Anterior asynclitism: more parietal bone and the sagittal suture in the anterior half of the pelvis.

The newborn’s head showing the larger suboccipito-bregmatic diameter well above the position of the ear.
The IVD should be carried out in a room with adequate facilities and personnel. The procedure should be carried out under adequate antiseptic and aseptic conditions. There is inadequate evidence to recommend antibiotic prophylaxis [22]. The clinician should have the competence to perform the procedure, be capable of managing any complications and be prepared to abandon the procedure and carry out a CS. The CS in such situations is fraught with difficulties and complications and hence the help of an experienced clinician may become necessary. Compressive and traction forces on the head due to the application of an instrument may give rise to prolonged decelerations, and should there be difficulties in delivery with a prolonged period of traction it may be best to abandon the procedure and carry out a CS. To identify the fetal condition, intermittent or continuous fetal heart rate (FHR) monitoring is recommended. Difficulty or failure are likely to arise when the head is one-fifth or more palpable on abdominal examination, the presenting part is at or above the level of spines, there is occipito-posterior position, excessive moulding of the fetal head, fetal macrosomia, dysfunctional or prolonged labour and body mass index >30 kg/m2 [23]. In such cases, a trial of IVD should be performed in the operating theatre under effective epidural or spinal anaesthesia, with facilities and personnel available for CS. Such an eventuality should have been mentioned to the mother and her partner and appropriate consent taken.
Vacuum-assisted Deliveries
The vacuum extractor is a device with a suction cup attached with tubing to a vacuum source and a handle, which is used to apply traction to the cup. Traction is applied to the fetal head along the axis of the birth canal. Malmström devised the stainless steel vacuum cup in the 1950s. It has rounded edges and a diameter of 60 mm, with the vacuum tubing and the traction chain attached to the centre of the upper surface of the cup. Bird modified the Malmström vacuum extractor by attaching the vacuum tubing and the traction chain on the side of the cup. This allows the placement of the cup close and anterior to the occiput in occipito-posterior and lateral positions. Kobayashi introduced a single unit silastic cup with a diameter of 65 mm and a stainless steel valve that allows the release of suction between contractions without loss of application of the cup to the head (Figure 9.3a). Kiwi Omnicup (Clinical Innovations Inc., Murray, Utah) is a disposable vacuum extractor with a rigid flat plastic cup and a hand-pump traction system directly applied to the vacuum cup (Figure 9.3b). The accurate development of negative pressure can be monitored via an indication gauge on the traction handle. Randomized studies [24] suggest that rigid cups are more likely to result in vaginal birth than soft cups, but they are more likely to cause scalp trauma.
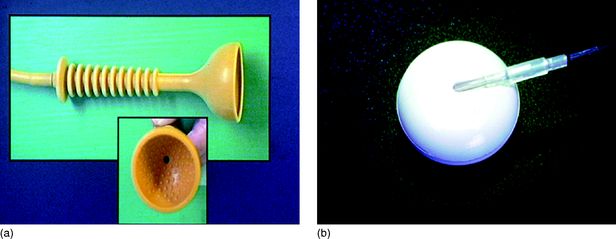
(a) Silk cup; (b) Kiwi™ posterior cup (Omnicup) showing the tubing used for creating suction and also used for traction, going through a groove to the centre of the cup.
The parturient should be in lithotomy position with adequate analgesia. Prior to cup placement, the fetal presentation, the amount of fetal head in ‘fifths’ palpable abdominally above the symphysis pubis, the position of the fetal head and the station should be confirmed. Correct placement of the cup is a major determinant of the outcome. The ‘flexion point’ is the site on the fetal scalp over which the centre of the vacuum cup should be placed to achieve a flexing median application. Flexion point is on the sagittal suture 3 cm anterior to the posterior fontanelle (Figure 9.4). Application of the vacuum cup on this point promotes synclitism and flexion of the fetal head, presenting the optimal diameter of the fetal head (suboccipito-bregmatic, 9.5 cm) to the maternal pelvis. By incorrect application of the vacuum cup (deflexing and paramedian, Figure 9.5), the fetal head will present with a larger diameter that will increase the difficulty and risk of failure or fetal injury [25,26]. In occipito-lateral or posterior positions, a vacuum cup with the tubing emerging from the lateral aspect (posterior metal cup) or through a groove in the cup (posterior rigid plastic cup – Omnicup) (Figure 9.3b) should be used, as it can be inserted between the vaginal wall and the head to reach the flexion point. Soft silk, plastic or anterior metal cups, where the tubing is attached in the centre of the cup, are not suitable for occipito-posterior or lateral positions as the lateral vaginal wall would not permit a cup with the central stem or suction tubing on the dorsum to be shifted to the flexion point. These cups are suitable for occipito-anterior positions as the flexion point is directly accessible.
