6 Polycystic ovary syndrome
Understanding Pcos
What is polycystic ovary syndrome (PCOS)?
Stein and Leventhal first described PCOS in 1935 as a symptom complex associated with anovulation. It was said to be present in women who had oligomenorrhoea, hirsutism and obesity, together with a demonstration of enlarged polycystic ovaries. More recently, a consensus definition for PCOS has been reached (Box 6.1).1
BOX 6.1 The Rotterdam Consensus Group criteria for the definition of polycystic ovary syndrome
(From Rotterdam ESHRE/ASRM-sponsored POCS Consensus workshop group1)
The diagnosis of PCOS requires that at least two of the following three criteria are met:
Other conditions can also be present as part of PCOS, but these are not among the diagnostic criteria; they include obesity, insulin resistance, impaired glucose tolerance and type 2 diabetes mellitus, dyslipidaemia, cardiovascular disease, obstructive sleep apnoea and infertility.2
How many women have polycystic ovaries?
As many GPs practising in women’s health know, the ultrasonographic description of polycystic ovaries is commonly found in asymptomatic women. In fact, studies have found that approximately 25% of normal women demonstrate the classic features of polycystic ovaries described in Box 6.2. A ‘necklace-like’ appearance or ‘string-of-pearls’ pattern of follicular cysts is said to be ‘typical’ of polycystic ovaries.3,4 These findings have become even more common with the use of high-resolution transvaginal ultrasounds. Around 14% of women on oral contraceptive pills have also been found to have polycystic ovaries.4
How many women have polycystic ovary syndrome?
General estimates for the prevalence of PCOS based on old definitions range between 5% and 10% in women of reproductive age.5,6 Estimates using the Rotterdam Consensus definitions indicate that the prevalence is as high as 20–25%, although symptoms are often mild7 and about 20% of women with polycystic ovaries have no symptoms.8 Another way of viewing the prevalence is that 70–90% of women with oligomenorrhoea or anovulation have PCOS.9
How does PCOS come about?
PCOS is a heterogeneous condition, with both genetic and environmental factors influencing its development. The familial nature of PCOS is well established,10 with about 35% of mothers and 40% of sisters of PCOS patients affected by the disorder.11
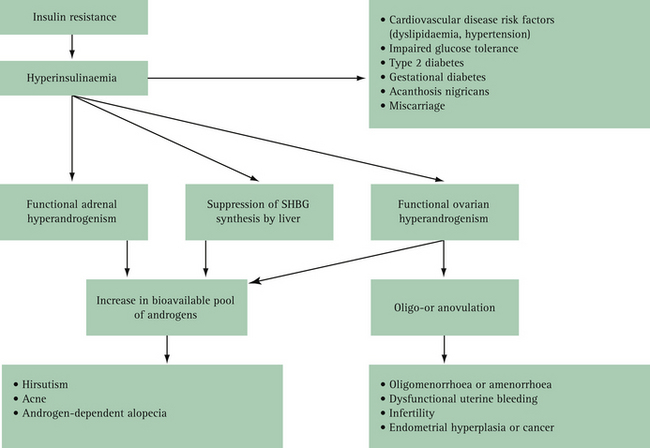
Over time, focus on causation of PCOS has shifted from the ovary to the hypothalamic–pituitary axis and then to some primary defects of insulin activity as the primary pathological cause of the syndrome. Insulin resistance is a key pathophysiological feature of PCOS,12 and the association between increased insulin resistance and PCOS is a consistent finding in all ethnic groups.13 Insulin resistance results in hyperinsulinaemia, functional adrenal hyperandrogenism, suppression of serum human binding globulin (SHBG) synthesis by the liver and functional ovarian hyperandrogenism14 (Fig 6.1), which in turn give rise to symptoms such as hirsutism, acne and oligomenorrhoea. More serious sequelae include infertility, impaired glucose tolerance, a fourfold to sevenfold increase risk of diabetes and a potentially increased risk of cardiovascular disease.15 However, insulin resistance is seen in only 10–15% of slim women and 20–40% of obese women with PCOS,16 so clearly work remains to be done in clarifying the aetiology and nature of this puzzling condition.
The proportion of overweight and obese women with PCOS appears to be the same as in the general population.17 While obesity does not cause PCOS, weight gain is an important contributor (both genetic and environmental) to phenotype in many women with PCOS and may be enough to unmask the condition, which may otherwise have remained asymptomatic. Indeed, obesity increases the degree of insulin resistance typically found in PCOS women;18 thus, obese women often have more severe hormonal and metabolic abnormalities.19 As obesity in the community increases, the prevalence of the PCOS phenotype and its associated glucose intolerance — including diabetes — are expected to rise significantly.20
What are the manifestations of PCOS?
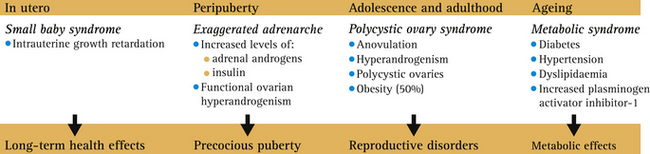
The clinical manifestations of PCOS (shown in Box 6.2, see p 120) affect all ages, ranging from childhood (premature puberty) to the teenage years (hirsutism, menstrual abnormalities), early adulthood and middle life (infertility, glucose intolerance), and later life (diabetes mellitus and cardiovascular disease) (Fig 6.2).21 PCOS is the most common cause of anovulatory infertility and hirsutism.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree