oblique incision is performed along ulnar portion of volar forearm. The flexor carpi ulnaris (FCU) tendon is also isolated. An additional skin incision is made along the radial side of the thumb MCP joint to expose the eventual site for FDS tendon attachment. The ring finger FDS tendon is identified in at the base of the finger and separated from the flexor digitorum profundus (FDP) tendon. The FDS tendon is also isolated in the forearm (Fig. 6). The FDS tendon is tagged with a suture and cut at the base of the ring finger while protecting the underlying FDP tendon. An Allis tissue forceps (Jarit, Hawthorne, NY) is placed around the ring FDS tendon in the forearm and used to roll the tendon through the carpal tunnel and into the forearm (Fig. 7). Failure of the FDS tendon to roll into the forearm requires assessment for FDP-FDS attachments and/or division of Camper’s chiasm.


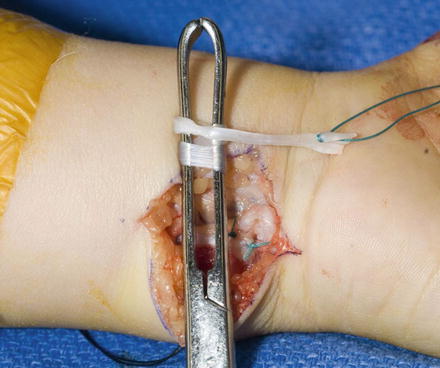

Fig. 5
Four-flap Z-plasty to widen the narrowed thumb-index web space (Courtesy of Shriners Hospital for Children, Philadelphia)

Fig. 6
Ring finger FDS tendon is identified in at the base of the finger and within the forearm (Courtesy of Shriners Hospital for Children, Philadelphia)
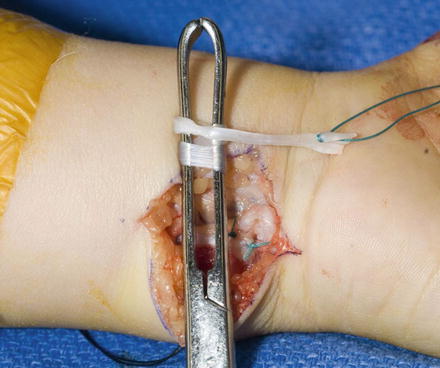
Fig. 7
Ring finger flexor digitorum superficialis tendon rolled into volar forearm incision (Courtesy of Shriners Hospital for Children, Philadelphia)
A loop of FCU tendon is used to construct a pulley for the FDS tendon. The distal 2–3 cm of FCU tendon is isolated. The radial one-half of the FCU tendon is harvested preserving its distal attachment to the pisiform (Fig. 8). The radial one-half of the tendon is passed through the retained FCU at the pisiform to fashion a loop. The radial one-half of the tendon is sutured to the retained FCU at the pisiform. The ring finger FDS tendon is passed through the FCU loop in preparation of transfer (Fig. 9).
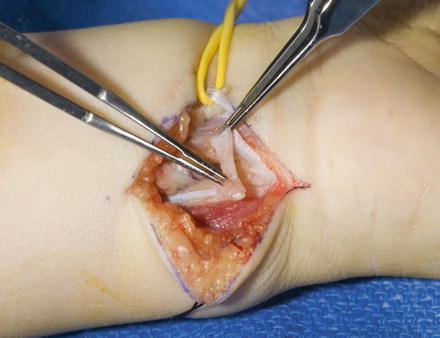
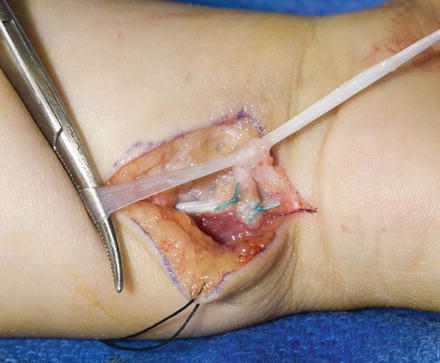
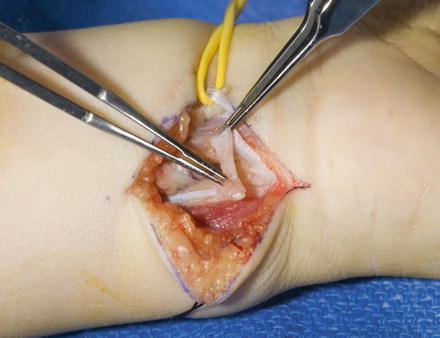
Fig. 8
One-half of the distal 2–3 cm FCU tendon is used to construct a pulley for the FDS tendon (Courtesy of Shriners Hospital for Children, Philadelphia)
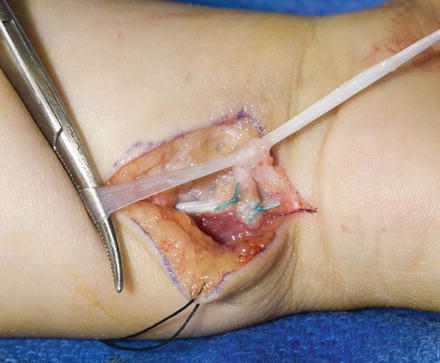
Fig. 9
Ring finger FDS tendon is passed through the FCU loop (Courtesy of Shriners Hospital for Children, Philadelphia)
A subcutaneous tunnel is made between the radial side of the thumb and the volar forearm incision for passage of the ring finger FDS tendon. The FDS tendon is passed through the FCU loop under the skin to the radial side of the thumb (Fig. 10). The metacarpal head is isolated and a 0.45″ Kirschner wire drilled across the metacarpal head parallel to the joint surface (Fig. 11). Mini-fluoroscopy is used to ensure appropriate Kirschner wire position. The wire is directed from the volar aspect of the radial side of metacarpal to the ulnar and dorsal aspect. The hole is enlarged with a drill bit to allow passage of the FDS tendon. The MCP joint is reduced and stabilized with a longitudinal 0.045″ Kirschner wire drilled antegrade from the tip of the thumb across the MCP joint. The wire is cut short and a Jurgan Pin Ball (RFO Medical Company, London, UK) applied. The FDS tendon is passed through the drill hole to the ulnar side of the thumb for ligament reconstruction (Fig. 12). If the tendon is too large in diameter, one FDS slip can be removed.