The flexion point about 3 cm anterior to the posterior fontanelle along the sagittal suture.
After the application of the cup to the fetal head and before inducing negative pressure, any maternal tissue entrapment between the cup and the fetal head should be excluded. Apart from causing significant vaginal or cervical trauma and maternal haemorrhage, entrapment of maternal tissue may cause detachment of the cup and failure of the procedure. Detachment of the cup is associated with increased incidence of cranial fractures (9.58%; RR 2.11) cephalhaematoma (18.56%; RR 1.86) and scalp oedema (26.34%; RR 1.41) [14].
(a) Flexing median application of the vacuum cup (correct application). (b–d) Various malapplications of the vacuum cup: (b) flexing paramedian; (c) deflexing median; (d) deflexing paramedian.
The vacuum is created by mechanical, electrical or a hand pump and the cup is held in place by atmospheric pressure acting on the dorsum of the cup. Hence the maximum pressure that can be created is less than 760 mmHg. In the past it was thought that the formation of chignon, i.e. the soft tissue sucked into the cup, was important for traction and suction was created in a gradual stepwise manner. Based on studies it is known that quick development of negative pressure is as effective as the gradual stepwise process [27]. Effective traction usually requires a negative pressure of at least 0.6 kg/cm2 (440 mmHg) and usually 0.8 kg/cm2 (588 mmHg). Higher pressures are associated with increased risk of fetal head injury. The traction force indicators of the vacuum devices should be checked throughout the delivery as attention to the force and duration may help to reduce the incidence of fetal injuries [28]. Traction should be in line with the axis of the pelvis, and ideally it should be perpendicular to the plane of the vacuum cup. Each effort at traction should be with uterine contractions and coordinated with maternal expulsive efforts. Descent must be observed with the initial and subsequent traction efforts. The initial lengthening of the traction tube in an occiptio-posterior and lateral position signifies that the first traction has resulted in flexion of the head, resulting in the flexion point coming as the leading part of the presentation. This should result in progressive descent with successive traction efforts. If the cup is dislodged, the reason for the ‘pop-off’ should be evaluated, and if there are no contraindications it can be reapplied after careful inspection of the fetal scalp for injury. There is no consensus on the maximum number of traction attempts, the duration of a vacuum application or the number of ‘pop-offs’ that should be allowed. Vacca suggests that the traction force should not exceed 11.5 kg, the duration of the procedure should be restricted to 15 min and the number of pulls limited to three for the descent phase and three for the perineal phase [29]. A traction force exceeding 13.5 kg is associated with an increased risk of fetal scalp injury [29]. Higher levels of traction force and a greater number of pulls may, however, be required during the outlet phase of the vacuum delivery as resistance is greatest at this stage. For this reason, additional time and pulls should be allowed for the perineum to stretch over the head, especially if the birth is managed without episiotomy [29]. The ‘pop-offs’ are due to change in direction of the pull to upwards before the maximum biparietal diameter emerges from underneath the sub-pubic arch, large caput underneath the pubic arch acting as a ‘door stopper’ or sudden excess force due to the belief that the head is just going to come out on seeing the portion of the head that may be the scalp and not the bony skull.
The traction force is less when the head descends with the cup during traction compared with a situation when the head does not descend with traction. Hence additional pulls with descent are less likely to be harmful compared with traction on a head that does not descend with three pulls. The RCOG guidelines recommend that ‘operative vaginal delivery should be abandoned where there is no evidence of progressive descent with each pull or where delivery is not imminent following three pulls of a correctly applied instrument by an experienced operator’ [1]. The SOGC guidelines advise that if delivery has not occurred after four contractions the intended method of delivery should be reassessed [5]. With efficient uterine contractions and good maternal expulsive efforts, almost all vacuum-assisted deliveries should be completed within 15 min. If a 20 min limit is exceeded, the procedure should be abandoned unless delivery is imminent [16]. The procedure should also be abandoned if there is evidence of fetal scalp trauma.
Forceps Deliveries
Forceps are a paired instrument with a handle, shank, lock and blade. The blades have a cephalic and a pelvic curve between the heel and toes (at the distal end) and are attached to each other by a lock on the shank. Forceps are used for traction of the fetal head. Specially made forceps that allow sliding of one shank over the other and with minimal pelvic curve, i.e. Kielland’s forceps, can be used for correction of asynclitism and rotation of the head followed by traction. The Barton’s forceps are used for transverse arrest in a flat pelvis and the Piper’s forceps with long shanks for the delivery of the after-coming head in breech presentations.
The mechanism of action of forceps includes correction of deflexion, asynclitism or positional abnormalities of the fetal head, extraction by working in synchrony with the maternal expulsive forces and transient reduction of the resistance of the outlet by enlargement of the soft tissue of the birth canal. The cephalic curve grasps the fetal head over the maxilla or malar eminences, while the length of the blade grasps the sides of the head from the malar area along the side of the head in front of the ear and the parietal bones in front of the occiput (Figure 9.6). This bimalar–biparietal application exerts uniform pressure on the head. In this position the shank is over the flexion point, allowing the correct direction of traction.

Bimalar–biparietal application of the forceps which when checked before traction will allow one finger between the head and heel of the blade on either side, the sagittal suture would be perpendicular to the shank and the occiput would be 3 cm above the shank, allowing the traction on a flexed head with the line of pull along the flexion point.
The choice of forceps depends on the indication, clinical situation and preferences of the obstetrician, as well as the availability of instruments. For occipito-anterior positions in the mid- or low-cavity or low-direct occipito-posterior positions, the Neville–Barnes with or without axis traction handle or the Simpson’s forceps can be used. Wrigley’s forceps are ideal for outlet deliveries. If the position is occipito-lateral or posterior, Kielland’s forceps can achieve rotation without inflicting trauma to the fetus or the maternal passages. Non-fenestrated blades are indicated in cases with oedematous soft maternal tissues to minimize risk of tearing. Face presentation with mento-anterior position can be delivered using Kielland’s or Simpson’s forceps.
Proper application of the forceps to the fetal head is extremely important for a safe procedure with a successful outcome. The exact location of the sagittal suture and posterior fontanelle should be ascertained. The arrangement of the blades should be rehearsed prior to insertion. The forceps blades should be applied gently between contractions. The left blade is applied first to the left side of the maternal pelvis using the left hand, while the right hand guides and protects the head and the vagina. The right blade is applied to the right side of the maternal pelvis using the right hand. No force should be required. If there is resistance the blade should be removed and reapplied. The blades are correctly placed when they are situated in the spaces between the fetal orbits and ears and this will be reflected by the shanks and handles being horizontal and there being easy locking of the blades. When the blades are locked and prior to applying traction, the obstetrician should confirm correct application by ensuring that the sagittal suture is symmetrically and perpendicularly in the midline between the two shanks, the occiput is 3–4 cm above the shanks (so that the traction line is along the flexion point, thus promoting flexion and exposing the minimal diameter) and the space between the heel of the blade and the head does not admit more than a finger breadth (ensures synclitism).
Analgesia before forceps delivery includes pudendal nerve block, spinal analgesia, diazepam, and ketamine or vinydan ether. The available evidence shows that none of these agents or methods is superior to the others [30].
Once the forceps have been applied and the position of the blades checked, traction should be coordinated with uterine contractions and maternal bearing down efforts. The axis of the traction forces should follow the pelvic curve (curve of Carus). The traction is initially downward and as the head descends in the birth canal, the angle moves forward and upward at the outlet. The Pajot manoeuvre involves the combined exertion of outward and downward forces, which produce a vector that follows the pelvic curve. Traction should be released between contractions in order to reduce the intracranial pressure and the associated vagally induced bradycardia. An episiotomy is usually indicated when the head is crowning at the perineum.
Delivery in Malposition of the Fetal Head
Malpositions of occipito-transverse or -posterior position may be associated with some degree of extension of the head and asynclitism. One needs to carefully consider whether to use digital or manual rotation or rotational forceps delivery, ventouse delivery or CS. If the head is rotating and descending with uterine contractions and bearing down efforts, it may be possible to keep a finger on the suture line and assist, i.e. digital rotation. Alternatively the whole hand can be used to assist with manual rotation. In a digital rotation the index and middle fingers are placed onto the part of the anterior parietal bone that overlaps the occipital bone in the area of the posterior fontanelle and gentle pressure is applied with the tips of the fingers to rotate the posterior fontanelle upward and toward the symphysis pubis. In a manual rotation, the hand under the posterior parietal bone and the thumb on the anterior parietal bone applies rotational pressure (Figure 9.7) [31].
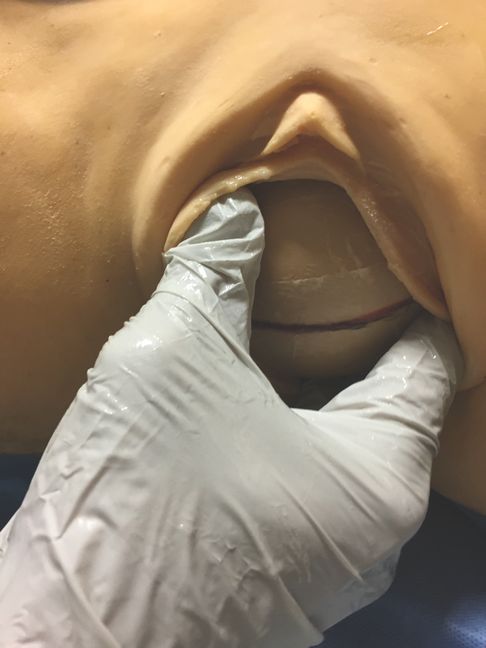
Manual rotation of the fetal head from left occipito-transverse to occipito-anterior position.
For mid-cavity or rotational assisted vaginal birth it is recommended that a skilled operator be present for all attempts [15]. Insufficient training is likely to result in poor outcomes [32]. Correction of asynclitism and auto-rotation is expected with traction and descent of the head with a ventouse delivery if the cup was placed over the flexion point. Twisting or rotational motions of the vacuum cup may result in injury. The auto-rotation occurs as the head descends by virtue of the anatomy of the pelvis. Rotation of the fetal head can be attempted using special rotational forceps (Kielland’s). Before Kielland’s forceps are used, it is essential to identify abdominally the side of the baby’s back and the occiput on vaginal examination. The forceps are applied with the ‘knobs’ facing towards the baby’s occiput. The anterior or posterior blade may be applied first directly depending on the preference of the obstetrician. The anterior blade can be positioned by direct, reverse or classical and wandering method. In the wandering method the anterior blade is placed over the face and then moved to lie on the side of the fetal head. The posterior blade can be applied directly. The blades are locked and asynclitism corrected by sliding the shanks on each other until the sliding locks come to the same level. If there is no asynclitism the sagittal suture of the fetus will lie equidistant from the two blades of the forceps. If the blades cannot be locked easily, their position should be checked and they should be removed and reinserted.
An abnormal position (e.g. occipito-transverse) is corrected by rotating the handles of the forceps blades and directing the fetal occiput to the anterior position to emerge underneath the symphysis pubis. The risk of injury can be minimized by avoiding excessive torsion during rotation, rotation in the wrong direction, forceful rotation or combined rotation with traction. In a rotational delivery the movements of traction and rotation should always be separate unless rotation occurs spontaneously with traction. Rotation should be avoided during a uterine contraction [33].
Complications
Maternal Injuries
Vaginal, cervical, labial, periurethral lacerations, pelvic haematomas, perineal injuries, episiotomy extension and the associated haemorrhage are the most common complications. Severe maternal morbidity is increased after operative vaginal deliveries [34] and maternal deaths from traumatic operative delivery have been reported [17].
Maternal injury is less frequent and less extensive with the use of vacuum compared to forceps [8,35,36]. Maternal complications of vacuum delivery include cervical lacerations, severe vaginal lacerations, periurethral lacerations, vaginal haematomas, and third- and fourth-degree tears [8]. The use of forceps has been associated with a higher rate of episiotomies and third- and fourth-degree perineal and vaginal tears [37].
The most common vaginal lacerations are the posterior midline tears or the anterior periurethral tears. Inadvertent entrapment of the cervix or the vaginal wall with consequent lacerations can occur during an operative delivery. Posterior tears should be repaired if they involve more than the vaginal mucosa. Anterior labial and periurethral tears do not usually require repair unless they are bleeding. Injury to the bladder or the urethra may cause urinary retention secondary to oedema or haematoma and late fistula formation. The first volume of urine passed should be checked and the residual urine measured if the bladder is palpable or there was difficulty in voiding. Insertion of a Foley catheter is advisable if the tear is close to the urethra. Vaginal lacerations may extend into the ischiorectal fossae.
A third- or fourth-degree perineal tear with anal sphincter injury is a potentially severe complication of vaginal delivery, which may result in anal incontinence and rectovaginal fistula formation. A third-degree perineal tear and altered faecal continence occurs more frequently after forceps than vacuum deliveries [38] and in occipito-posterior positions [39,40]. The incidence of third- or fourth-degree perineal tears with forceps-assisted delivery can be as high as 31% and 17% with the use of vacuum, respectively. This rate is significantly higher than at an unassisted delivery [36]. However, normal vaginal delivery without evidence of sphincter injury is also associated with significant effect on anal sphincter function [41]. Anal incontinence can occur regardless of the mode of delivery [42].
Trauma to the pelvic floor musculature and its innervation as a result of forceps and vacuum delivery may contribute to the occurrence of urinary incontinence [43]. Arya et al. found that in primiparous women, urinary incontinence after forceps delivery is more likely to persist compared with spontaneous vaginal or vacuum delivery [44]. Liebling et al. studied the symptoms of pelvic floor morbidity after difficult operative vaginal deliveries and CSs during the second stage of labour, and concluded that although a CS does not completely protect women from pelvic floor morbidity, operative vaginal delivery was associated with a greater prevalence of urinary symptoms and dyspareunia for up to a year after delivery [45].
Psychological morbidity following IVD is also of concern. Instrumental vaginal delivery can be associated with fear of subsequent childbirth, which may present as a post-traumatic stress type syndrome termed ‘tokophobia’. Midwife-led debriefing after assisted vaginal birth did not reduce maternal depression [46]. After delivery the obstetrician that conducted the birth should discuss the indications and complications of operative delivery with the woman if anxieties and fear of the next childbirth are to be alleviated [47].
Fetal Injuries
Scalp Bruises and Lacerations
Fetal scalp injuries occur in most operative vaginal deliveries. They are usually transient and of no clinical significance. The more significant injuries are related to incorrect application of the instrument, excessive or incorrectly directed traction or cephalo-pelvic disproportion.
During application of the vacuum cup to the fetal head a collection of interstitial fluid and microhaemorrhages (chignon) fill the internal diameter of the vacuum cup. This is less pronounced when using soft cups, and resolves within 12–18 hours. The incidence of scalp abrasions and lacerations after vacuum extraction is 10%. The incidence of scalp abrasions is higher in infants delivered by Kiwi Omnicup vacuum or metal cup devices compared to those delivered by silastic cup [48]. Correct cup placement and traction, and avoidance of cup detachments (‘pop-offs’) reduce the risk of scalp injuries [16].
Cephalhaematoma
Cephalhaematoma is secondary to rupture of blood vessels between the skull and the periosteum. It is delineated by the suture lines and thus can be differentiated from subgaleal haemorrhage. As the capacity of the subperiosteal space is limited, these haematomas are small. Cephalhaematoma occurs in 1–2% of spontaneous vaginal deliveries, in 6–10% of vacuum extractions (range 1–26%) [8,14,24,25] and in 4% of forceps deliveries [8]. Vacuum extraction therefore has a stronger association with cephalhaematoma compared with forceps (odds ratio: 2.38) [8]. Metal cups are more likely to cause cephalhaematoma than silastic cups or the Omnicup [49]. Vacuum extractions at mid or low station are associated with a higher incidence of cephalhaematoma (13.11% and 13.56% respectively) when compared with vacuum applied at the outlet (6.81%; RR 1.92; RR 1.99) [14].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


